For months, I’ve been calling on the CDC to release state-by-state demographic data on who is getting vaccinated. While the vast majority of states report this information themselves, the state data are completely unstandardized—making it difficult to perform comprehensive analyses or compare one state to another.
“The vaccine data that individual states are publishing replicate the patchwork nature of the other state-level COVID-19 data our teams have been compiling,” COVID Tracking Project leaders Alice Goldfarb and Erin Kissane wrote in The Atlantic in January.
While many more states are reporting vaccination demographics now than in January—Montana and Wyoming are the only two states that now fail to report vaccinations by race—the data continue to be patchwork and hard to analyze.
Bloomberg has devoted a small team to analyzing and presenting these data in the publication’s U.S. Vaccine Demographics Tracker. But Bloomberg isn’t making their underlying data public, so other journalists and researchers are unable to build on this work. And really, it shouldn’t be on journalists to standardize from a fragmented state-by-state landscape—it should be the work of the CDC.
That’s why I was thrilled when, this week, we finally got that data from the CDC. Well… sort-of.
A team from KHN received CDC state-by-state demographic vaccination data via a public records request. This team—which includes Hannah Recht, Rachana Pradhan, and Lauren Weber—analyzed the CDC’s data and made their work public on GitHub.
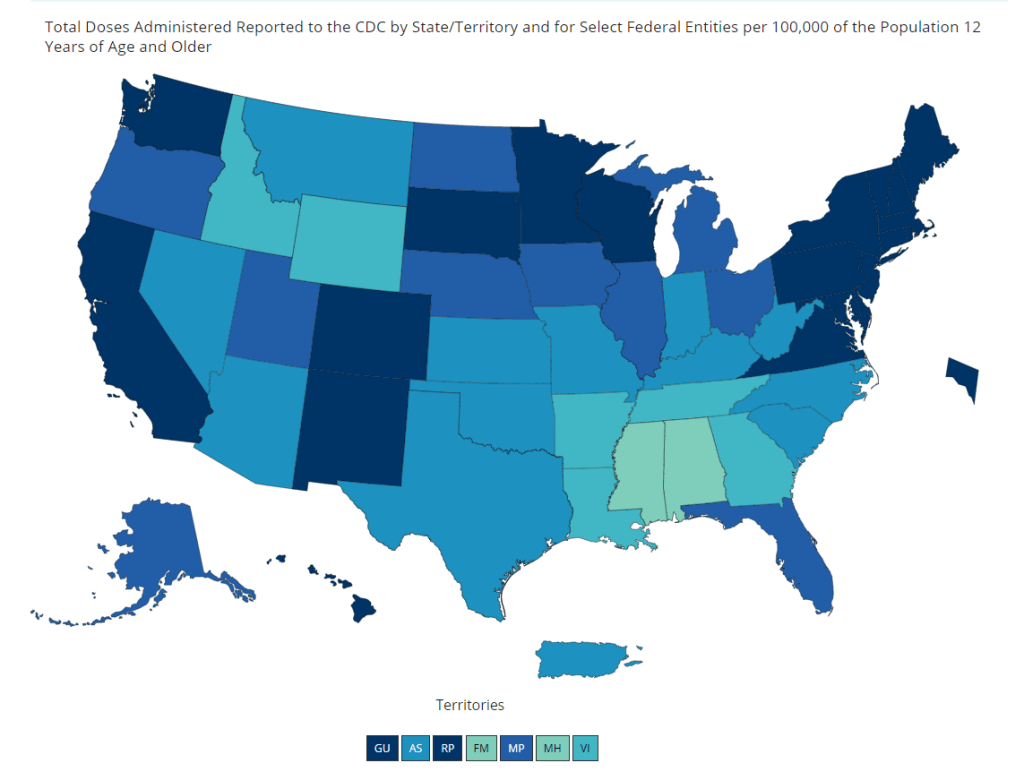
The data indicate that, despite promises from the White House to prioritize vulnerable communities in the vaccination campaign, a lot of inequities persist: “KHN’s analysis shows that only 22% of Black Americans have gotten a shot, and Black rates still trail those of whites in almost every state.”
!function(){“use strict”;window.addEventListener(“message”,(function(a){if(void 0!==a.data[“datawrapper-height”])for(var e in a.data[“datawrapper-height”]){var t=document.getElementById(“datawrapper-chart-“+e)||document.querySelector(“iframe[src*=’”+e+”‘]”);t&&(t.style.height=a.data[“datawrapper-height”][e]+”px”)}}))}();In some states, white residents have been vaccinated at almost twice the rate of Black residents. In Iowa, for example, 15% of the Black population has received at least one dose—compared with 37% of the white population. Other states with high disparities include Florida, New Hampshire, Maine, Wisconsin, New Jersey, New York, Hawaii, and Connecticut.
Hispanic/Latino vaccination rates also lag behind the rates for white residents in some states, but the disparities are not as drastic as those for the Black population. Nationwide, 22% of Black Americans have received at least one dose, compared to 33% of white Americans.
Both Native Americans and Asian Americans have higher vaccination rates than the white population. Many tribes, in particular, have made dedicated efforts to promote vaccination.
And another hopeful caveat: vaccination rates for minorities have improved in recent weeks as the rate for white Americans goes down. In the last two weeks, about half of first doses administered in the U.S. have gone to people of color. This includes about 24% of doses going to Hispanic/Latino Americans, 10% going to Black Americans, and 8% going to Asian Americans.
The day after KHN’s analysis was published, Victoria Knight (another KHN reporter) asked CDC Director Dr. Rochelle Walensky whether the agency would add state-level race and ethnicity vaccination data to its dashboard.
“We have been updating our website,” Dr. Walensky said in response. “I can’t say that it’s daily; I believe that it’s weekly.”
And yet as of Sunday morning, May 23, state-by-state demographic data are nowhere to be found on the CDC’s site.
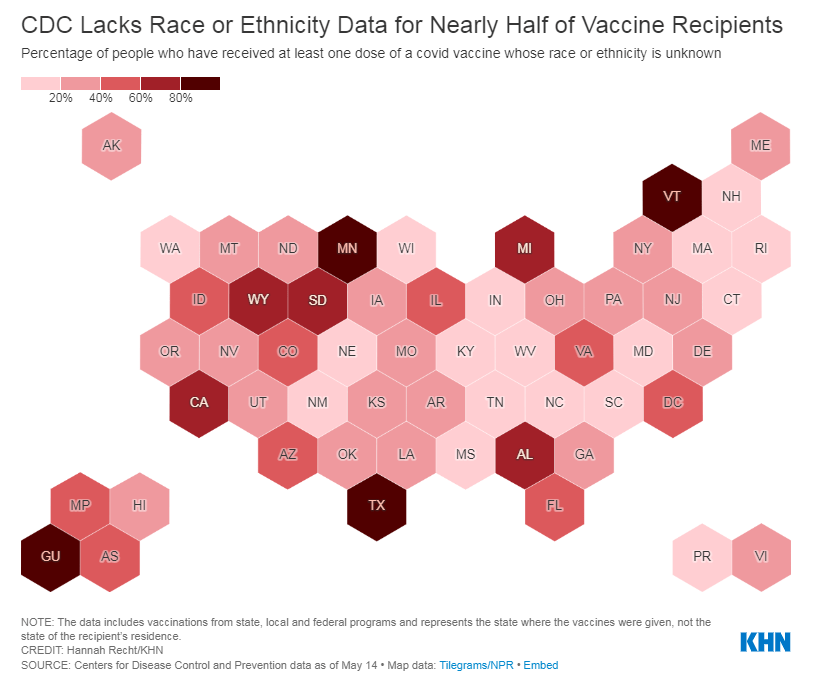
Knight also asked what the CDC is doing to address the high number of vaccinations for which demographic details are unknown. Race/ethnicity data are missing for about 44% of vaccinated Americans, meaning that true disparities may be even starker.
!function(){“use strict”;window.addEventListener(“message”,(function(a){if(void 0!==a.data[“datawrapper-height”])for(var e in a.data[“datawrapper-height”]){var t=document.getElementById(“datawrapper-chart-“+e)||document.querySelector(“iframe[src*=’”+e+”‘]”);t&&(t.style.height=a.data[“datawrapper-height”][e]+”px”)}}))}();In some states, that unknown percentage is much higher than 44%. Eight states “either refuse to provide race and ethnicity details to the CDC or are missing that information for more than 60% of people vaccinated,” according to KHN. These states are excluded from KHN’s analysis as a result: they are Alabama, California, Michigan, Minnesota, South Dakota, Texas, Vermont and Wyoming.
Dr. Walensky told reporters the CDC is working with state and local public health departments to improve demographic reporting, but didn’t provide specifics.
In order to continue improving vaccination rates for minority communities, the CDC needs to actually make all of the agency’s data public. If state-by-state demographic data were easily available, researchers and reporters like me could more easily identify both the success stories and the disappointments—and help the states that are lagging catch up.
As Hannah Recht put it on Twitter: “we should not have to keep FOIAing for CDC state-level data that they could just put online if they wanted to.”
More vaccine reporting
- Sources and updates, November 12Sources and updates for the week of November 12 include new vaccination data, a rapid test receiving FDA approval, treatment guidelines, and more.
- How is the CDC tracking the latest round of COVID-19 vaccines?Following the end of the federal public health emergency in May, the CDC has lost its authority to collect vaccination data from all state and local health agencies that keep immunization records. As a result, the CDC is no longer providing comprehensive vaccination numbers on its COVID-19 dashboards. But we still have some information about this year’s vaccination campaign, thanks to continued CDC efforts as well as reporting by other health agencies and research organizations.
- Sources and updates, October 8Sources and updates for the week of October 8 include new papers about booster shot uptake, at-home tests, and Long COVID symptoms.
- COVID source shout-out: Novavax’s booster is now availableThis week, the FDA authorized Novavax’s updated COVID-19 vaccine. Here’s why some people are excited to get Novavax’s vaccine this fall, as opposed to Pfizer’s or Moderna’s.
- COVID-19 vaccine issues: Stories from COVID-19 Data Dispatch readers across the U.S.Last week, I asked you, COVID-19 Data Dispatch readers, to send me your stories of challenges you experienced when trying to get this fall’s COVID-19 vaccines. I received 35 responses from readers across the country, demonstrating issues with insurance coverage, pharmacy logistics, and more.