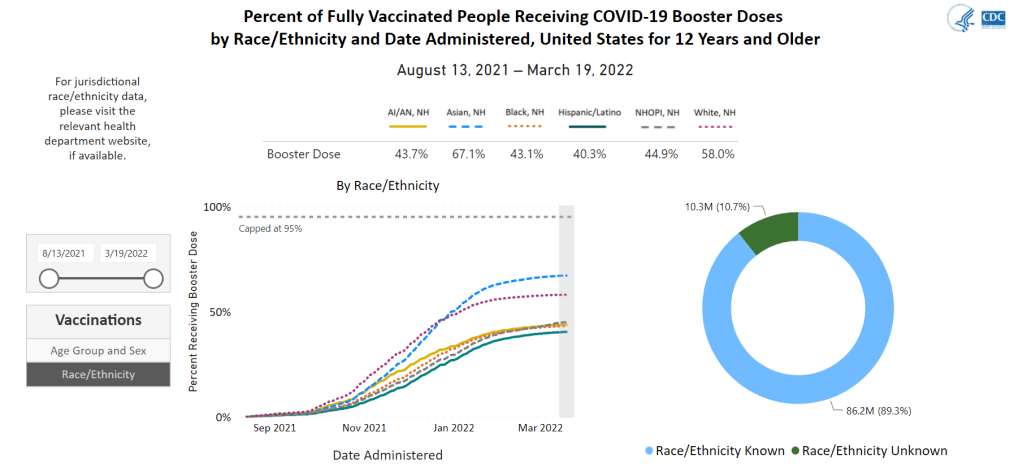
This week, the CDC added a new feature to the vaccination section of its COVID-19 dashboard: you can now look at demographic vaccination trends at the state level, not just nationally and regionally.
But there’s a catch: the state-by-state demographic trends only include age and sex data. Vaccination trends by race and ethnicity are still only available at the national level; in fact, when you click on “Race/Ethnicity” on the booster shots section of this dashboard, the CDC directs you to “please visit the relevant health department website” for more local data.
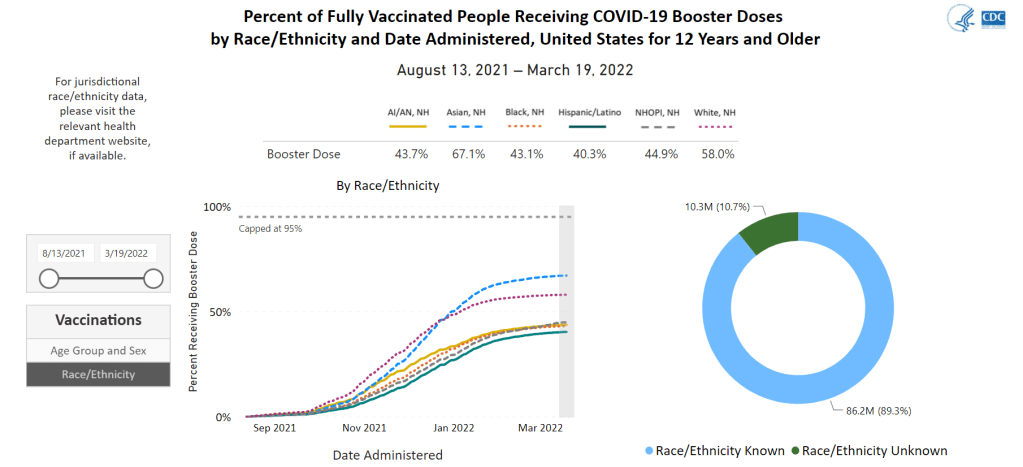
It is now over a year into the U.S.’s vaccine rollout, and the CDC is still failing to publicly share data on vaccinations by state and race/ethnicity. I actually wrote a callout post about this in March 2021, and nothing has changed since then!
This is a major issue because such data are needed to examine equity in the vaccine rollout. While it’s possible to compile data from the states that report vaccinations by race and ethnicity themselves, major inconsistencies in state reporting practices make these data hard to standardize. Why isn’t the CDC doing this? Or, if the CDC is doing this, why aren’t the data public?