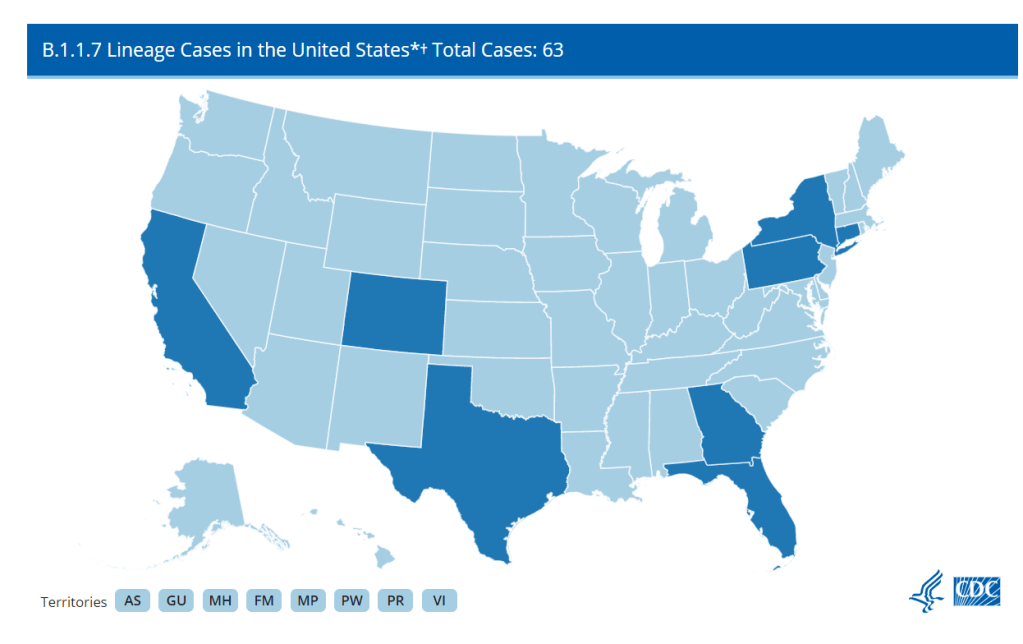
A new, more transmissible strain of COVID-19 (known as B.1.1.7) has caused quite a stir these past few weeks. It surfaced in the United Kingdom and has been detected in eight states: California, Colorado, Connecticut, Florida, Georgia, New York, Texas, and Pennsylvania. The fact that a mutant strain happened isn’t a surprise, as RNA viruses mutate quite often. But as vaccines roll out, the spread of a new strain is yet another reminder that we’re nowhere near out of the woods yet.
It’s entirely possible to differentiate between strains of SARS-CoV-2 through genetic testing. To detect the B.1.1.7 variant, COVID-19 positive samples can be sequenced to search for a telltale deletion in the virus’s RNA. And in theory, we could track the spread of this variant with good testing data. A truly robust tracking effort should include a centralized surveillance program to sequence the RNA of the SARS-CoV-2 virus in all positive cases—or at least a good sample—to detect any mutant strains and track their impact. However, this is an area where the US has consistently faltered: as of December 23rd, only 51,212 out of 18 million positive cases had been sequenced.
As with most of the government’s response, handling this seems to be mostly up to the states. According to releases from Colorado, Pennsylvania, Connecticut, and Texas, it looks like these states are making sequencing efforts. Georgia said, “The variant was discovered during analysis of a specimen sent by a pharmacy in Georgia to a commercial lab”, which I can only assume means they have been conducting some kind of sequencing effort. I couldn’t find references to the extent of sequencing efforts in the announcements from California, Florida, or New York.
From these releases, it’s obvious that there is no unified cross-state effort. Pennsylvania stated that they had been sending “10-35 random samples biweekly to the CDC since November to study sequencing,” but that’s not going to be nearly enough to track this more transmissible variant. Are there any plans to ramp up sequencing? And that’s just from Pennsylvania because they deigned to tell us—are all states going to ramp up sequencing? It’s just not clear.
And after all that, starting to test for the variant now still won’t tell us just how widespread it is. The first case in New York was in someone with no evident travel history. Indeed, this is true for most people who have been infected, and, per Dr. Angela Rasmussen in Buzzfeed News, this suggests that the variant is already circulating in the community. To know how widespread the variant is, we would need to retroactively test samples that had already tested positive. Colorado’s press release mentioned that they would be doing some retroactive testing, but what about the other seven states?
Plus, that’s just states with already confirmed cases—there absolutely will be more confirmed cases in other states, because if it is already present in the community, there probably already are cases in other states. To know just where this variant is, every positive test in the US stretching back months into the past would have to be retroactively re-tested for the variant—an unlikely occurrence.
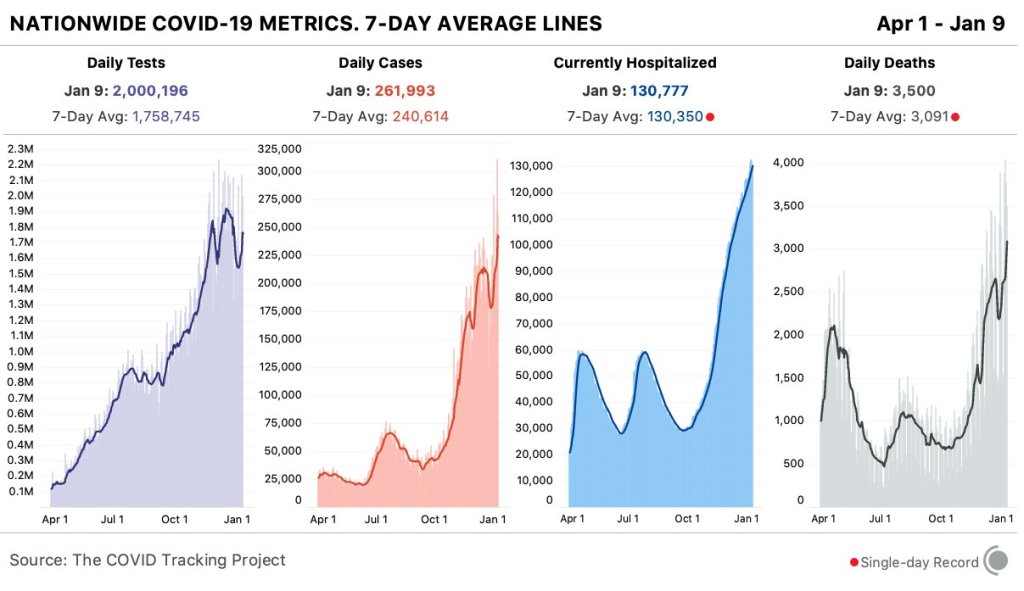
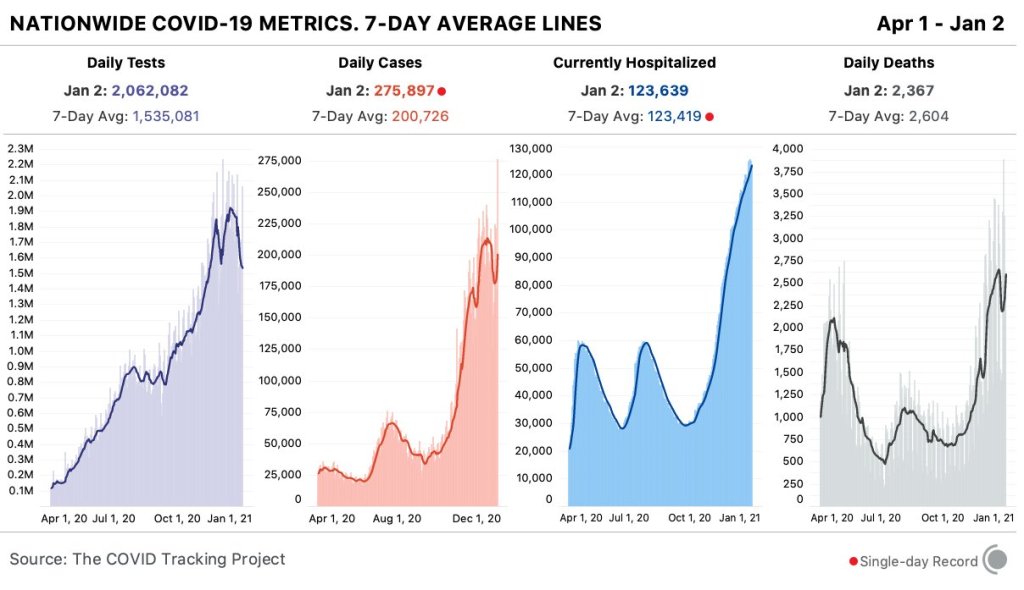
Even if there were a coordinated effort to retroactively sequence all positive tests, some cases of the variant could still slip through the cracks, because most states still aren’t doing enough PCR testing as it is. As of January 8th, according to Ashish Jha’s team at the Brown University School of Public Health, 86% of states aren’t meeting their testing targets. (Meeting testing targets indicates that enough testing is happening to “identify most people reporting symptoms and at least two of their close contacts.” State targets on this dashboard were last configured on October 1, so keep that in mind.) Only two states where the variant has surfaced, Connecticut and New York, are meeting their targets—and cases are surging in both states right now. Longtime readers are going to be very familiar with this problem, but if any new people are reading, this means that in most states we don’t even know how widespread our “garden variety” COVID-19 is. So how are we supposed to know where the UK variant is if we can’t even keep track of the virus that’s been here for almost a year?
Beyond testing, even reporting on confirmed cases of the variant is spotty at best. The CDC is reporting how many detected cases of COVID-19 have been caused by the variant, but no state with a confirmed case caused by B.1.1.7 is displaying that data on their dashboard. (I checked the 8 states’ dashboards and left a comment on California’s because the ask box was right there.) Why is this not on their dashboards? I couldn’t tell you, but it seems like important information that should be reported.
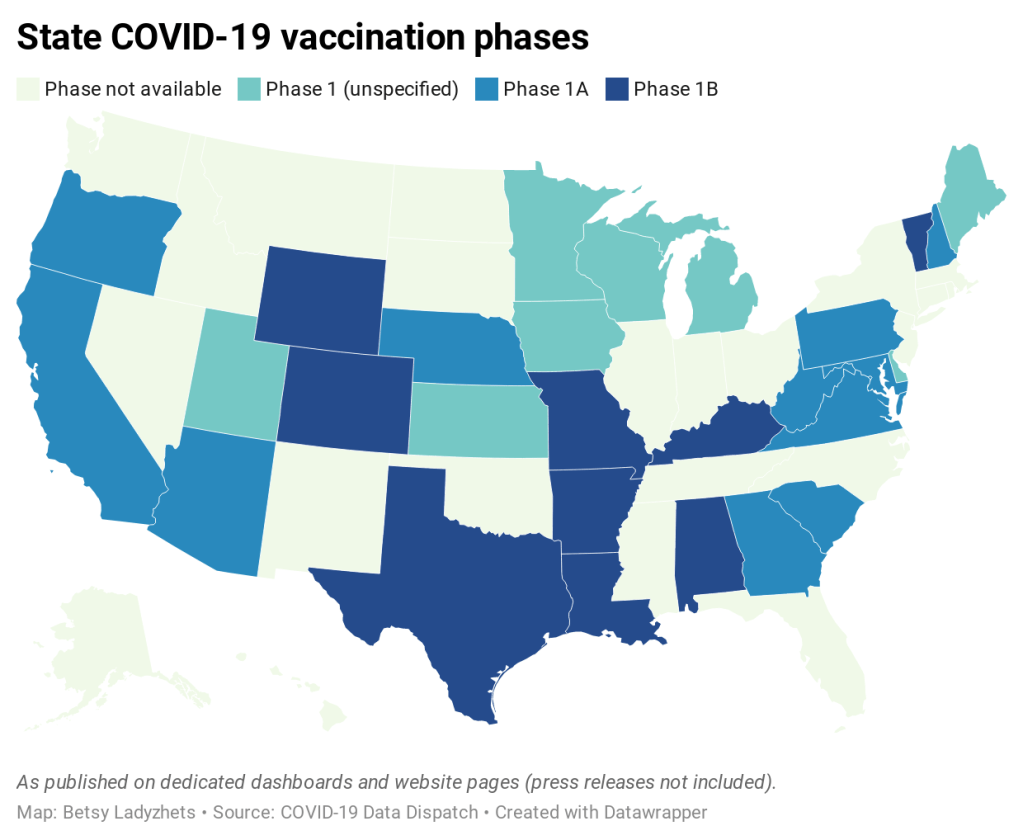
All of these unanswered questions show, yet again, that we desperately need a unified effort from the federal government to track and combat this virus. It should not be this hard to find how we’re tracking the spread of this variant, it should not be this hard to tell which methods work for even identifying the variant, and it should at least be possible to find this data on state health dashboards. It might look like we’re close to the finish line as vaccines continue to be distributed, but we’re tripping over the exact same problems we did at the beginning.