Two weeks ago, I shared that I’d recently purchased a monitor to measure CO2 as a proxy for ventilation in my apartment and other spaces. That post led to responses from several readers who’ve also been using CO2 monitors—including Kate Nyhan, a research and education librarian at Yale University who specializes in public health.
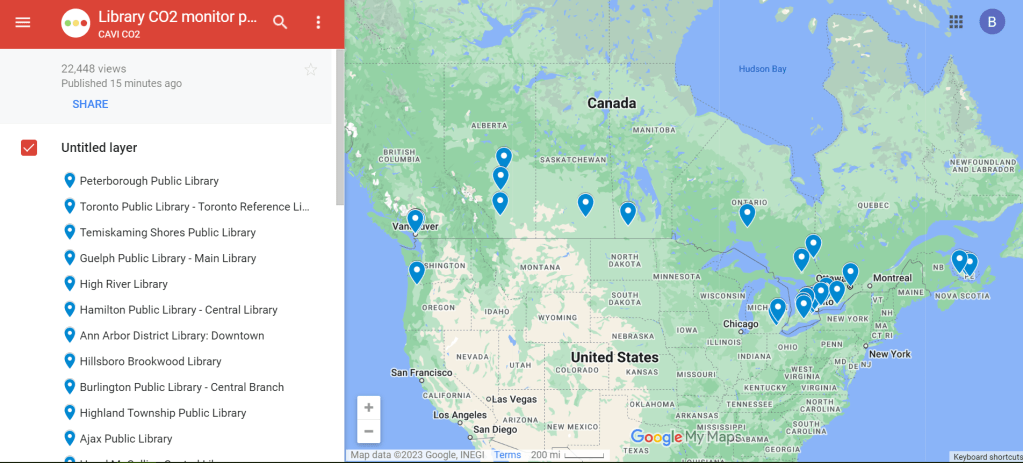
Nyhan explained that, in addition to using a CO2 monitor at her home and workplace, she co-founded a nonprofit that helps public libraries loan out monitors. This nonprofit, called Community Access to Ventilation Information (CAVI), has brought CO2 monitor access to libraries serving about one in five Canadians. In addition to the monitor-lending, CAVI develops educational materials to help library patrons use these tools and collaborates with other air quality initiatives.
I talked to Nyhan and Danielle Cane, CAVI’s managing director, to learn more about the organization and get their tips on using CO2 monitors. Here are the highlights from our conversation.
How CAVI started
Cheryl White, an engineer and air quality expert based in Toronto, Canada, got the idea for this organization in fall 2021. At that time, many people on the COVID-conscious side of Twitter started to express interest in air monitoring, Cane said.
“When we would post our readings from CO2 monitors on social media, a lot of people were saying, ‘This is really cool, I’d love to get involved,’” she recalled. “But it’s just so expensive to access these tools.” Higher-end monitors, like the Aranet device I purchased, can cost around $300.
White had the “bright idea” to partner with libraries as a way to make these monitors more accessible, Cane said. After Cane and Nyhan came onboard, the group reached out to Peterborough Public Library, a library system in a town northeast of Toronto. (Cane and White are both based in the area.)
“Peterborough Public Library was really game to introduce this program,” Cane said. CAVI also worked with the local public health department, which helped gain buy-in for lending out air monitors. The initial Peterborough pilot was launched in spring 2022 with 15 monitors, supported by funding from Canadian and American Aranet distributors.
The city of Toronto later joined the program, followed by other Canadian municipalities. Right now, about 22% of Canadians “have access to a co2 monitor through a public library,” Cane said. CAVI received additional funding in late 2022 to expand further. While the monitor-lending is focused on Canadian libraries, CAVI also produces free, open-source educational materials that can be used in other places.
Why do this in libraries?
Nyhan explained that libraries are well-poised to make air monitors more accessible. “Libraries want to empower community members with access to information,” she said. “In the context of indoor air quality, or COVID transmission risk mitigation, that might be information about airborne transmission, that might be about information about mitigations like air filters… It might be as tangible information as, what’s the number of CO2 parts per million in the space that I’m in right now?”
Lending out CO2 monitors also fits into the “Library of Things,” a concept in which libraries lend out non-traditional items—ranging from home repair tools to arts and crafts materials. As an expensive item that can provide valuable information to the community, CO2 monitors are a great addition to many libraries’ existing collections. In addition, some libraries already have people on staff with public health expertise or existing programming in this area, Nyhan said.
How the program works
The lending system tends to vary from one library to the next, but most places are loaning out CO2 monitors for one week at a time, Cane said: “Especially given the demand in certain areas, like big cities, we find that the one week schedule tends to work out best to both balance, giving people the opportunity to check a variety of settings… and allowing other people to also have that same opportunity.”
Some libraries have seen high demand, especially when the CO2 monitors first arrive at a new library. But as demand levels out over time, patrons might be able to “renew” their loans to keep the monitors for an additional week, Cane explained. Along with the physical monitors, libraries can point patrons to educational resources from CAVI that help interpret the findings.
Interpreting CO2 monitor data
As I’ve found in my own CO2 monitor adventures, there’s a lot these devices can tell you—but also a lot they can’t tell you. The biggest caveat, Cane explained, is that CO2 monitors are “a proxy for ventilation,” not a “proxy for infection risk.” In other words: a really high CO2 reading in a particular space doesn’t necessarily mean that infection is guaranteed, especially if other safety measures are in place. And “a really low reading doesn’t necessarily mean that you will not get infected,” Cane said.
Aranet monitors have a built-in interpretation feature, marking certain CO2 readings as green (good), yellow (less good), and red (bad). But CAVI has produced materials that go into more detail about explaining the ppm (parts per million) measurements. Cane shared one document, designed in partnership with Toronto Public Library, which goes into detail on what higher CO2 readings mean and how to act on them.
Taking action based on CO2 readings
Nyhan used the example of a small car to explain how people may take simple actions based on their CO2 monitors’ results. “Even if it’s just a single person, because [a car is] such a small and tightly enclosed environment, you can very quickly see the impact of breathing out, or opening the window, or changing the air to recirculate or not,” she said. Opening a window or telling the car not to recirculate brings in more outdoor air, causing CO2 levels to get lower.
This is a fairly simple lesson that a library patron might learn during the one week they have with a monitor, Nyhan said: “You learn that, and then you can give the CO2 monitor back to the library so someone else can use it.”
In a larger space, actions based on high CO2 readings might include adding external air filters, opening several windows, or hiring an HVAC engineer to evaluate the ventilation system, Cane said. Not everyone might have the capacity to hire an HVAC engineer, but many people can buy or make air filters; Corsi-Rosenthal boxes are one popular DIY model that can be constructed with commercially available box fans and filters. CAVI has recently partnered with a Canadian high-schooler who’s worked to build these boxes and share accessible instructions.
Nyhan also pointed out that CO2 monitors are “not just for people who control their own spaces” and can easily make ventilation changes. CO2 readings could also inform behavioral safety measures, she said, such as rapid testing before a social gathering in a poorly-ventilated apartment or avoiding certain poorly-ventilated parts of one’s workplace. In some cases, these readings could even be used to advocate for ventilation changes.
Next steps for CAVI
CAVI plans to continue expanding among public libraries in Canada. The organization also works with libraries elsewhere that may want to set up their own CO2 monitor lending programs, Nyhan said. Library staff and users are welcome to reach out to the CAVI team to learn more about the project: “We can share best practices, educational materials, assessment tools, grant proposals,” Nyhan said.
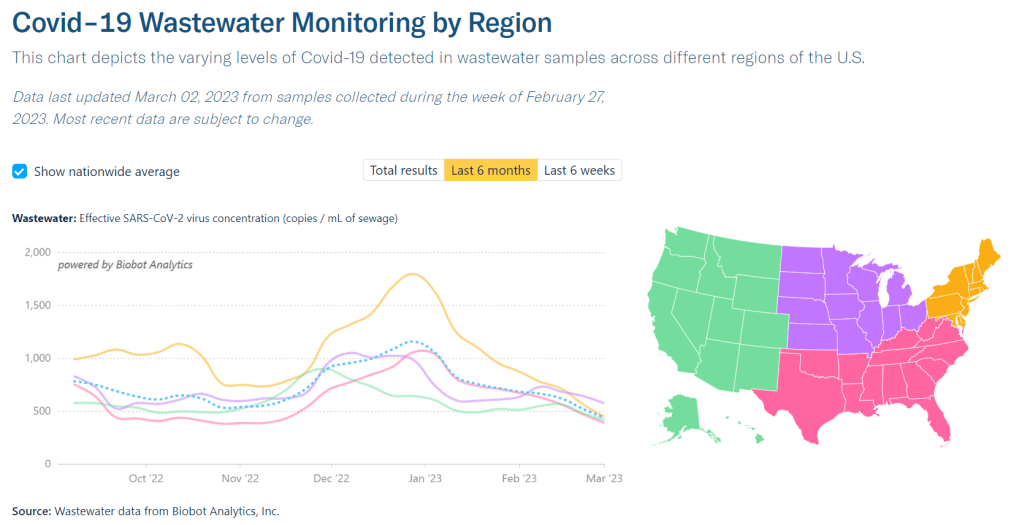
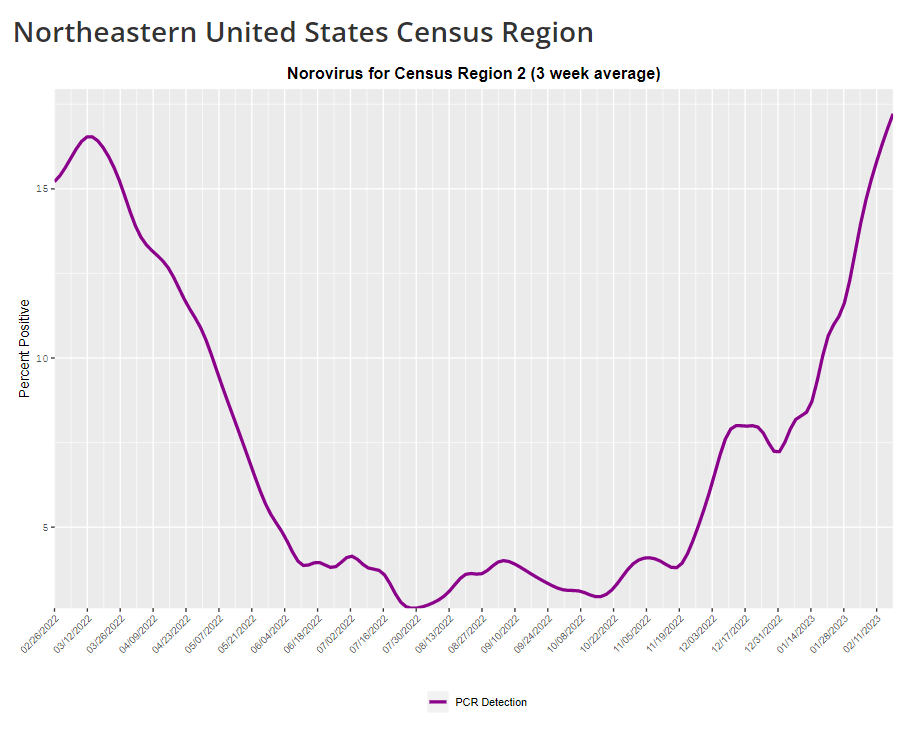
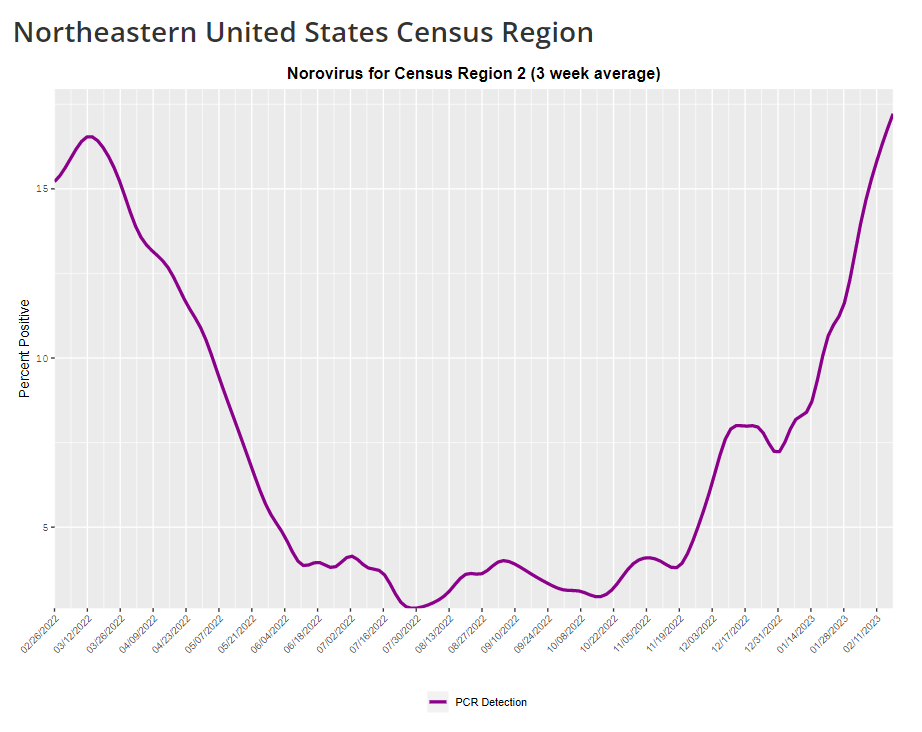
While CAVI, like other air quality citizen science efforts, is currently focused on mitigating COVID-19 risks, its work has implications for many other public health threats. “If we have a wider acceptance of how respiratory pathogens are transmitted, it could be useful to help mitigate other viruses, other bacteria,” Cane said. Improving ventilation can lower the chances of infection for many pathogens and reduce the health risks associated with indoor air pollutants.
Lending out air monitors fits into work that some public libraries are already doing on environmental health, Nyhan said. Libraries might have existing programs about wildfire smoke, radon, and similar air quality threats; COVID-19 and pathogens like it provide motivation for expanding these efforts. “Indoor air quality, and environmental health more generally, is a hot topic that’s only going to get more important,” Nyhan said.