- Holiday risk estimator: A group of data analysts at the Rockefeller Foundation’s Pandemic Prevention Institute put together this tool showing the risk of coronavirus exposure at an event or gathering, taking Omicron’s increased transmissibility into account. You can plug in your county and view your risk at 10, 20, and 30-person events, with adjustments for attendee vaccination and rapid testing. The tool will be updated daily through the end of December, according to analyst Kaitlyn Johnson, with potential further updates after that point.
- State Reporting of Covid-19 Vaccine Breakthrough Infections: Another source from the Rockefeller Foundation: researchers from the Pandemic Tracking Collective evaluated every state’s reporting of COVID-19 breakthrough cases. The evaluations include both the data fields states report and how information is presented. Only three states (California, Colorado, and Utah) scored an A; nine states that don’t share breakthrough case data regularly scored an F.
- POLITICO’s State Pandemic Scorecard: And another evaluation of how states fared, but much broader: POLITICO reporters compiled data about state outcomes during the COVID-19 pandemic, including health, economy, social well-being, and education. For each category, states are scored between zero and 100. “No state did well in every policy area,” the report finds; for example, some states that imposed more COVID-19 restrictions fared better on health but worse on economy and education.
Category: Uncategorized
-
Featured sources, December 26
-
The 21 best COVID-19 data stories of 2021
As 2021 comes to a close, I want to dedicate this final issue of the year to all of the other science, health, and data journalists who have continued following COVID-19 in the last twelve months. It hasn’t been easy, as burnout dovetails with declining public interest in pandemic news; still, so many people have stuck with this beat and brought important issues to light.
Here’s my list of the 21 best COVID-19 data stories of 2021. Disclaimer: this list is not comprehensive or objective—I selected these stories from my own readings of national and local outlets, combined with a couple of reader submissions. Still, I tried to include a variety of publications and story types, ranging from short news pieces to large investigative projects.
If you’d like to check out my 2020 list, you can find it here.
- The “Good” Metric Is Pretty Bad: Why It’s Hard to Count the People Who Have Recovered from COVID-19 (COVID Tracking Project, Jan. 13): This analysis post illuminates the issues behind tracking “recovered” COVID-19 patients, a metric that used to appear on many state dashboards. Amanda French and Quang Nguyen explore the inconsistent definitions that states use to track this metric—most COVID-19 metrics are inconsistent from one source to another, but “recovery” is particularly inconsistent—as well as how the metric excludes Long COVID patients. The post also explains why CTP removed many “recovered” values from its website.
- As Covid vaccine rollout expands, Black Americans still left behind (KHN/NBC, Jan. 29): While vaccines became more widely available throughout the early months of 2021, the CDC’s data on which Americans were getting vaccinated remained extremely limited. In fact, the agency has never released demographic vaccination data at the state-by-state level. KHN reporters Hannah Recht and Lauren Weber filled that gap by compiling data from state dashboards, while also reporting on the vaccine gap between Black and white Americans.
- As governor cherry-picked data, the pandemic took a toll on Florida Sunshine laws (Miami Herald, March 2): Throughout the pandemic, Florida has attracted attention—from Governor Ron DeSantis railing against mandates to the Florida Department of Health (FDOH) replacing its comprehensive COVID-19 dashboard with stripped-down weekly reports in June. This important Miami Herald article sheds light on FDOH’s reluctance to “release new data related to COVID-19 that contradicts the governor’s upbeat narrative,” hurting journalists’ and academics’ ability to hold the DeSantis administration accountable.
- The uncounted: People who are homeless are invisible victims of Covid-19 (STAT News, March 11): Usha Lee McFarling, national science correspondent at STAT News, has spent the year reporting on equity issues connected to COVID-19 and other areas of medicine. In this story, she investigates the lack of COVID-19 deaths reported among homeless populations. According to McFarling, one attempt to track these deaths resulted in a count of under 400, even though homeless shelters are prime locations for outbreaks.
- Why the Pandemic Experts Failed (The Atlantic, March 15): On March 7, the COVID Tracking Project updated its datasets for the last time. Shortly afterwards, founders Alexis Madrigal and Robinson Meyer wrote this story sharing lessons learned from a year of data collection, including the challenges of reporting COVID-19 data, the impact of America’s fractured public health systems, and what data can and can’t tell us. For more: check out the project’s analysis posts with further lessons and resources for using federal COVID-19 data.
- 3.9 million years (Vox, March 17): Typically, when we think about the losses of COVID-19, we think of the number of deaths. But there’s another metric we can use, beautifully explored in this Vox article: years of potential life lost. As of January 31, 2021, the U.S. has recorded about 420,000 deaths, amounting to 3.9 million years lost. The article includes an illustration of this toll, as well as personal stories from the family members of those who died.
- We Ran Tests on Every State’s COVID-19 Vaccine Website (The Markup, March 24): The Markup, a nonprofit newsroom that investigates big tech, is famous for its Blacklight tool, which scans websites for user-tracking technologies. In this story, The Markup ran that Blacklight tool on state websites built for users to make their vaccination appointments. The tool found that many sites had below-average privacy ratings and poor accessibility, likely contributing to the stress that many Americans felt in trying to book their vaccinations.
- A Tiny Number of People Will Be Hospitalized Despite Being Vaccinated. We Have to Learn Why. (ProPublica, April 14): ProPublica’s Caroline Chen was writing about breakthrough infections before it was cool—or, before Delta hit the U.S. and these infections became common. This article clearly explains what breakthrough infections are, why they’re so rare (at the time), and why they need to be investigated anyway, as scientists hope to find patterns in the breakthrough cases that lead to severe disease. At the time, many states were doing a poor job of data collection; this is still true, many months later.
- The First Billion Doses (Bloomberg, April 24): Since late 2020, a group of Bloomberg health and data journalists have run the most comprehensive dashboard on global COVID-19 vaccinations, including data from 184 countries and all U.S. states. It’s an immense undertaking, and has driven plenty of important reporting on vaccine rollouts nationally and globally—such as this story marking the first billion doses administered. The piece both celebrates this scientific achievement and highlights inequities: “Vaccine access so far has been determined by national wealth,” the story says.
- COMIC: For my job, I check death tolls from COVID. Why am I numb to the numbers? (NPR, April 25): This comic, by one of the reporters behind NPR’s COVID-19 dashboard, resonated deeply with me. It explores why one death may feel like a tragedy, but 500,000 deaths may feel like a natural part of the world. The comic ends by emphasizing the importance of reading individual people’s stories and maintaining connection, to cope with all of the trauma and loss of the past two years.
- Broken system can’t keep track of Native deaths (Indian Country Today, June 8): In this story, the Indigenous Investigative Collective explores how a “labyrinthian system of local, state, federal and tribal data-reporting systems” makes it difficult to accurately track how many Native Americans have died of COVID-19. As a result, the already-high official death toll is likely a significant undercount; and the problem goes beyond COVID-19 to other health issues.
- New CDC dataset showing COVID vaccine-by-county numbers misses the entire state of Texas. Why? (Houston Chronicle, June 23): For a long time, there was a Texas-shaped hole in the CDC’s dataset of COVID-19 vaccinations by county. This article, by Houston Chronicle reporter Kirkland An, digs into the issue and explains: a unique state law in Texas restricts sharing of individual data, including the anonymized vaccination records that the CDC requested from states in order to calculate county-level vaccination rates. To me, this is a great example of a local reporter diving into an issue that their region is facing in a national dataset. (And the data issue has since been fixed!)
- How Local Reporters in India Exposed the Pandemic’s True Death Toll (Global Investigative Journalism Network, June 28): This one is a bit meta: it’s an article about COVID-19 death investigations, carried out by journalists in India during the country’s severe spring 2021 surge. One reporter, Yogen Joshi, used counts of Hindu funeral rituals at a holy riverbed site to reveal that the true number of deaths in the state of Gujarat was much higher than the official record stated. Other journalists similarly investigated body counts and death certificates directly, showing how national data fell short.
- Meet the people who warn the world about new covid variants (MIT Technology Review, July 26): MIT Technology Review’s Pandemic Technology Project has produced a number of important COVID-19 stories this year (including my own!), but this one is my personal favorite. Cat Ferguson profiled a group of scientists who created and contributed to the Pango system for tracking coronavirus variants, racing to name and classify new sequences as soon as they’re uploaded into the public domain. This article demonstrates the human toll of running such an important database, particularly when it’s led by PhD students and postdocs who never anticipated the scale their project would attain.
- Inside America’s Covid-reporting breakdown (POLITICO, Aug. 15): At this point, most COVID-19 reporters are familiar with the challenges underlying our spotty pandemic numbers: public health agencies have long been underfunded, records are transmitted by fax and mail, data systems are inconsistent, workers are overwhelmed, etc. But few articles lay out the problems as clearly as this feature by POLITICO’s Erin Banco, who spoke to health officials in more than 20 states. The article also includes great data visualizations and graphics that illustrate the issues.
- Ahead Of NYC School Reopening, 1,500 Classrooms Still Undergoing Ventilation Repairs (Gothamist/WNYC, Aug. 30): By mid-2020, there was a growing scientific consensus that the coronavirus spreads through the air, and ventilation is an important means of increasing COVID-19 safety. Yet businesses and news cycles alike failed to focus on ventilation well into 2021—so I was very excited to see Gothamist’s thorough investigation of air filtration in New York City schools. This article is part one in an extensive series, combining city records with expert insights on air quality standards.
- How did a Kansas grandmother just become the first U.S. COVID death? Not even her family knew until this week (The Mercury News, Sept. 2): Sometimes, the best kind of data story is an investigation into one singular data point. This piece, published in Bay Area newspaper The Mercury News, tells the story of Lovell Brown, a senior in Leavenworth County, Kansas who is now the first recorded COVID-19 death in the U.S.—after her death certificate was amended in May 2021 to include the disease. While the exact reasons behind this death certificate update are unknown, the revision suggests that the coronavirus was spreading in the Kansas City area well before official data collection started.
- The fight to manufacture COVID vaccines in lower-income countries (Nature, Sept. 15): As someone who has been writing about global health long before COVID-19 hit, Amy Maxmen is an expert on the global vaccination beat. This story lays out the immense gap between vaccine access in high-income countries and low-income countries, while also explaining a potential solution: many manufacturers in low- and middle-income countries are ready to produce COVID-19 vaccines, if only they could get ahold of the patents. I’ve come back to reread this piece several times in the past few months, as booster shot campaigns in the U.S. and elsewhere have further exacerbated vaccine inequity.
- Opening Project conclusion: 11 lessons from the schools that safely reopened (COVID-19 Data Dispatch, Sept. 19): Yes, I snuck one of my own projects onto this list: the Opening Project, in which I identified and profiled five school communities that brought the majority of their students back to in-person learning by the end of the 2020-2021 school year while reporting fewer COVID-19 cases than the national average. For me, this project was a departure from past data journalism stories; instead of describing an overall trend with data, I focused on five outliers, investigating why they were successful. The project, which was funded with a grant from the Solutions Journalism Network, was republished at several education and science news outlets.
- Covid response hampered by population data glitches (Financial Times, Oct. 11): Vaccination rates—which show the percentage of a population that’s received at least one vaccine dose or been fully vaccinated—have been a key metric driving government COVID-19 responses in the past year. But when the population data underlying these calculations are inaccurate, this article by Oliver Barnes and John Burn-Murdoch explains, the vaccination rates can be way off. For example, some Miami, Florida ZIP codes have vaccination rates of over 200% among seniors, because snowbirds who don’t formally reside in the city got vaccinated there. (If you hit the Financial Times’ paywall, you can read my summary of the piece here.)
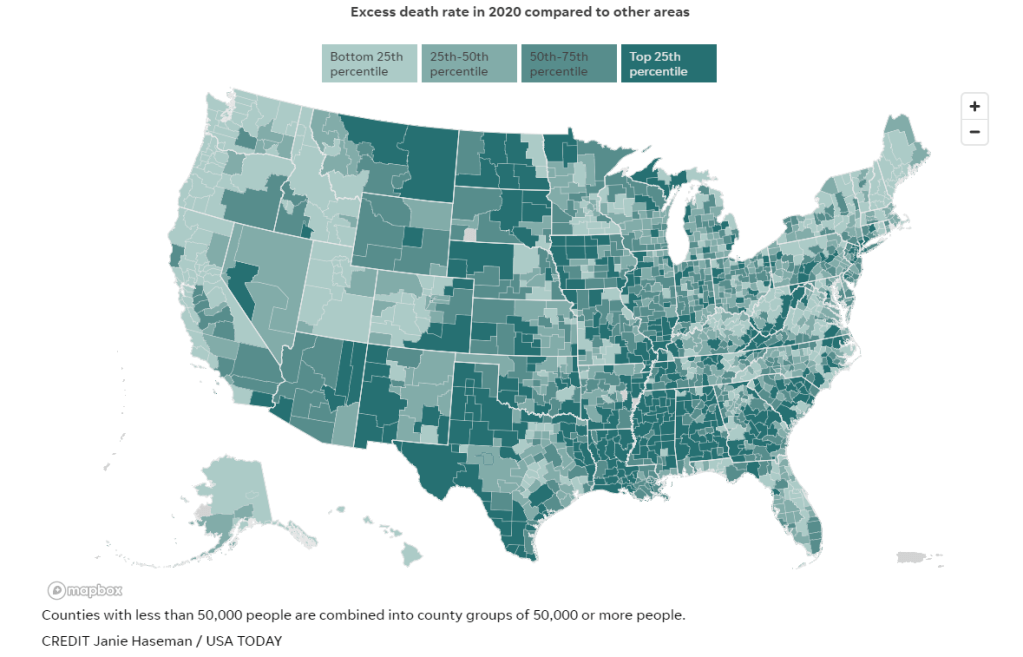
- Uncounted: Inaccurate death certificates across the country hide the true toll of COVID-19 (Documenting COVID-19 & USA Today, Dec. 22): For months, the Documenting COVID-19 team has worked with several USA Today newsrooms to investigate unreported COVID-19 deaths. While the official COVID-19 death toll in the U.S. is about 800,000, experts suspect that up to 200,000 additional deaths from the disease have gone uncounted, due to a combination of undertrained coroners and medical examiners, a lack of standardization for identifying these deaths, under-testing, and other issues with death certificates. I was part of the team behind this investigation, which will continue with further stories in 2022; you can read more about the CDC data that drove much of our analysis here.
Note: the featured image for this post is taken from the Uncounted project; it’s a visualization by Janie Haseman at USA TODAY.
-
National numbers, December 26

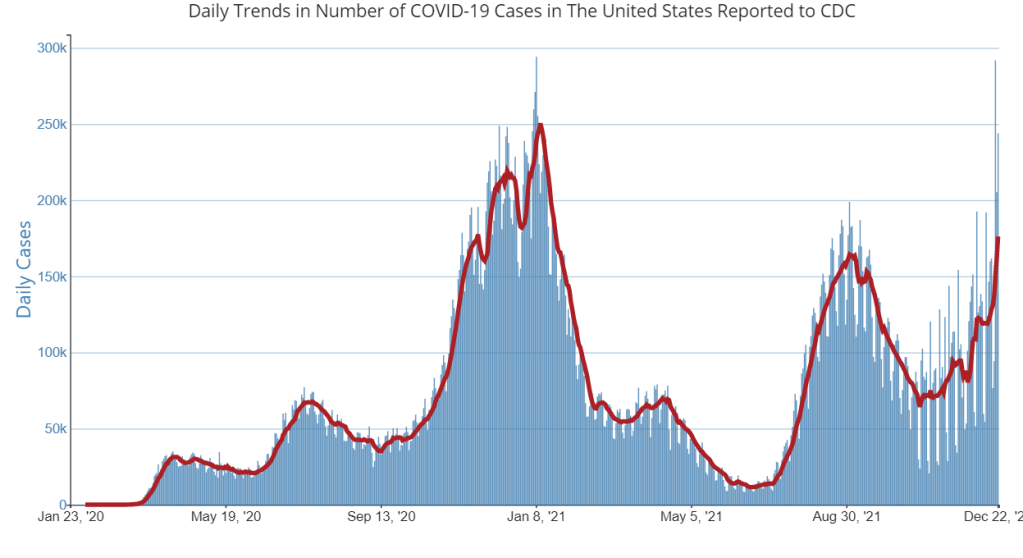
The seven-day average for new COVID-19 cases in the U.S. on December 23 has passed the peak of the Delta surge. Chart via the CDC. In the past week (December 17 through 23), the U.S. reported about 1.2 million new cases, according to the CDC.* This amounts to:
- An average of 176,000 new cases each day
- 376 total new cases for every 100,000 Americans
- 42% more new cases than last week (December 10-16)
Last week, America also saw:
- 55,000 new COVID-19 patients admitted to hospitals (17 for every 100,000 people)
- 8,500 new COVID-19 deaths (2.6 for every 100,000 people)
- 73% of new cases are Omicron-caused (as of December 18)
- An average of 1.4 million vaccinations per day (including booster shots; per Bloomberg)
*This week’s update is based on data as of Thursday, December 23; I typically utilize the CDC’s Friday updates, but the agency is not updating any data from Friday through Sunday this week due to the Christmas holiday.
Last week, the Omicron surge had clearly arrived; this week, it’s picking up steam. Nationwide, the U.S. reported well over one million new cases this week—more than a 40% increase from last week. 244,000 cases were reported on Thursday alone, and the daily new case average is now higher than at any point during the Delta surge.
Hospitalization and death numbers have yet to increase so sharply: the number of new COVID-19 patients admitted to hospitals this week is up less than 1%, and the number of new COVID-19 deaths is up by about 4%.
But when Omicron reaches those Americans who are more vulnerable to COVID-19, they’ll arrive at hospitals already overwhelmed from Delta, the flu, and nearly two years of pandemic burnout. At the same time, Omicron’s incredible capacity to spread will likely cause staffing shortages for many hospitals, as workers get breakthrough cases. On Thursday, the CDC announced that healthcare workers who get sick may shorten their quarantines if their facilities are facing shortages.
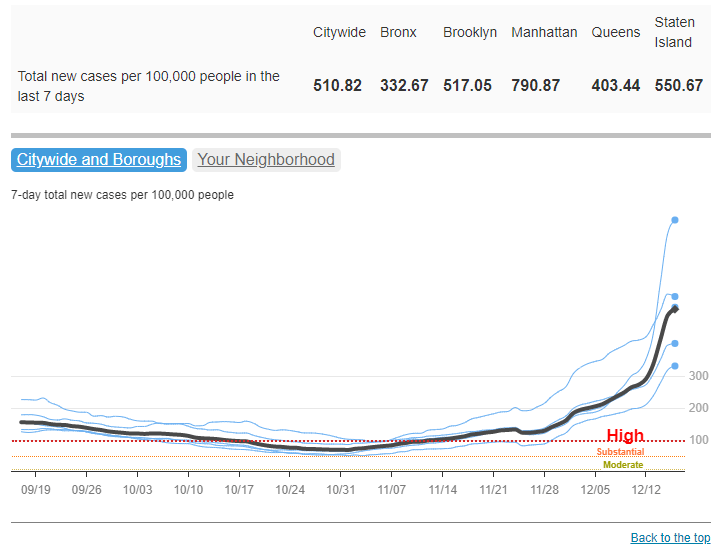
New York City continues to be a major Omicron hotspot: according to city data, one in every 100 New Yorkers has tested positive for COVID-19 in the last week. In Manhattan, the number is one in 60. And these numbers don’t include people who tested positive on rapid at-home tests and weren’t able to confirm it with PCR. The city’s test positivity rate is over 10%, indicating that a lot of cases are going unreported in official data.
Washington, D.C. has also emerged as a Omicron hotspot this week, with an average of over 1,000 new cases reported daily in the week ending December 22. That’s more than three times higher than the city’s case record at any other point during the pandemic. Meanwhile, several states have seen their case rates more than double in the past week, according to the latest Community Profile Report: Hawaii, Florida, Louisiana, Georgia, and Maryland.
As Omicron sweeps across the country—aided by holiday travel and gatherings—we are about to face the reporting delays that come with every holiday. Public health workers from local agencies to the CDC are taking time off, while testing sites close for Christmas and millions of rapid tests go unreported.
Erin Kissane, co-founder of the COVID Tracking Project, wrote about holiday data issues in The Atlantic this week. Her piece concludes:
In this information vacuum, some of us will tend toward caution and others toward risk. By the time Americans find out the results of our collective actions, the country will have weeks of new cases—an unknown proportion of which will turn into hospitalizations and deaths—baked in. In the meantime, the CDC’s COVID Data Tracker Weekly Review has wished us all a safe and happy holiday and gone on break until January 7, 2022.
-
Featured sources, December 19
- COVID-19 preventable mortality and leading cause of death ranking: The Peterson-KFF Health System Tracker has recently updated its analysis of preventable deaths from COVID-19 and the disease’s position among top causes of death in the U.S. In November 2021, COVID-19 was the #3 cause of death after heart disease and cancer. And, between June and November, more than 160,000 COVID-19 deaths could have been prevented with vaccinations.
- AARP analysis of nursing home data: AARP researchers have analyzed and visualized data showing staff shortages in nursing homes, along with vaccination rates, PPE availability, and other related figures. According to AARP’s analysis, almost one-third of the 15,000 nursing homes in the U.S. “recently reported a shortage of nurses or aides,” as of mid-November. (H/t Al Tompkins’ COVID-19 newsletter.)
- News workers laid off and outlets closed during the pandemic: At least 6,154 workers at news organizations were laid off between March 2020 and August 2021, according to a new report from Columbia Journalism Review. And at least 100 organizations closed during this time, though 14 have since resumed operations to some extent. The report includes detailed data on these layoffs and organization closures.
- Recommendations to transform public health data in the U.S.: The Robert Wood Johnson Foundation, a health philanthropy organization, has convened a commission of experts to reimagine how public health data are collected, shared, and used in the U.S. The commission put together this report, which includes recommendations ranging from data literacy to racial equity. While the report doesn’t include much data, per se, I wanted to include it in this week’s issue as a resource—and a source for potential story ideas.
- Science Literacy Resource Guide: The Science Literacy Foundation, a new nonprofit in the scicomm space, had compiled this database of science literacy-related resources. It includes resources specific to journalism, communication, education, policy, and research; the guide isn’t COVID-specific, but has a lot of utility for continued pandemic coverage. (Disclaimer: I’ve previously worked on a project for the Science Literacy Foundation, but was not involved with this guide.)
-
Send me your favorite COVID-19 data stories of 2021
In late December last year, I shared a list of news stories and projects that I considered the 20 best COVID-19 data stories of 2020. The list ranged from early STAT News coverage of the novel coronavirus, to a FiveThirtyEight investigation of testing access, to THE CITY’s online memorial of New Yorkers who lost their lives to COVID-19.
I enjoyed compiling the list because it gave me a way to look back on COVID-19 news coverage throughout 2020, with a focus on those stories that dug into the numbers—whether that was visualizing pandemic trends or explaining an issue with data collection and reporting. (Also, it was a fairly straightforward issue to compile and send out two days after Christmas!)
This year, I’m planning to compile a similar list: the 21 best COVID-19 data stories of 2021.
And I need your help to pick these stories! Last year’s list was very U.S.-heavy, as I primarily read coverage from national and New York city-specific publications, and I would love to make this year’s list more geographically diverse. Please send me COVID-19 data stories you loved from your local news outlet, your favorite science journalist, or any other publication.
To submit ideas, you can comment below, email me at betsy@coviddatadispatch.com, or reach out on Twitter or Facebook. My full list will go out in next week’s issue, on December 26, and I’ll accept submissions until the 25th.
-
National numbers, December 19
COVID-19 cases have increased sharply in New York City in the past week, to over 500 new cases for every 100,000 people city-wide. Chart via NYC Health, retrieved December 19. In the past week (December 11 through 17), the U.S. reported about 860,000 new cases, according to the CDC. This amounts to:
- An average of 122,000 new cases each day
- 261 total new cases for every 100,000 Americans
- 2% more new cases than last week (December 4-10)
Last week, America also saw:
- 55,000 new COVID-19 patients admitted to hospitals (17 for every 100,000 people)
- 8,300 new COVID-19 deaths (2.5 for every 100,000 people)
- 2.9% of new cases are Omicron-caused (as of December 11)
- An average of 1.6 million vaccinations per day (including booster shots; per Bloomberg)
The Omicron surge has arrived in the U.S. While national COVID-19 cases are not significantly up from last week to this week, last week’s bump in the numbers from delayed Thanksgiving reporting has been replaced with a true increase, thanks to the combined pressures of both Delta and Omicron.
Hospitalizations are also increasing, with about 60,000 Americans hospitalized with COVID-19 nationwide as of December 15—a 9% increase from the previous week. The number of Americans dying from COVID-19 each day is increasing as well, now at about 1,200 deaths a day.
Omicron’s impact feels particularly pronounced in New York City, where I live, as the city’s case rate more than doubled in the first two weeks of December. This past week, the city’s test positivity rate doubled in the span of three days. Yesterday, New York state reported a record number of new COVID-19 cases (about 22,000), with more than half of those cases reported in NYC.
To be fair, the case rates reported in NYC this week are probably lower than the true case rates during spring 2020, as testing wasn’t widely available during the city’s first COVID-19 surge. But on a personal level, this city’s current Omicron surge is undeniable: testing lines stretch around the block, and everyone from my old college friends to my local City Council representative is reporting a breakthrough case. I personally have yet to catch “the Media Variant,” but I’m rapid testing frequently and avoiding indoor activities as I prepare to visit my parents for Christmas.
Omicron was causing 13% of new COVID-19 cases in New York and New Jersey in the week ending December 11. By today, it’s likely causing the majority of new cases. But the NYC region isn’t the only part of the country seeing rapid case increases: Hawaii, Florida, Connecticut, Maine, and D.C. have all reported more than a 30% increase in cases from the previous week to this one, according to the latest Community Profile Report. Rhode Island, New Hampshire, Maine, and other Northern states have the highest cases per capita.
Vaccines, particularly booster shots, can protect against this dangerous variant (more on that later in this issue). While 61% of Americans are fully vaccinated, according to the CDC, less than 30% have received booster doses. This includes about 53% of Americans over 65, even though seniors were one of the first groups become eligible for boosters—and are among those most in need of this additional protection.
-
Sources and updates, December 12
- CDC adds booster shot trends to its dashboard: One significant update to the CDC’s COVID-19 dashboard this week: the agency has added daily booster shot administration trends to its Vaccination Trends page. Now, you can see how many booster shots are being given each day in your state; in New York, for example, I see clear jumps when eligibility opened to all adults, and when Omicron was identified after Thanksgiving.
- Global Health Security Index: Back in fall 2019, a group of public health and national security researchers put out an index that ranked 195 countries around the world on their capacity to respond to future health threats. The U.S. was ranked number one—a ranking that soon became laughable as the country proved to be incredibly unprepared for the COVID-19 pandemic. This week, the organization released their 2021 update to that index… and the U.S. is, somehow, still number one. Yet despite this, the researchers say, “no country is fully prepared for future pandemic or epidemic threats.”
- COVID Collaborative: Hidden Pain report: The COVID Collaborative is a team of health, education, and economic experts aiming to develop recommendations for U.S. leaders. Their recent Hidden Pain report focuses on children who lost parents or caretakers to COVID-19—a group that, the report estimates, includes over 167,000 children across the country.
- State Alcohol-Related Laws During COVID-19: The Alcohol Policy Information System has compiled a database of alcohol-related state laws during the pandemic, including rules about drinking both inside and outside of bars and restaurants. The database allows you to see when a specific state allowed restaurants to open or close, restrictions for take-out only, shortened hours, and more. (H/t Data Is Plural.)
-
National numbers, December 12

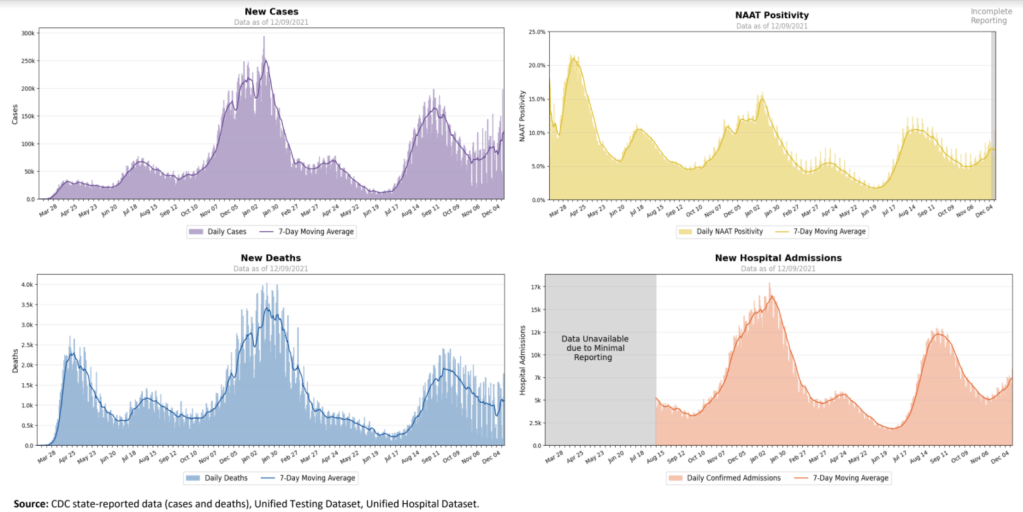
All major COVID-19 metrics shot up in the U.S. this week. Chart from the December 9 HHS Community Profile Report. In the past week (December 4 through 10), the U.S. reported about 830,000 new cases, according to the CDC. This amounts to:
- An average of 119,000 new cases each day
- 253 total new cases for every 100,000 Americans
- 37% more new cases than last week (November 27-December 3)
Last week, America also saw:
- 52,000 new COVID-19 patients admitted to hospitals (16 for every 100,000 people)
- 7,600 new COVID-19 deaths (2.3 for every 100,000 people)
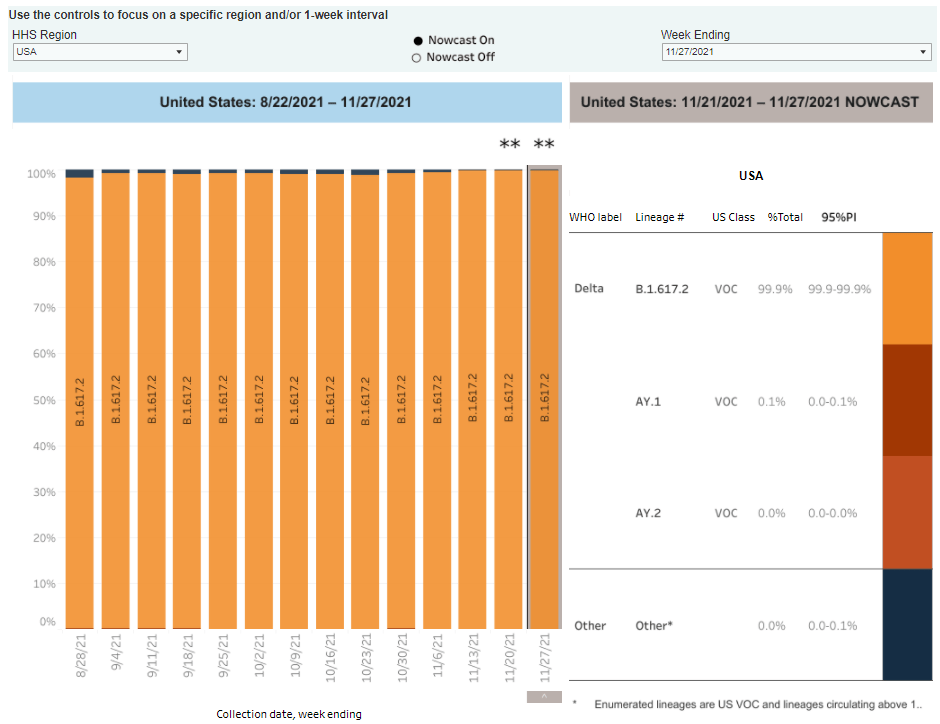
- 99.9% of new cases are Delta-caused (as of December 4)
- An average of 2.3 million vaccinations per day (including booster shots; per Bloomberg)
Remember how, last week, I said that the dip in the CDC’s case counts was a vestige of Thanksgiving data delays—and we’d see more cases in the next week? Well, we’re seeing those cases now. Cases have increased by 37% from last week to this week, and they’ve increased by 55% in the last month.
Hospitalizations are also going up: the number of new COVID-19 patients admitted to hospitals each day has risen 16%, to over 7,000. About 56,000 people are currently hospitalized with COVID-19 in the U.S., as of Thursday. And, tragically, death counts are rising as well: once again, over 1,000 Americans are dying from COVID-19 every day.
Current hotspots include states in the Northeast and Midwest. New Hampshire reported the most cases per capita last week, at 659 new cases for every 100,000 people, per the latest Community Profile Report. Michigan, Minnesota, Rhode Island, and New Mexico also all reported over 500 new cases for every 100,000 people.
In many parts of the country, COVID-19 patients have once again pushed hospitals to their breaking points, as the pandemic intersects with staff shortages and burnout as well as flu and other conditions. “We’re at capacity on a daily basis,” the president of a hospital system in Detroit told a local reporter.
Despite growing Omicron concerns (more on that later), the Delta variant is clearly driving this surge. According to the CDC’s estimates, the Delta variant has caused more than 99% of cases in the week ending December 4, while Omicron has yet to cause even 0.1%. If Omicron is able to outcompete Delta in the U.S., the situation could become even more dire.
It’s now been two years since a COVID-19 patient first sought medical attention, at a hospital in Wuhan, China. Though most Americans didn’t become aware of the pandemic until March 2020, the coronavirus was already spreading in December 2019—meaning that now, in December 2021, we’re entering Year Three of this global crisis. I hope this can be the year that we get vaccines to every country in the world, and truly get the virus under control.
-
Sources and updates, December 5
- State approaches to contact tracing: This report from the National Academy for State Health Policy, updated on December 2, explores how every U.S. state is approaching contact tracing for COVID-19 cases. The report includes state partnerships with research institutions, adjustments for case surges, workforce sizes and training, digital contact tracing apps, and more. (H/t Al Tompkins’ COVID-19 newsletter.)
- KFF COVID-19 Vaccine Monitor (December update): The newest polling report from the Kaiser Family Foundation’s Vaccine Monitor project is out this week, detailing public opinion on vaccinations, including booster shots, mandates, and more. Two notable findings: four in ten Republican adults are unvaccinated, and Republicans are less likely to report receiving a booster dose than Democrats.
-
National numbers, December 5

Though Omicron is making headlines, Delta is still causing 100% of COVID-19 cases in the U.S. Chart via the CDC, screenshot taken on December 5. In the past week (November 27 through December 3), the U.S. reported about 600,000 new cases, according to the CDC. This amounts to:
- An average of 86,000 new cases each day
- 184 total new cases for every 100,000 Americans
- 8% fewer new cases than last week (November 20-26)
Last week, America also saw:
- 45,000 new COVID-19 patients admitted to hospitals (14 for every 100,000 people)
- 6,000 new COVID-19 deaths (1.8 for every 100,000 people)
- 100% of new cases are Delta-caused (as of November 27)
- An average of one million vaccinations per day (including booster shots; per Bloomberg)
Don’t be fooled by the apparent case decline in the CDC’s numbers: the U.S. is still in the midst of a new surge. The agency reported fewer cases last week due to Thanksgiving holiday delays, but we can expect cases to shoot up next week as delayed cases are added to the data.
I use the CDC for these updates because I find the national agency’s data reliable and easy to access, but the CDC does tend to be more heavily impacted by reporting delays than other sources which compile numbers from U.S. states or counties. For example, the New York Times is reporting a daily new case average of 108,000 as of December 4, while BNO Newsroom has reported over 100,000 new cases for five days in a row.
Meanwhile, hospitalizations are ticking up: with 45,000 new COVID-19 patients admitted to U.S. hospitals last week and almost 50,000 people currently hospitalized, as of December 2. Hospitalizations are one COVID-19 metric that tends to be less impacted by holidays, as the hospitals collecting these data don’t take days off.
Northern states continue to lead the country in new cases per capita. According to the latest Community Profile Report, top hotspots are New Hampshire, Michigan, Minnesota, North Dakota, and Wisconsin. New Hampshire reported over 500 new cases for every 100,000 people in the last week, and is continually setting new COVID-19 records.
Michigan is seeing more cases now than it has in any previous surge, and the state’s hospital systems—like many others—are facing dire staff shortages, along with increased numbers of flu patients. The state has almost 900 fewer staffed hospital beds now than in November 2020, according to ABC News.
While the Omicron variant has now been identified in more than ten U.S. states (more on that below), the Delta variant is still driving this current surge. According to the CDC’s latest variant data, 100% of new cases in the country are caused by Delta. In the coming weeks, we’ll see how much Omicron is able to compete.