In the past week (March 5 through 11), the U.S. reported about 260,000 new COVID-19 cases, according to the CDC. This amounts to:
- An average of 37,000 new cases each day
- 79 total new cases for every 100,000 Americans
- 29% fewer new cases than last week (February 26-March 4)
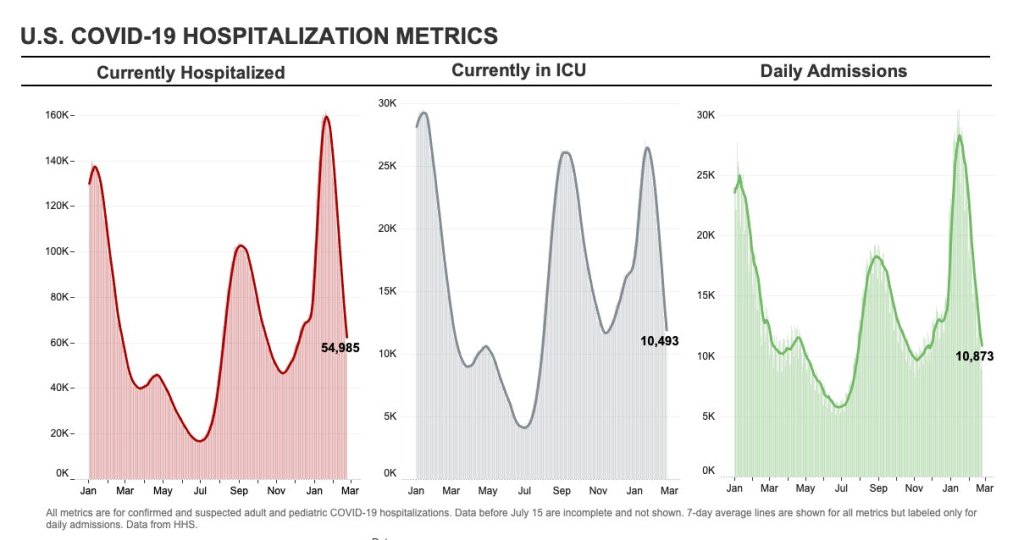
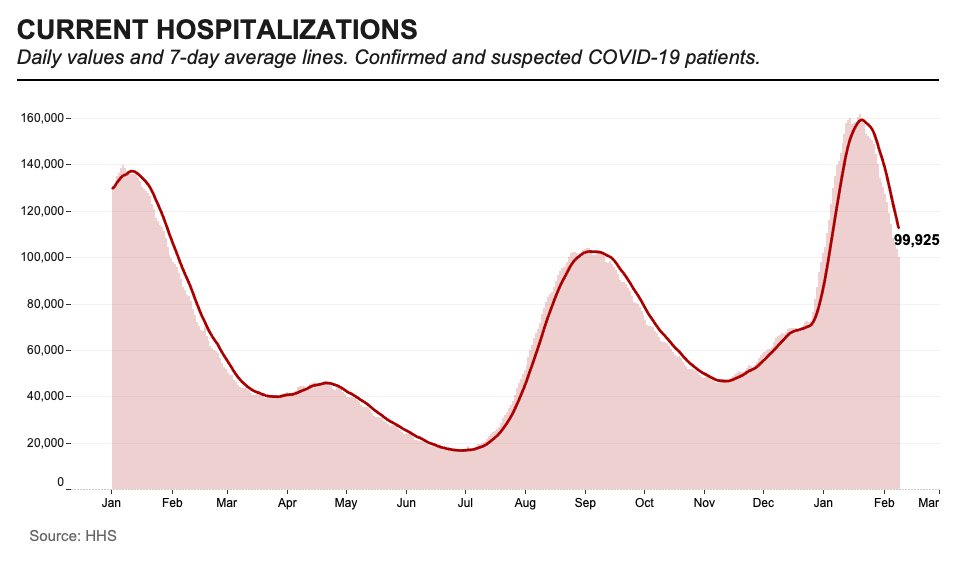
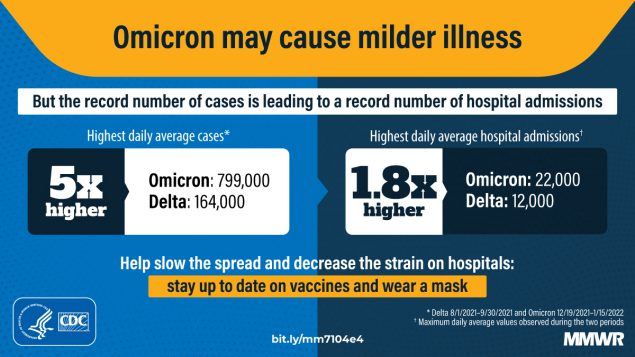
In the past week, the U.S. also reported about 22,000 new COVID-19 patients admitted to hospitals. This amounts to:
- An average of 3,100 new admissions each day
- 6.6 total admissions for every 100,000 Americans
- 28% fewer new admissions than last week
Additionally, the U.S. reported:
- 8,200 new COVID-19 deaths (2.5 for every 100,000 people)
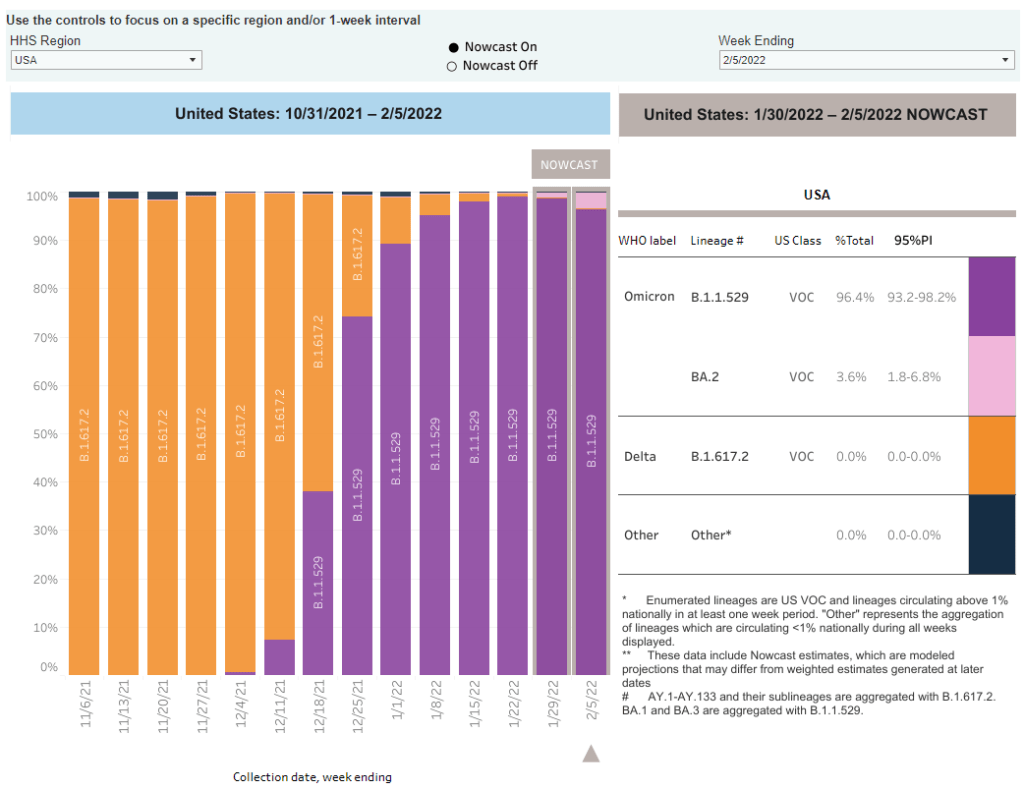
- 100% of new cases are Omicron-caused; 12% BA.2-caused (as of March 5)
- An average of 100,000 vaccinations per day (per Bloomberg)
Note: I’m shifting the format of these National Numbers posts to focus more on hospitalizations and wastewater, as case data become both less reliable and less available in many parts of the U.S.
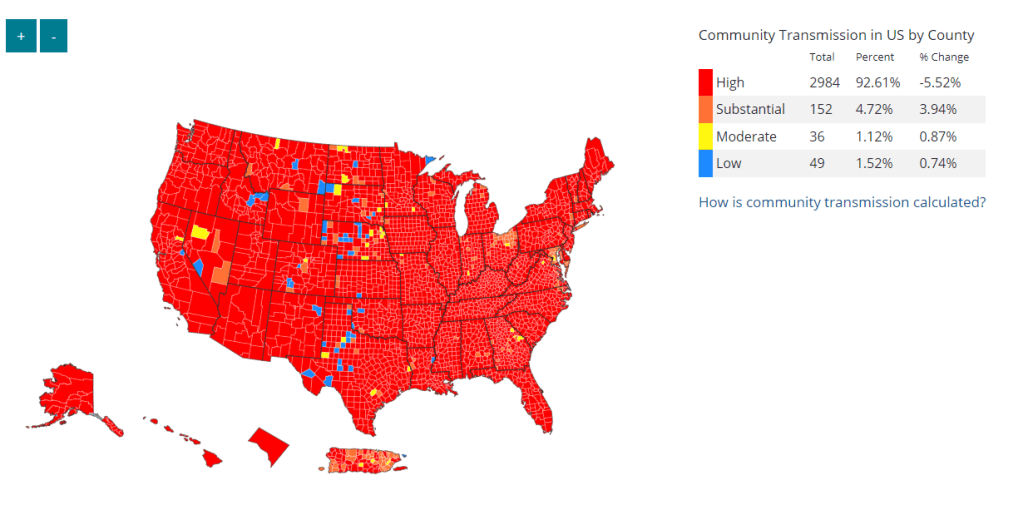
Overall, new COVID-19 cases are continuing to fall across the U.S. The country reported about 37,000 new cases a day last week, according to the CDC, compared to ten times that number in early February.
Case numbers have become less reliable lately as testing sites close and people are redirected to use at-home rapid tests, which are generally not reported. Still, we’re seeing a similar trend in new COVID-19 patients admitted to hospitals: both new cases and new admissions dropped almost 30% last week from the week prior.
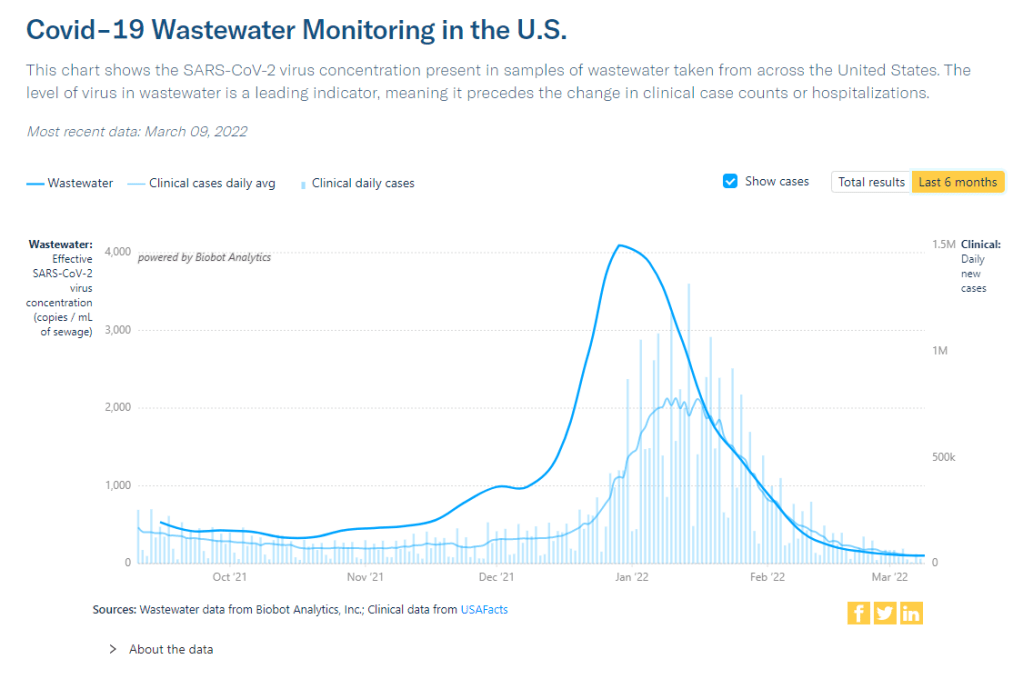
Additionally, wastewater levels are decreasing or plateauing across the country, according to the Biobot tracker, which compiles trends from over 90 locations. The CDC wastewater surveillance tracker is showing similar overall trends as well.
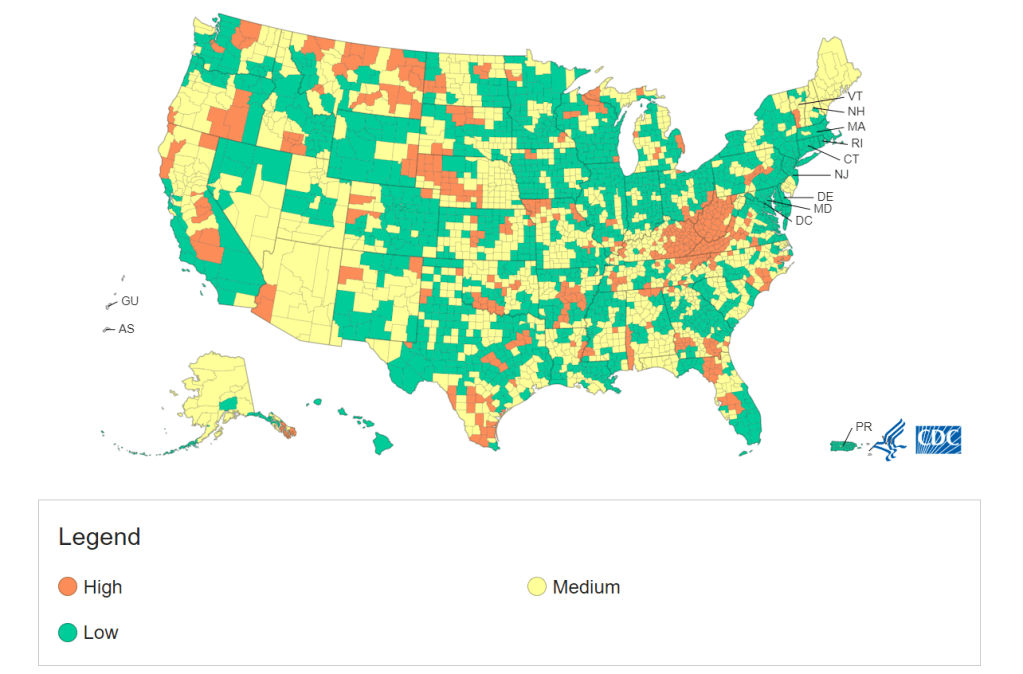
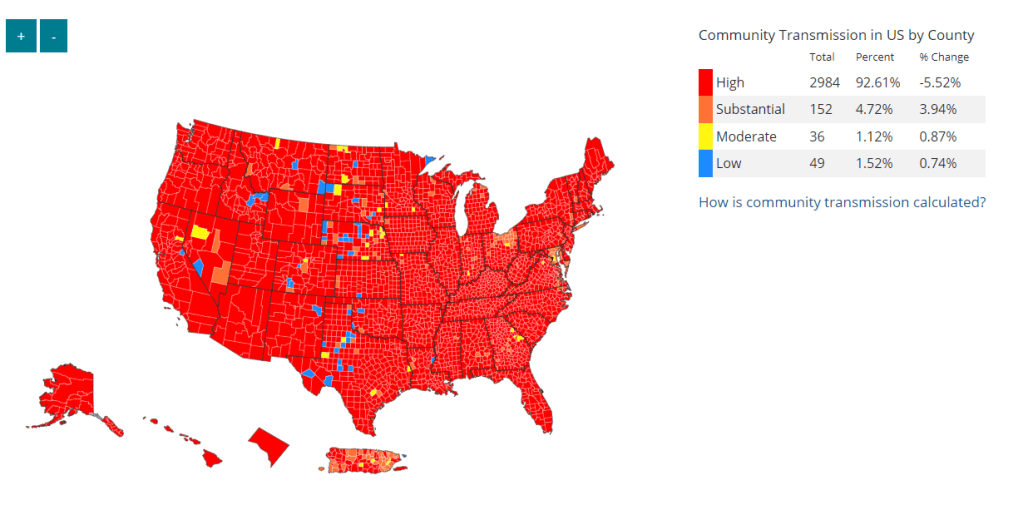
More than 98% of the U.S. population now lives in a location with a low or medium COVID-19 Community Level, according to the CDC. But a few places did see case increases last week: these include Nebraska, Kentucky, Alaska, and Delaware, according to the March 10 Community Profile Report.
BA.2, the Omicron sister variant that is even more transmissible than the original version of this strain, is slowly gaining ground in the U.S.: it’s gone from causing an estimated 1% of cases in the first week of February to 12% in the first week of March, according to the CDC’s modeling.
It hasn’t impacted case trends here yet, but deserves close attention in the coming weeks and months. Gothamist has a helpful article about BA.2’s potential impact in New York, where the variant’s prevalence in wastewater is doubling statewide every two weeks.
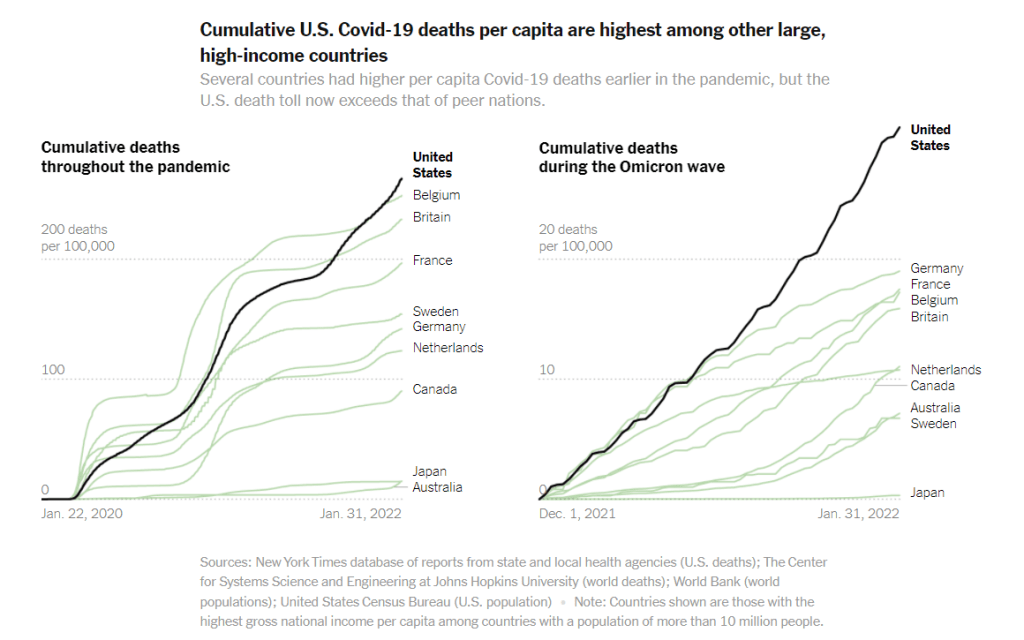
Meanwhile, several European countries—including the U.K., Germany, the Netherlands, and others—reported case increases this week. This is likely due to ending pandemic safety measures, Omicron gaining its second wind, or some combination of the two; regardless, it doesn’t bode well for the U.S., which is also ending pretty much all pandemic safety measures.