In the past week (October 1 through 7), the U.S. reported about 300,000 new COVID-19 cases, according to the CDC. This amounts to:
- An average of 42,000 new cases each day
- 89 total new cases for every 100,000 Americans
- 10% fewer new cases than last week (September 24-30)
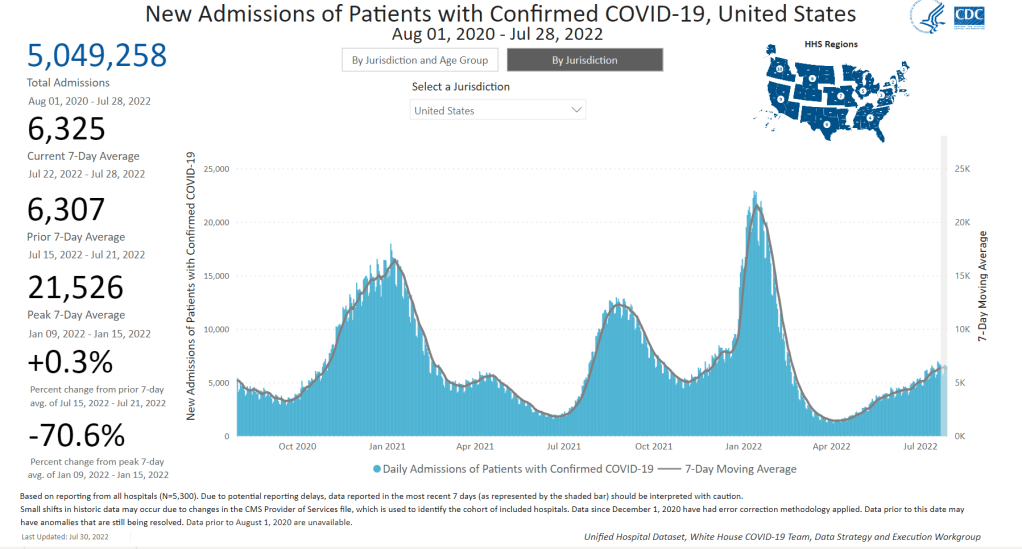
In the past week, the U.S. also reported about 23,000 new COVID-19 patients admitted to hospitals. This amounts to:
- An average of 3,300 new admissions each day
- 7.1 total admissions for every 100,000 Americans
- 5% fewer new admissions than last week
Additionally, the U.S. reported:
- 2,400 new COVID-19 deaths (350 per day)
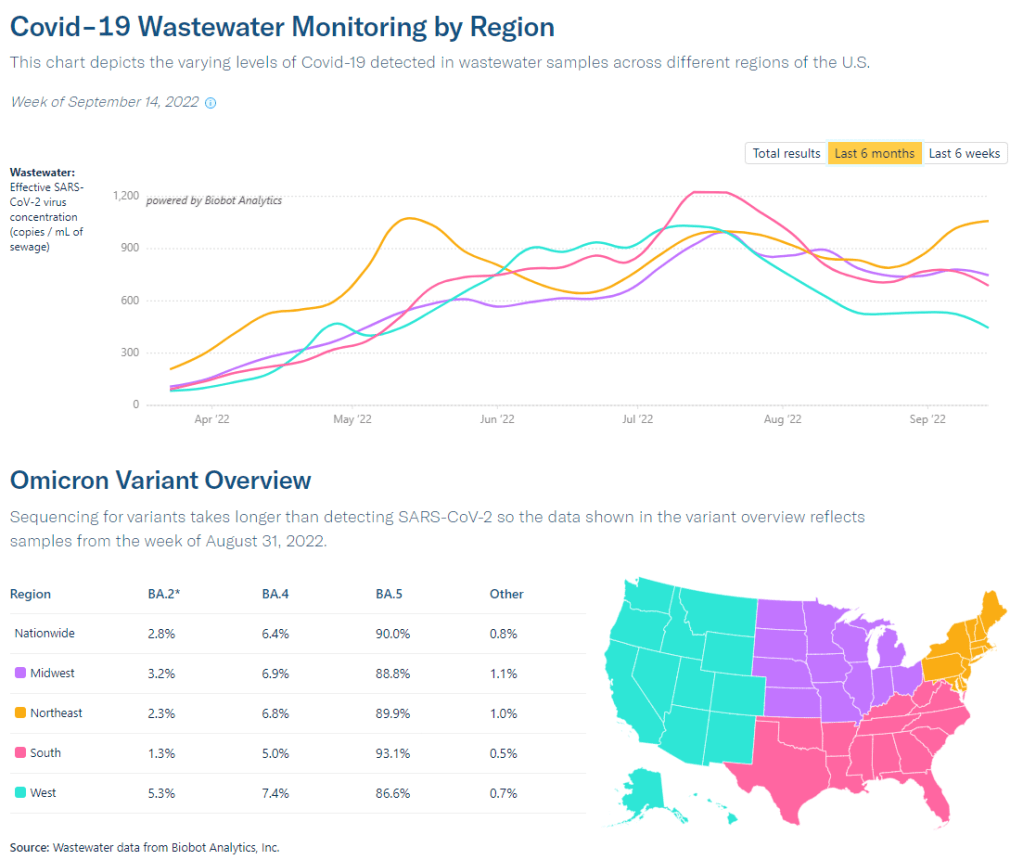
- 79% of new cases are caused by Omicron BA.5; 14% by BA.4.6; 5% by BF.7; 2% by BA.2.75 (as of October 8)
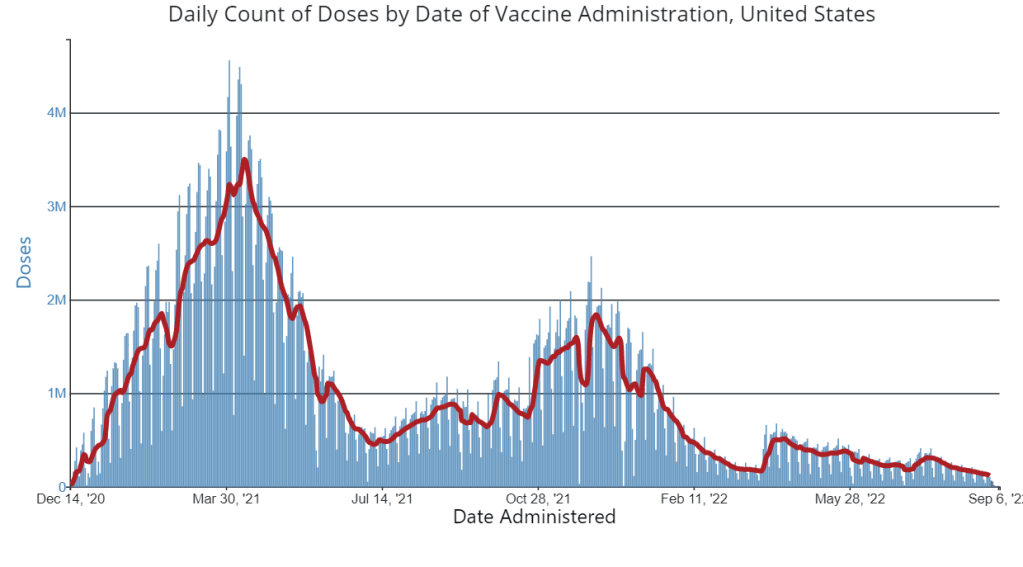
- An average of 400,000 vaccinations per day (CDC link)
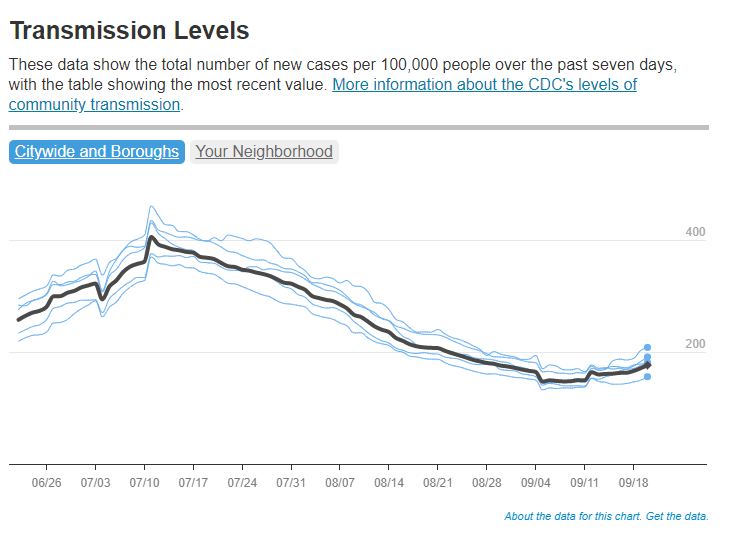
Following a pattern from the last couple of months, national COVID-19 cases and hospitalizations continued to trend slightly downward this week—though local indicators suggest we may experience a fall surge soon.
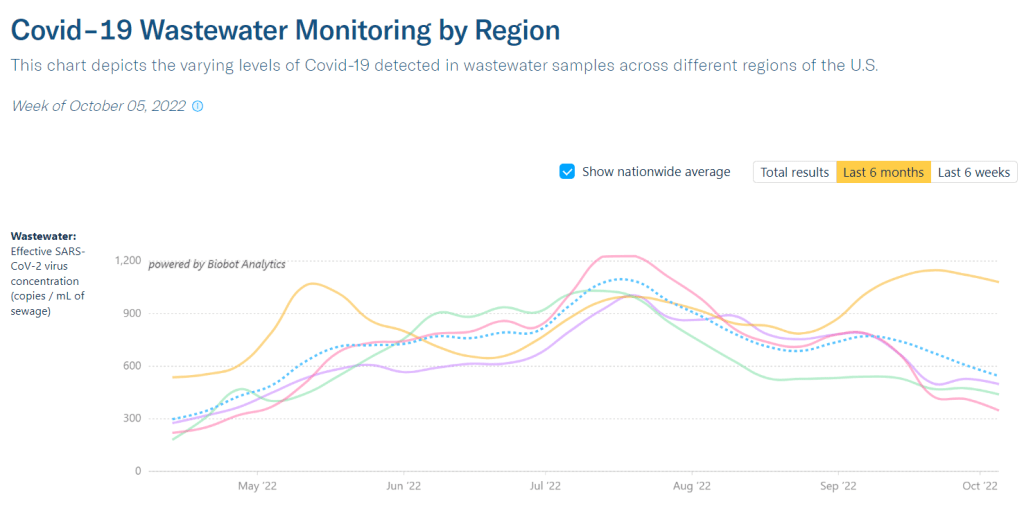
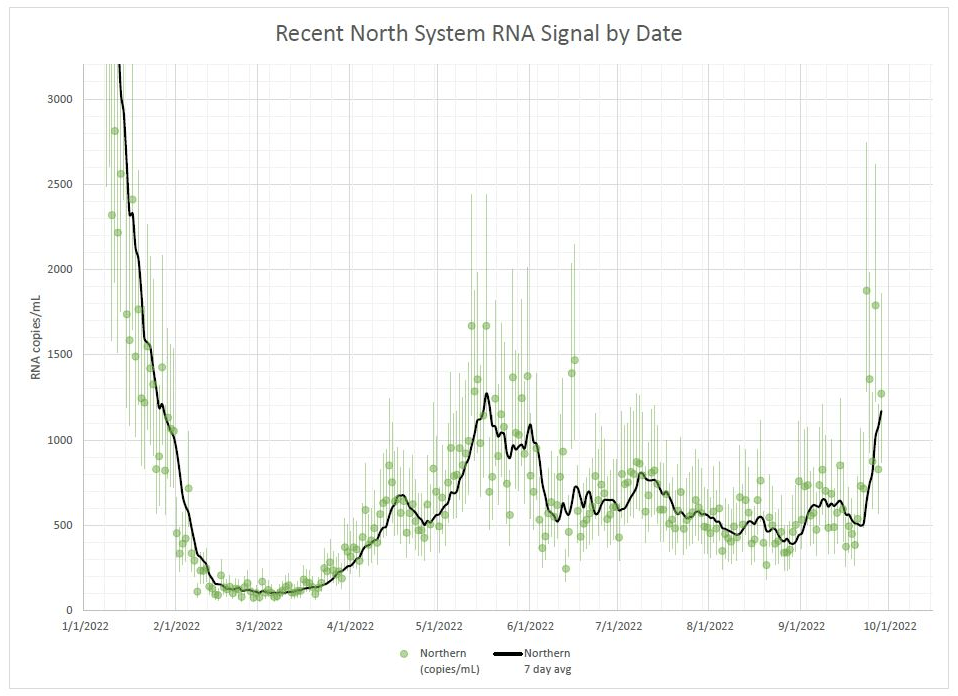
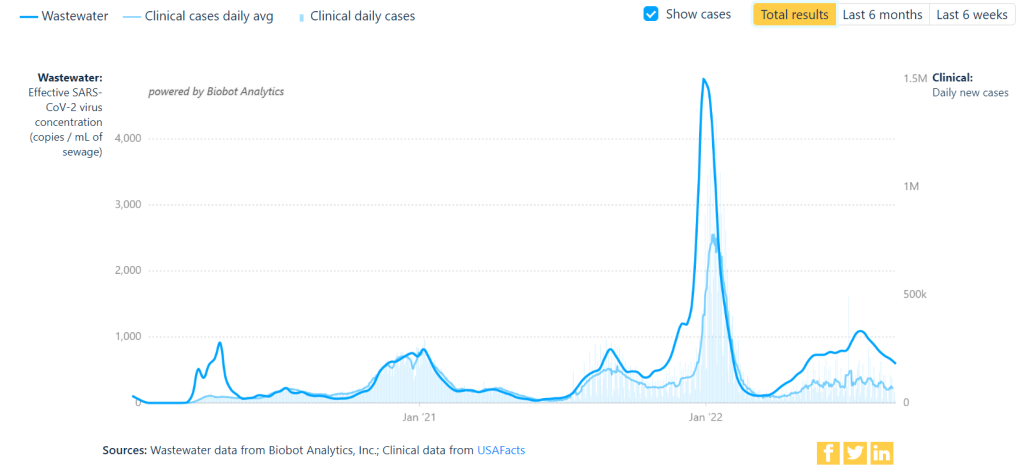
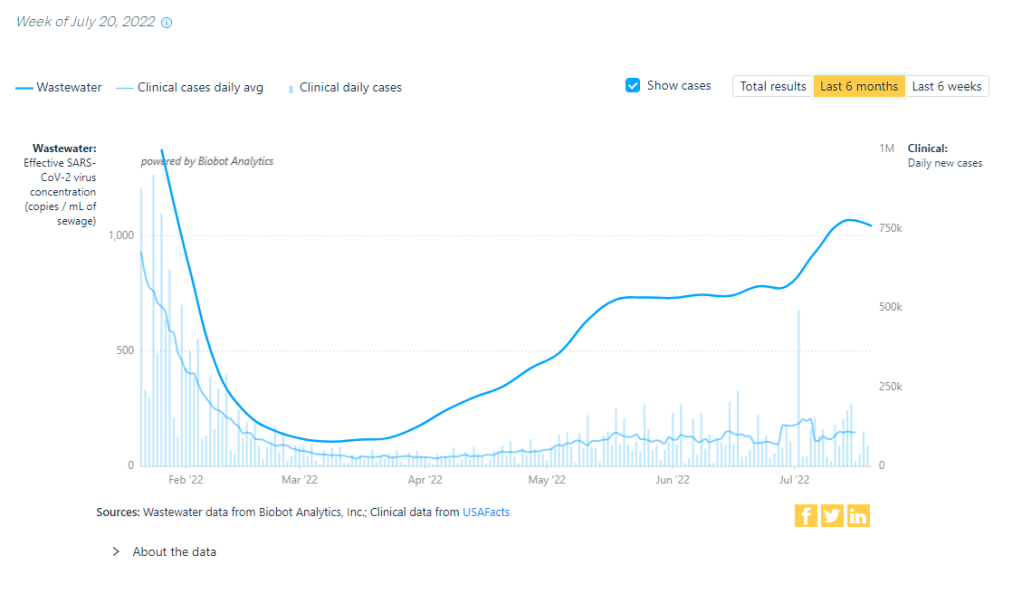
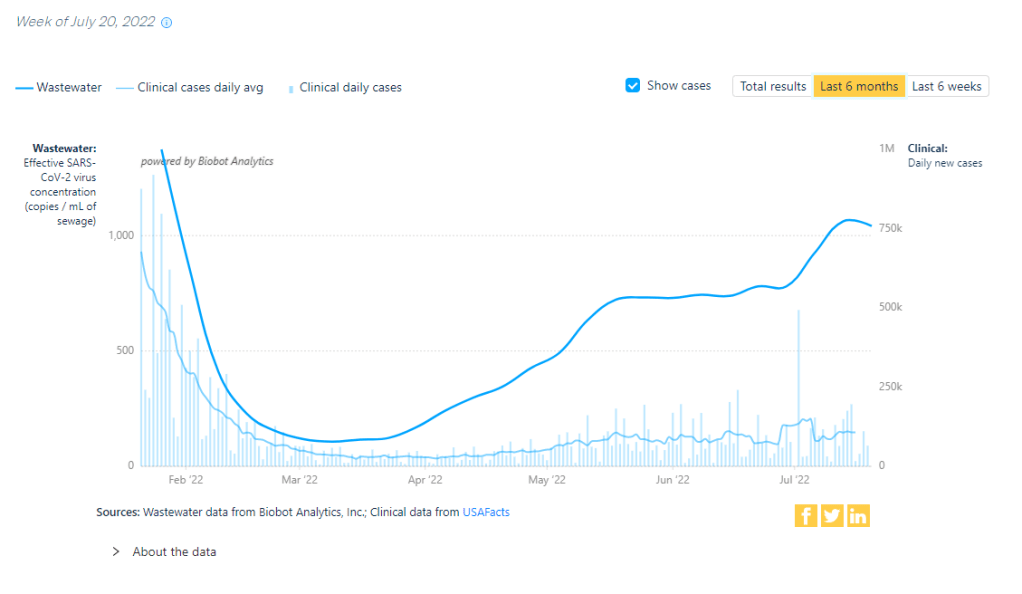
Biobot’s wastewater dashboard reports that coronavirus transmission has plateaued at a high level in the Northeast, and at lower levels in the Midwest, West, and South. More locally, several counties that Biobot monitors in Massachusetts, New Jersey, and nearby states are seeing increased viral levels in their wastewater; two prominent examples are Boston and Hartford, Connecticut.
Official COVID-19 cases are heavily underreported right now (by a factor of ten times or more); if we had a better testing infrastructure, they might match more closely to wastewater trends.
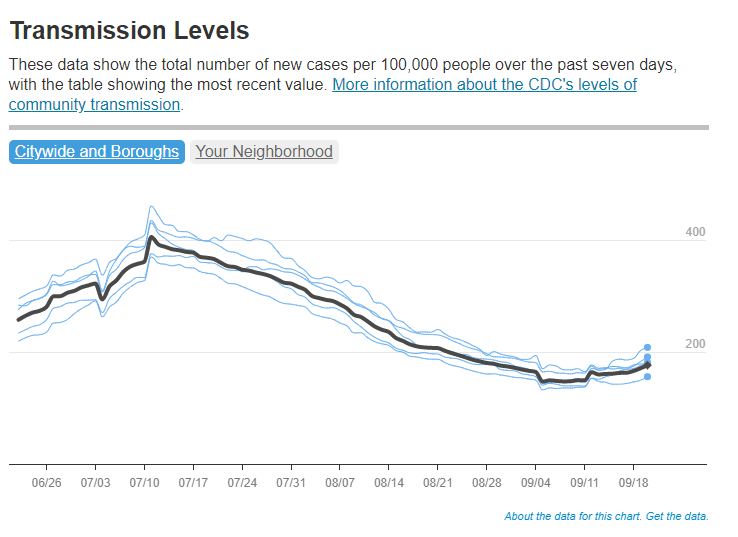
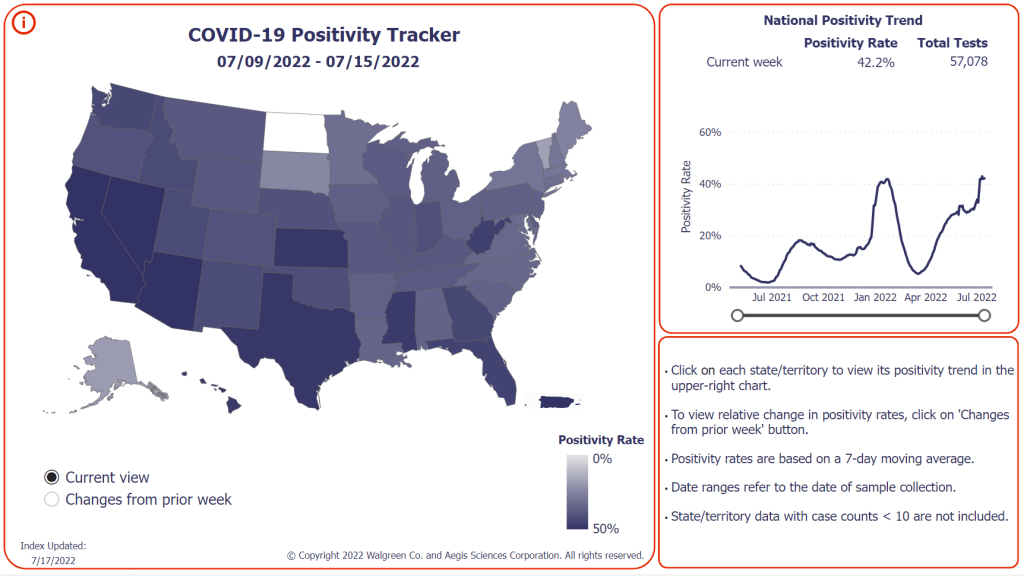
Even so, data from the HHS’s October 6 Community Profile Report show that several Northeast states reported among the highest case rates this week. Rhode Island, New Jersey, New York, and Massachusetts all reported 150 or more cases per 100,000 people in the week ending October 5. Kentucky and Puerto Rico reported even more cases, at rates over 200 per 100,000.
At the moment, we’re not seeing enough of the newer Omicron subvariants (BF.7, BA.2.75, etc.) to blame the transmission increases on them. Cold weather (driving people to gather indoors) and waning immunity from past cases and vaccinations are more likely culprits, as Katelyn Jetelina noted in a recent Your Local Epidemiologist post.
Jetelina also pointed out that fall waves are starting in Western European countries, including Germany and the U.K. The U.S. has followed trends in these countries throughout the pandemic, and it seems likely that the same thing will happen this fall—especially considering that the U.S. and European nations have similarly dismissive attitudes towards safety measures right now.
Again, the best way to protect yourself as we prepare for a potential surge is to get an Omicron-specific, bivalent booster shot. Uptake of these shots continues to be quite low in the U.S. so far: as of October 5, just 11.5 million Americans have received them, representing about 5% of the eligible population.