- New vaccination data from the CDC: The CDC has started publishing vaccination data reflecting how many Americans have received COVID-19, flu, and RSV shots in fall 2023. These numbers are estimates, based on the CDC’s National Immunization Survey, as the agency is no longer directly compiling COVID-19 vaccinations from state and local health agencies. (See this post from last month for more details.) According to the estimates, about 28% of American adults have received a 2023 flu shot, compared to 10% who have received a 2023 COVID-19 shot. The numbers reflect poor communication about and accessibility challenges with this year’s COVID-19 vaccines.
- FDA approves a rapid COVID-19 test: Following the end of the federal public health emergency this spring, the FDA has advised companies that produce COVID-19 tests to submit their products for full approval, transitioning out of the emergency use authorizations that these tests received earlier in the pandemic. The FDA has now fully approved an at-home COVID-19 test: Flowflex’s rapid, antigen test. This is the second at-home test to receive approval, following a molecular test a few months ago. The Floxflex test “correctly identified 89.8% of positive and 99.3% of negative samples” from people with COVID-like respiratory symptoms, according to a study that the FDA reviewed for this approval.
- WHO updates COVID-19 treatment guidance: This week, the World Health Organization updated its guidance on drugs and other treatment options for severe COVID-19 symptoms. A group of WHO experts has regularly reviewed the latest evidence and updated this guidance since fall 2020. The update includes guidelines on classifying COVID-19 patients based on their risk of potential hospitalization, recommendations for drugs such as nirmatrelvir and corticosteroids, and recommendations against other drugs such as invermectin and hydroxychloroquine. Clinicians can explore the guidance through an interactive tool that summarizes the expert group’s findings.
- Gargling with salt water to reduce symptoms: Speaking of COVID-19 treatments: gargling with salt water may help people with milder COVID-19 symptoms recover more quickly, according to a new study presented at the American College of Allergy, Asthma and Immunology’s annual conference. The researchers compared COVID-19 outcomes among people who did and did not use salt water for 14 days while sick; those who used the treatment had lower risks of hospitalization and reported shorter periods of symptoms. This study has not yet been peer-reviewed and more research will be needed, but it’s still helpful evidence to back up salt water as a potential treatment (something I’ve personally seen recommended anecdotally in the last couple of years).
- Allergies as potential Long COVID risk factors: Another study that caught my attention this week: researchers at the University of Magdeburg in Germany conducted a review of connections between allergies and Long COVID. The researchers compiled data from 13 past papers, including a total of about 10,000 study participants. Based on these studies, people who have asthma or rhinitis (i.e. runny nose, congestion, and similar symptoms, usually caused by seasonal allergies) are at higher risk for developing Long COVID after a COVID-19 case. The researchers note that this evidence is “very uncertain” and more investigation is needed; however, the study aligns with reports of people with Long COVID getting diagnosed with mast cell activation syndrome (or MCAS, an allergy-related condition).
- Dropping childhood vaccination rates: One more notable study, from the CDC’s Morbidity and Mortality Weekly Report (MMWR): vaccination rates for common childhood vaccines are declining among American kindergarteners, according to CDC research. CDC scientists reviewed data reflecting the childhood vaccinations that are required by 49 states and D.C. for the 2022-23 school year, and compared those numbers to past years. Overall, 93% of kindergarteners had completed their state-required vaccinations last school year, down from 95% in the 2019-20 school year, while vaccine exemptions increased to 3%. In 10 states, more than 5% of kindergarteners had exemptions to their required vaccines—signifying increased risk of vaccine-preventable disease outbreaks in schools, according to the CDC.
Tag: WHO
-
Sources and updates, November 12
-
WHO ends the global health emergency for COVID-19
As the U.S. gears up to end its federal public health emergency for COVID-19, the World Health Organization just declared an end to the global health emergency. WHO Director-General Tedros Adhanom Ghebreyesus announced the declaration on Friday, following a meeting of the organization’s COVID-19 emergency committee the day before.
Here’s what this declaration means, pulling from Helen Branswell’s article in STAT News and Katelyn Jetelina’s Your Local Epidemiologist post:
- The world is at a point of transition from considering COVID-19 an unexpected emergency to considering it a part of our daily lives, a disease that we’ll be dealing with in the long term.
- The WHO will have fewer resources for an international response to COVID-19, such as coordinating between countries and sharing data at a global scale.
- The WHO will also have less authority when it comes to issuing international guidance to control COVID-19 spread.
- There will be fewer incentives for countries to accelerate vaccines, treatments, and tests for COVID-19.
The declaration does not mean that COVID-19 is “over.” We have plenty of long-term issues to deal with here: millions suffering from Long COVID, continued COVID-19 waves around the world, potential new variants, healthcare worker shortages, and declines in childhood vaccination rates, to name a few. Tedros may set up a new committee to make recommendations on long-term COVID-19 management, according to Branswell’s article.
In fact, the WHO recently publicized the impacts of Long COVID: Tedros delivered a PSA explaining that one in ten coronavirus infections leads to some form of Long COVID, and suggesting that “hundreds of millions of people will need longer-term care.” Shifting out of the emergency phase of our global COVID-19 response should be a call to action for scientists and health experts to now focus on Long COVID needs.
Still, a lot of people might interpret the WHO’s declaration as an announcement that they no longer need to worry about COVID-19. Some mainstream publications that have covered the change haven’t done a great job of conveying the nuances here, and I’ve already seen some misinterpretation on social media.
COVID-19 may not be an emergency at this point. But we’re probably going to be living with it for the rest of our lives, and there’s a lot of work left to do.
More on international data
-
Sources and updates, March 19
- Long-term effects of COVID-19 on kids: The National Academies of Sciences, Engineering, and Medicine (NASEM) recently published a report about how the COVID-19 pandemic has impacted children and families. It includes a variety of health impacts (physical, behavioral, mental), interventions taken by schools and other institutions, access to healthcare coverage, impacts of COVID-related economic policies, and recommendations for addressing this issue in the future. The report’s authors note that, for “almost every outcome” related to health and well-being, COVID-19’s impacts were worse for Black, Hispanic/Latino, Native American, and low-income families.
- Shorter sleep duration during the pandemic: On a similar topic: the CDC’s Preventing Chronic Disease journal recently published an article about teenagers’ sleep habits during the pandemic. The study used data from the 2021 Adolescent Behaviors and Experiences Survey, a nationally-representative survey of high school students. About three-quarters of students surveyed slept for less than eight hours a night, and students who slept less were more likely to report that doing their schoolwork became more difficult during the pandemic. While shorter sleep was becoming an issue before COVID-19, this study shows how COVID-related stress may have exacerbated the problem.
- Maternal mortality keeps getting worse: This week, the CDC released its most recent, official statistics on maternal mortality in the U.S. The new data reflect deaths in 2021, and show that mortality rates rose to about 33 deaths per 100,000 births, compared to rates closer to 20 per 100,000 births in 2020 and 2019. Mortality rates were more than 2.5 times higher for Black women compared to white women. For more recent data (and additional demographic figures), see this story and GitHub repository from MuckRock, also shared in last week’s newsletter.
- WHO updates its variant tracking system: The World Health Organization announced on Thursday that it will start classifying subvariants of Omicron as distinct Variants of Interest (VOIs) and Variants of Concern (VOCs), and will assign new Greek-letter names to VOCs. Omicron lineages have accounted for the vast majority of coronavirus circulating globally since early 2022, but all subvariants have previously been clustered under that one Greek-letter name. Now, the WHO will give us new names as needed, hopefully making future variants a bit easier to talk about. The WHO also updated its definitions for classifying new subvariants as VOCs or VOIs.
- Wastewater monitoring continues to expand: Two updates about local wastewater surveillance programs caught my attention this week. First, the City of Chicago’s public health department has announced it will start monitoring wastewater for polio, in collaboration with the University of Illinois, state health department, and national CDC. And second, two local agencies in the Bay Area, California recently started testing wastewater for traces of drugs, including fentanyl, methamphetamine, cocaine, and nicotine. We’ll likely see more announcements like this across the U.S. as agencies continue to expand their wastewater surveillance programs beyond COVID-19.
-
Sources and updates, January 29
- New York State expands wastewater surveillance program: This week, the New York State health department announced a major investment in the state’s wastewater surveillance program: the program has received a $6.6 million grant from the CDC and $15 million from the governor (over the next three years). With this investment, New York’s wastewater surveillance network will grow from 125 to 215 testing sites and will expand from COVID-19 to include flu, RSV, hepatitis, norovirus, and antimicrobial resistance. This is great news for New York—I hope to see other states make similar investments.
- Bivalent boosters vs. XBB lineages: The bivalent, Omicron-specific booster shots provide some protection against XBB.1.5 and related Omicron subvariants, according to a new study published this week in the CDC’s Morbidity and Mortality Weekly Report. CDC researchers used data from COVID-19 testing at pharmacies to compare results among people who had received the new booster and those who hadn’t. Booster recipients were significantly less likely to have a symptomatic XBB/XBB.1.5 infection compared to people who hadn’t received the shot, the researchers found (with a vaccine effectiveness value of 48%). While the boosters work less well against XBB.1.5 than they did against BA.4/BA.5, they’re still a valuable protective measure.
- CDC overhauling data communications: The CDC is creating new internal offices that will change how it processes, publishes, and communicates about data, according to POLITICO. The new offices include an Office of Health Equity and an Office of Public Health Data, Surveillance, and Technology—both of which have new acting directors as of this week. It’s currently unclear what the new offices will do, exactly, or how they will improve upon a fractured nationwide health data system (with decisions about how to store and share key data largely left up to state agencies and private companies). Still, it’s good to see movement on the CDC’s efforts.
- WHO deliberates ending the global health emergency: On Friday, a World Health Organization committee met to discuss whether the official global health emergency over COVID-19 should be ended. The committee’s decision will be made public tomorrow, as a recommendation to WHO Director-General Tedros Adhanom Ghebreyesus; Tedros will ultimately decide whether or not to end the emergency. Global health experts who spoke to STAT reporter Helen Branswell suggested that the WHO likely isn’t ready to end this emergency yet, but it may happen later in 2023.
- KFF compiles Long COVID data: A new report from the Kaiser Family Foundation compiles and provides context for Long COVID data reported by the Census and CDC’s Household Pulse Survey. The share of people who reported ever having Long COVID symptoms following a COVID-19 case has declined slightly over time, the KFF report finds; this number went from 35% in June 2022 to 28% in January 2023. However, the number is still high and Long COVID can be debilitating for many, as 79% of people with Long COVID report limitations to their day-to-day activities.
- Health of Congressional Districts: Finally: a new dashboard, published this week by researchers at NYU Langone Health, provides detailed health metrics for all 435 Congressional districts in the U.S. (plus Washington, D.C.). The dashboard is a helpful source for researchers and policymakers looking to understand health patterns in specific districts. One of its key metrics is a “COVID Local Risk Index” that reflects the risk residents face for severe health, social, and economic outcomes of COVID-19.
-

We failed to vaccinate the world in 2021; will 2022 be more successful?
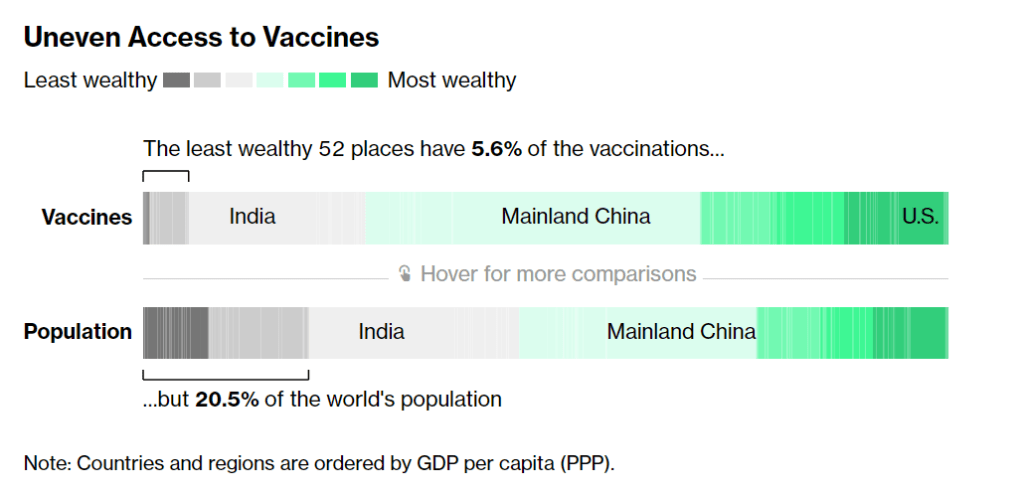
According to Bloomberg, the 52 least wealthy places in the world have 5.6% of the vaccinations. Chart from Bloomberg’s vaccine tracker, screenshot taken on December 19. In January, COVAX set a goal that many global health advocates considered modest: delivering 2.3 billion vaccine doses to low- and middle-income countries by the end of 2021. COVAX (or COVID-19 Vaccines Global Access) is an initiative to provide equitable access to vaccines; its leadership includes the United Nations, the World Health Organization (WHO), and other organizations.
Despite COVAX’s broad support, the initiative has revised its vaccine delivery projections down again and again this year. Now, the initiative is saying it’ll deliver just 800 million vaccine doses by the end of 2021, according to the Washington Post, and only about 600 million had been delivered by early December.
Considering that most COVID-19 vaccines are two-dose series—and boosters will likely be necessary to combat Omicron—those doses are just a drop in the bucket. According to Bloomberg’s vaccine tracker: “The least wealthy 52 places have 5.6% of the vaccinations, but 20.5% of the world’s population.”
Why this access gap? Many scientists and advocates in low- and middle-income nations blame vaccine manufacturers and rich countries like the U.S., I found when I reported a story on this topic for Popular Science.
“We basically have artificial scarcity of vaccine doses,” says Robbie Silverman, a vaccine advocate at Oxfam America. The pharmaceutical companies control “where doses are produced, where they’re sold, and at what price.” The world’s vaccine supply is thus limited by contracts signed by a small number of big companies; and many of those contracts, [Fatima Hassan, health advocate from South Africa] says, are kept secret behind non-disclosure agreements.
While rich countries claimed to support COVAX, the Washington Post reports, “they also placed advance orders with vaccine manufacturers before COVAX could raise enough money to do so.” This practice pushed COVAX to the back of the vaccine line—and then, when rich countries decided they needed booster shots, that pushed COVAX to the back of the line again. India’s spring 2021 surge didn’t help either, as the country blocked vaccine supplies produced at the Serum Institute of India from being exported to other nations.
According to Our World in Data, low-income nations have administered about 60 million doses total, while high-income nations have administered more than 300 million booster shots. At times this winter, there were more booster shots administered daily than first and second doses in low-income countries.
Even taking booster shots into consideration, there should be enough vaccine supplies produced by the end of this year to vaccinate 40% of the world’s population by the end of this year, meeting WHO targets, according to STAT News’ Olivia Goldhill. The world is on track to manufacture about 11 billion vaccines in total this year, Goldhill reports, while about 850 million doses are needed to get all countries to a 40% vaccination benchmark.
But again, rich countries pose a problem: the countries currently focused on administering booster shots have stockpiled hundreds of millions of doses, and are unwilling to send their stockpiles abroad. From STAT News:
“That number can be redistributed from what high-income countries expect to have by the end of this year. So it’s not an overall supply challenge,” said [Krishna Udayakumar, founding director of Duke’s Global Health Innovation Center]. “It’s very much an allocation challenge, as well as getting high income countries more and more comfortable that they don’t need to hold on to hundreds of millions of doses, for contingencies.”
The vaccine shortage for low-income countries is less than the surplus vaccines within the G7 countries and the European Union, according to separate analyses from both Duke and Airfinity, a life sciences analytics firm that is tracking vaccine distribution.
While leaders in the U.S., the U.K., and other nations with large stockpiles maintain that they can both administer booster shots at home and send doses for primary series shots abroad, their true priorities are clear. The U.S., for example, has pledged to donate 1.2 billion doses to other countries, but about 320 million—under one-third—of those doses have been shipped out so far.
Another challenge is the type of vaccines being used in wealthy nations, as opposed to low- and middle-income nations. Wealthy nations have been particularly eager to horde Pfizer and Moderna’s vaccines, which are more effective against Omicron and other variants of concern. On the other hand, many low-income nations have relied on Sputnik, CoronaVac, and other vaccines which are less effective.
“We’re now entering an era of second-class vaccines for second-class people,” Peter Maybarduk, director at the DC-based nonprofit Public Citizen, told me in October, discussing these differences in vaccine effectiveness. As Omicron spreads around the world, this concern is only growing.
The more the coronavirus spreads across the world, particularly in regions with less immunity from vaccines, the more it can mutate and create new variants. Delta and Omicron provide clear examples, demonstrating the need to vaccinate the world in 2022.
And there are some reasons to hope that this goal may be feasible. COVAX’s global supply forecast shows major jumps in vaccine supplies in the first three months of 2022. At the same time, vaccine companies are increasing their production capacity, and donations from the U.S. and other countries are expected to kick in. In South Africa, an mRNA vaccine hub is working to train African companies to manufacture COVID-19 vaccines similar to Pfizer and Moderna’s, without violating patents.
Still, additional variants—and the need for additional booster shots—could be a major hurdle, as vaccine companies continue to prioritize wealthy nations. These companies continue to refuse to share their intellectual property with other manufacturers, even as they make patents for COVID-19 antiviral drugs widely available. And, once vaccines are delivered, getting them from shipments into arms will be a challenge.
More international data
-
Featured sources, July 25
- 2021 Health Disparities Report by America’s Health Rankings: This source isn’t specific to COVID-19, but it may be invaluable for reporting on the disparities worsened by the pandemic. America’s Health Rankings has put together comprehensive reports on national health data for decades; this is the first report to focus specifically on social determinants of health, including social, economic, physical environment, and other factors.
- COVID-19 Orphanhood Calculator: Researchers at Imperial College London built this dashboard to track one of the most dire consequences of the pandemic: children who lost their parents or primary caregivers to COVID-19. That group includes more than 1.5 million children worldwide, according to a recent study by the same researchers. The estimates are based on COVID-19 mortality data and fertility data.
- WHO COVID-19 Detailed Surveillance Data Dashboard: The World Health Organization has a new COVID-19 dashboard, and it’s incredibly detailed. Here, you can find testing data, case fatality ratios, cases and deaths by age, healthcare worker data, and more for all WHO member nations.