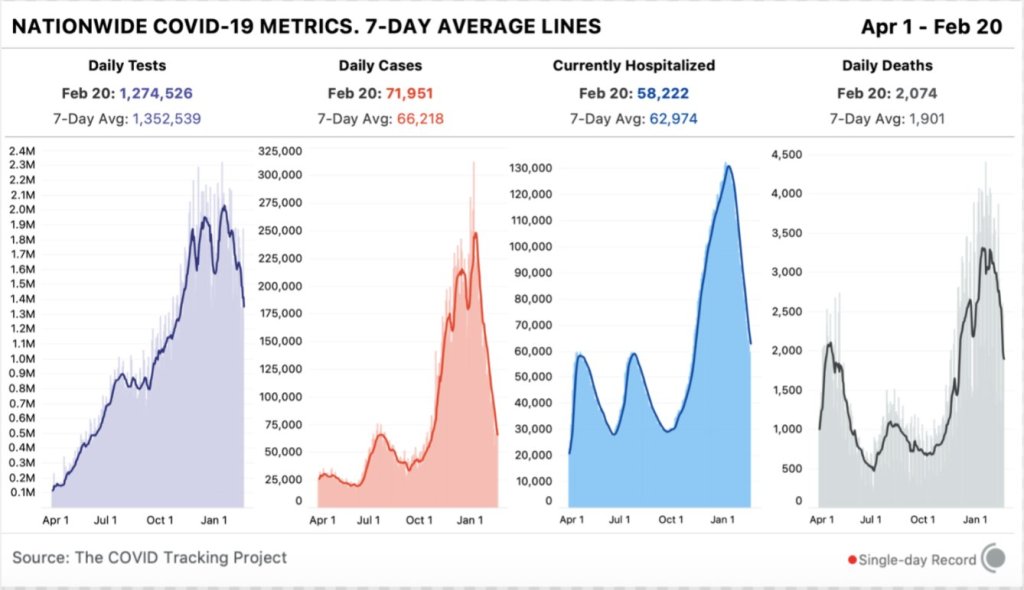
In the past week (February 14 through 20), the U.S. reported about 464,000 new cases, according to the COVID Tracking Project. This amounts to:
- An average of 66,000 new cases each day
- 141 total new cases for every 100,000 Americans
- 1 in 708 Americans getting diagnosed with COVID-19 in the past week
- About two-fifths of the new cases reported in the week of January 23
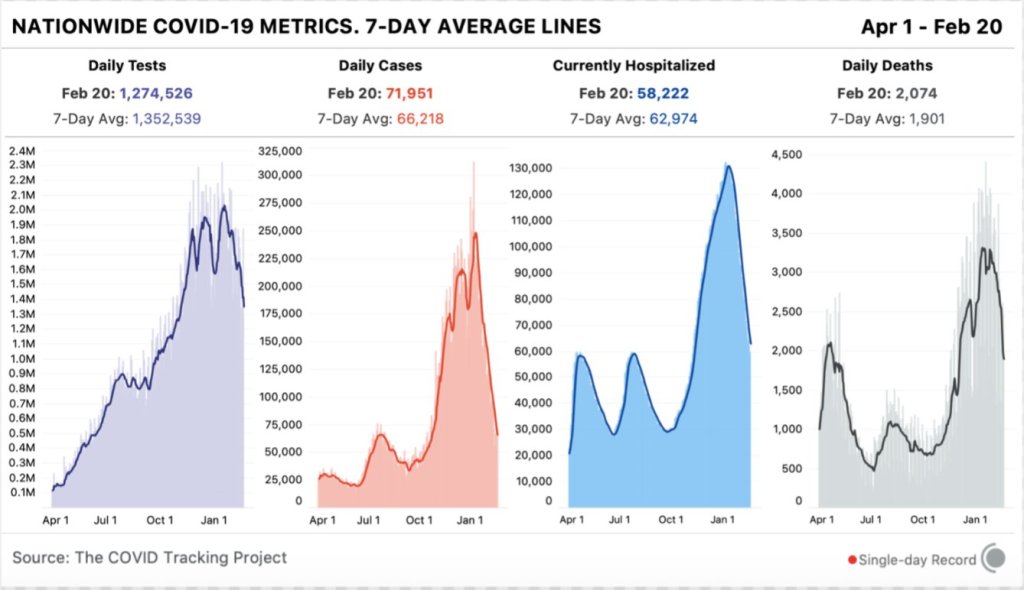
Last week, America also saw:
- 58,200 people now hospitalized with COVID-19 (18 for every 100,000 people)
- 13,300 new COVID-19 deaths (4.1 for every 100,000 people)
- An average of 1.49 million vaccinations per day (per Bloomberg)
The number of COVID-19 patients in U.S. hospitals is now the lowest it’s been since early November. About 7,000 new patients were admitted each day this week—while this is still a huge number, it’s a notable drop from the peak (18,000 per day) we saw earlier in the winter.
I got those new hospital admission numbers from the COVID Data Tracker Weekly Review, a new report that the CDC recently started publishing in conjunction with its COVID-19 dashboard. It’s kind-of like a longer, more numbers-heavy, less snarky version of this newsletter segment.
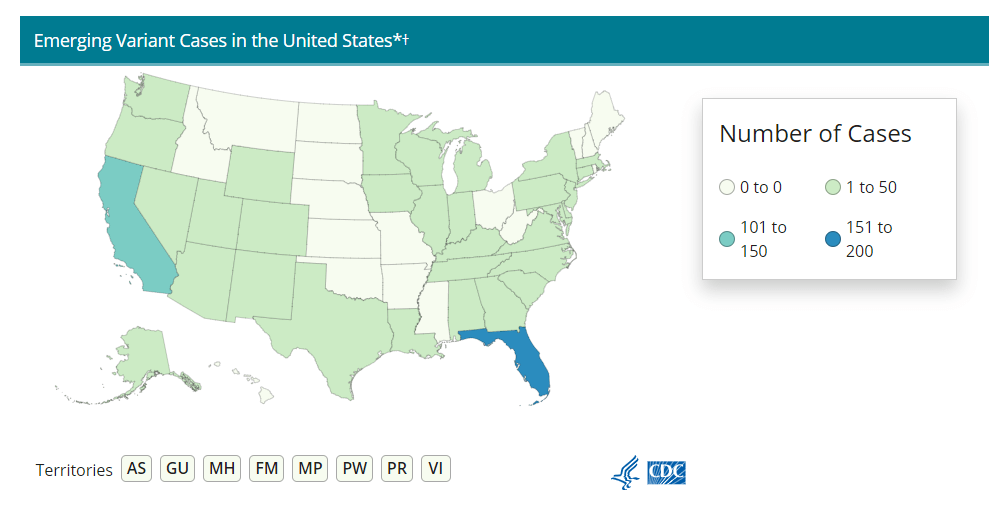
The Weekly Review this past Friday also highlighted the progression of coronavirus variants in the U.S. We’ve now detected over 1,500 cases of B.1.1.7 (the variant originating in the U.K.), as well as 21 cases of B.1.351 (originated in South Africa) and 5 cases of P.1 (originated in Brazil). While sequencing efforts have increased significantly in the past few weeks, these numbers are likely still massive undercounts. The CDC encourages Americans to “stop variants by stopping the spread.” In other words, all the behaviors we’ve been using to keep ourselves and our communities safe from spreading the virus will also help reduce its opportunities to mutate.
One more piece of good news from this week’s COVID-19 data: vaccinations may already be having an impact in nursing homes and other long-term facilities. The share of deaths occurring in these facilities dropped under 20% this week, for the first time since the COVID Tracking Project started collecting these data.
The pace of vaccinations was slowed this week thanks to winter storms across the South and Midwest. But this news from LTC facilities is a hopeful note of how elderly Americans may be more protected in the weeks to come.