On Friday morning, the FDA authorized booster shots of Pfizer’s and Moderna’s COVID-19 vaccines for all adults in the U.S., six months after their first two doses. The CDC’s vaccine advisory committee voted to support this expanded booster eligibility that afternoon, and CDC leadership signed off on it a few hours later.
Although the Biden administration has supported boosters for all adults since August, this specific federal eligibility expansion was preceded by several state and local leaders. Prior to Friday, the governors of Colorado, New Mexico, California, and other states said that any adult living in their jurisdictions could go get a booster, even if they didn’t fit the current national criteria. New York City leaders made a similar announcement this past Monday.
Perhaps spurred on by these state decisions, the FDA and CDC moved quite quickly to authorize booster shots for a larger group of Americans. The FDA was originally just considering the move for Pfizer’s vaccine, then added Moderna to the mix just this week (when Moderna sent in a formal application).
And the CDC’s vaccine advisory committee meeting had somewhat less time for deliberation than this committee typically tends to take. As Helen Branswell wrote in STAT News:
The meeting was called on such short notice — it was announced Tuesday — that only 13 of the committee’s members were able to attend. When the meeting went longer than scheduled, two members had to leave without voting.
I discussed expanded booster shot eligibility this week in a FiveThirtyEight Chat with editor Chadwick Matlin and science writer Maggie Koerth. Today at the COVID-19 Data Dispatch, I’d like to expand on the ideas in that chat piece, and attempt to answer a couple of other questions.
Why expand booster eligibility to all adults?
The short answer here is 1) more compelling evidence that boosters provide additional protection against coronavirus infection and 2) cases are rising in the U.S., and boosters might help make the surge less severe. Also, so far, very few cases of severe side effects have been reported following booster shots.
Since the last FDA and CDC booster shot deliberations, more evidence has rolled in showing their efficacy. One notable study, from the Imperial College of London, was published this past Wednesday; the report suggests that people who’ve received two COVID-19 vaccine doses are more than twice as likely to test positive than those who’ve received three doses.
While the study hasn’t yet been peer-reviewed, it’s part of a long-running surveillance project in the U.K. that examines COVID-19 prevalence in the entire population—including all age groups and comparing those who received Pfizer and AstraZeneca vaccines. “What they found is very, very strong data showing that as soon as 7 days after a third COVID-19 vaccine dose, the risk of infection is cut in half when you look at the entire population,” wrote Dr. Jorge Caballero in a Twitter thread summarizing the study.
At the same time, cases are going up in the U.S.—appearing to indicate a new winter surge. It’s no coincidence that Colorado and New Mexico, two of the states that were among the first to expand booster eligibility to all adults, are also among the states with the highest COVID-19 case rates.
When Delta hit Israel this past summer, the country started administering booster shots: first to seniors at the end of July, then for younger and younger age groups until all adults were able to get the shots. Data from the country’s national health agency suggest that these booster shots played a key role in driving down case numbers among both vaccinated and unvaccinated Israelis.
Personally, I am still a bit skeptical that Israel’s drop in cases was thanks to booster shots alone, as the data don’t necessarily show causation. But for a lot of U.S. leaders, the Israeli data provide a compelling model: it seems like booster shots can potentially drive down a case surge. This fits nicely into the national strategy that the Biden administration has already been preaching for months, which I call “vaccinate out of the pandemic.”
Here’s how I explained it in the FiveThirtyEight chat piece:
Listening to the advisory-committee meetings, I noticed that there seems to be this tension between the scientific experts who want to make robust evidence-based decisions — and the sense that, here in the U.S., our overall pandemic strategy is basically “vaccinate our way out of the pandemic.” If we had better masking, distancing, contact tracing, ventilation, rapid tests and everything else, we would not need boosters to stop people’s mild cases. But we’re not doing a great job at any of those other things, so … we kinda need boosters.
Maggie Koerth also pointed out that booster shots are also politically easier for a lot of leaders than some of the other COVID-19 strategies I mentioned. We already have the shots stockpiled, so it’s just a matter of telling people to go get them—unlike, say, expanding contact tracing, which would take a huge investment in hiring and training people.
In addition, the eligibility expansion solves communication and logistics challenges: now, every adult in the U.S. can just go get a booster shot, once enough time has passed from their first two doses. Almost 90% of vaccinated Americans were eligible already, but a lot of people were confused about whether they fit the criteria; the situation became much simpler after Friday.
Should you get a booster shot?
If you’re over 65 or you have a health condition that makes you particularly vulnerable to severe COVID-19 symptoms, answering this question is easy: YES. Go get a booster shot, as soon as you’re able to do so.
If you live or work in a setting that puts you at risk of contracting the coronavirus—or if you live or work in a setting with other people who are more vulnerable than you—then you also have a pretty solid argument towards getting a booster shot.
Even if you’re very unlikely to have a severe case of COVID-19 thanks to your initial vaccination, a mild case could still disrupt your work, your household, and others in your community. A teacher with breakthrough COVID-19 might cause their classroom to shut down for a week, for example, while a parent with breakthrough COVID-19 may interrupt their kids’ lives if those kids are too young to be vaccinated themselves.
For those who don’t fall into these categories (like me!), the situation is a bit more complicated. But after following all of the news this week, I’ve decided that it does make sense for me to get my booster shot.
Here’s why: much as I wish that national leadership and my own local leaders in NYC were investing in other measures to control COVID-19 cases, I don’t foresee widespread mask mandates, rapid tests, contact tracing, or any other safety overhauls anytime soon. Instead, my public health leaders are asking me (and those around me) to get booster shots in order to potentially lower case rates. So, I’ll do my part to contribute to that “vaccinate out of the pandemic” strategy, though I don’t necessarily agree with it.
It’s also important to note here that vaccinating the people who are still unvaccinated is much more important for lowering overall case counts—and for keeping people out of the hospital—than boosters. That includes kids in the 5 to 11 age group. As Maggie Koerth said in our chat:
If you’re under 65 and you’re not immune compromised, it almost certainly matters more to get your kiddos vaxxed the first time than to get yourself a booster. That’s my parent-centric takeaway from all this reading.
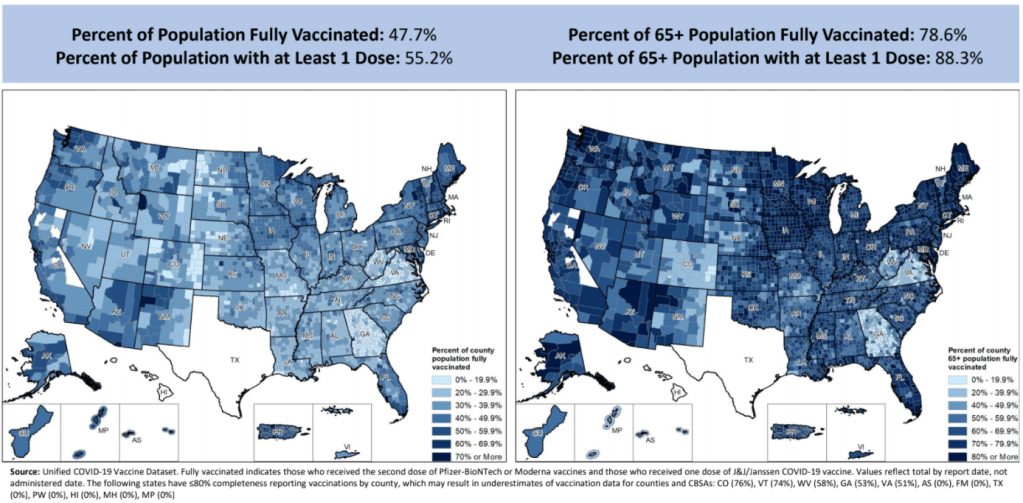
And, of course, to end the pandemic on a global scale, we need to get first and second doses to everyone in the world. Right now, booster shots are hindering global vaccination: according to the WHO, there are about six times more boosters administered daily in wealthy nations right now than there are first and second doses administered in low-income nations.
The U.S. has already chosen to stockpile millions of doses for boosters, so refusing a booster shot on an individual level doesn’t have any impact on the global situation. But there are other options for people who want to take action about vaccine inequality: for example, you can contact your congressional representatives about the issue.
What happens after a lot of Americans get booster shots?
Someone asked me this question on Twitter earlier this week. Do booster shots lead to other loosening COVID-19 restrictions, or something else?
It’s difficult to answer that right now, because the U.S. is still close to the beginning of our booster shot rollout. Within a couple of months—and millions more doses—we’ll have some data on whether booster shots here lead to a drop in cases, like what we saw in Israel. At the same time, many European countries are similarly offering booster shots to wide swaths of their populations; we can also watch what happens in those nations.
The U.S. is still likely to face a case surge this holiday season, I think, simply due to cold weather combined with travel and gatherings. But perhaps booster shots will mean that hospitalizations don’t rise as much as cases do, or that a higher share of the cases are mild. We’ll have to see.
Looking beyond this winter, we could see three shots become standard for COVID-19 vaccines. (Several other vaccines, such as HPV, are three-shot series.) We could also see annual boosters for COVID-19, similar to flu shots. More study of the booster shots’ effectiveness and of long-term COVID-19 immunity in general will help scientists figure this out.
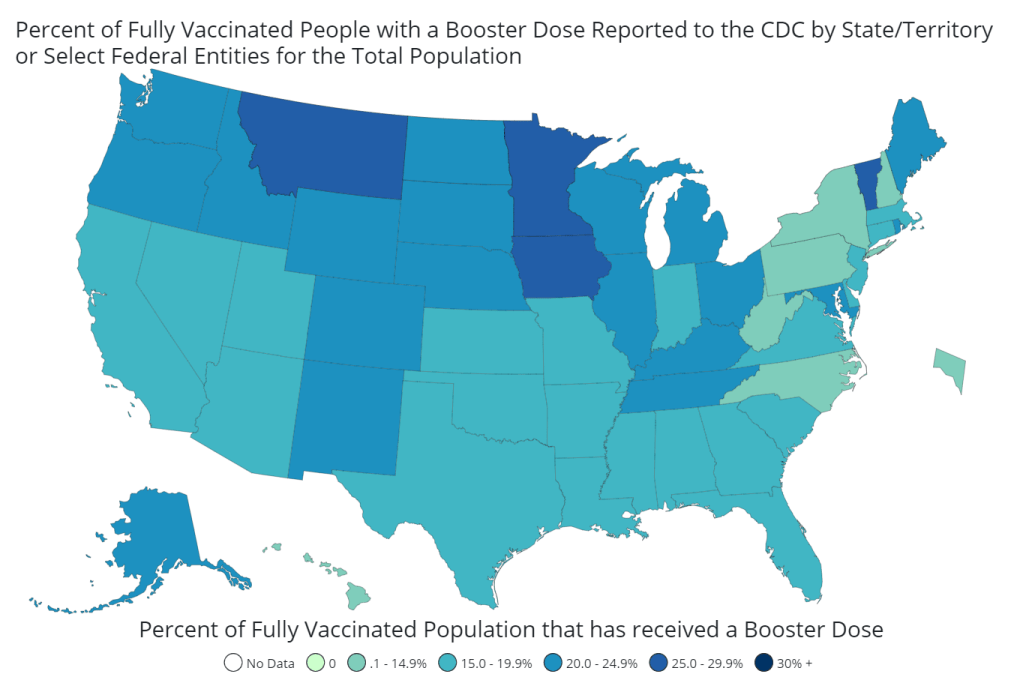
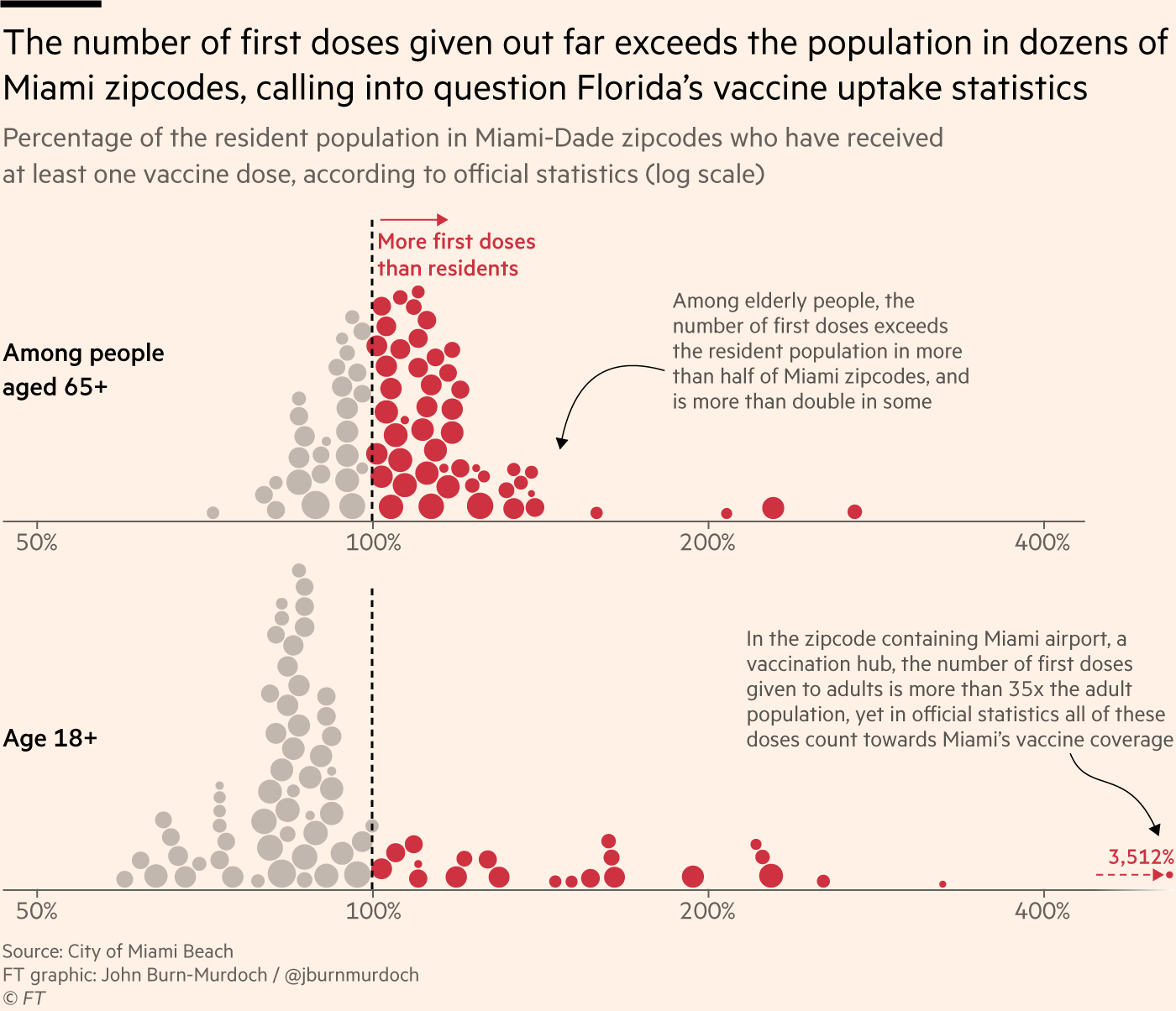
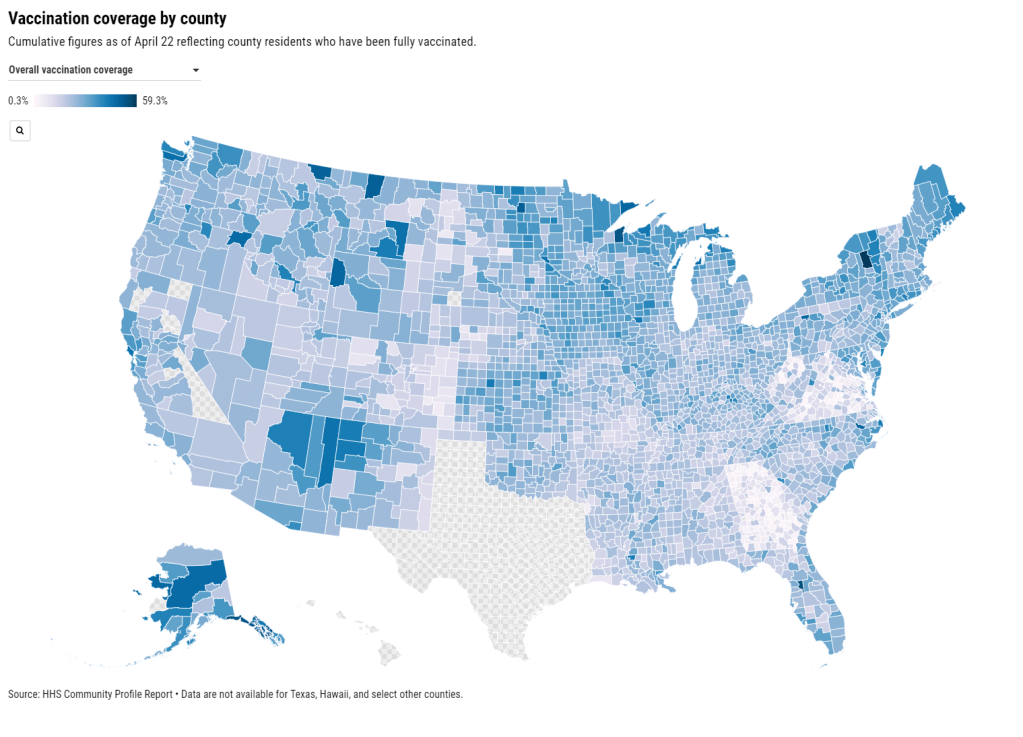
Finally, I couldn’t end this post without pointing out the continued data gaps here. The U.S. is still not tracking breakthrough cases in any kind of comprehensive manner, and a lot of information is missing on who’s getting booster shots—the CDC and most states are not reporting demographic data on booster recipients.
To quote Dr. Katelyn Jetelina from her recap of Friday’s CDC advisory committee meeting:
And this is it. This [three small studies] is all the data the CDC presented today. Which is insane— the United States does not have a real-time, comprehensive picture of our vaccines, nor the number of breakthrough cases, nor who’s more likely to have a breakthrough case or not. I cannot emphasize enough of how detrimental this is to our public health response. Bad data produces (potentially) bad policy. We are flying blind.