Longtime readers may remember that I am no fan of “The Morning,” a daily newsletter from the New York Times that has frequently downplayed COVID-19 in recent years. Last summer, for example, I called out the newsletter for misleading reporting about who was dying most from COVID-19.
Well, this week, the newsletter’s primary author, David Leonhardt, has done it again. Leonhardt wrote on Monday that “the pandemic really is over.” As evidence, he pointed to excess deaths (i.e. deaths above expected norms from past years), writing that this metric has returned to a pre-COVID-19 baseline.
It is true that excess deaths have been low since early 2023, when the country’s holiday COVID-19 surge concluded. And sure, this is good news about COVID-19’s current impact on mortality. You can see the CDC’s estimates here. However, Leonhardt’s newsletter fails to mention several caveats:
- If the pandemic were truly “over,” excess deaths would actually be below historical averages, not at them, to reflect people who had died prematurely of COVID-19 in the last three years. (Health law scholar Blake Murdoch pointed this out on Twitter.)
- Current death data are seriously undercounting COVID-19 deaths, thanks to the now-very-limited availability of COVID-19 tests combined with limited surveillance following the end of the federal public health emergency. The CDC revises up its estimates every week.
- Excess death data, in general, are typically considered preliminary estimates for about a year. So, the data Leonhardt sites are preliminary and likely to be revised up once the CDC compiles more information from death certificates.
- The pandemic has disproportionately impacted people of color and other vulnerable groups. Analysis from APM Research Lab shows that this pattern has continued through the first half of 2023.
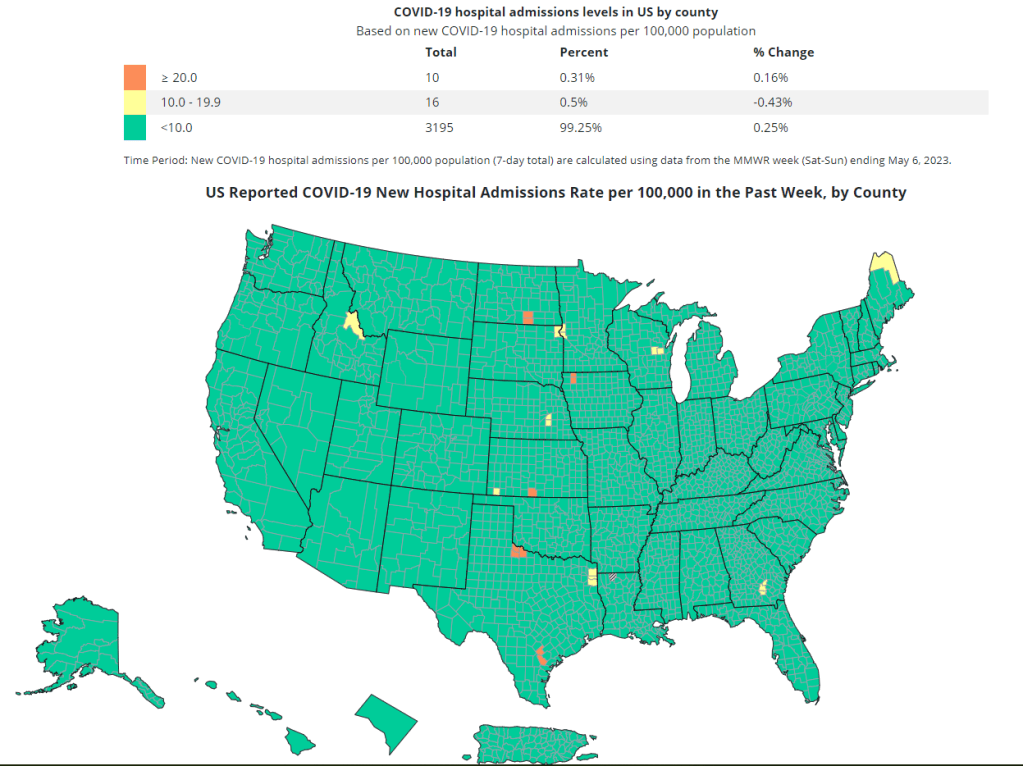
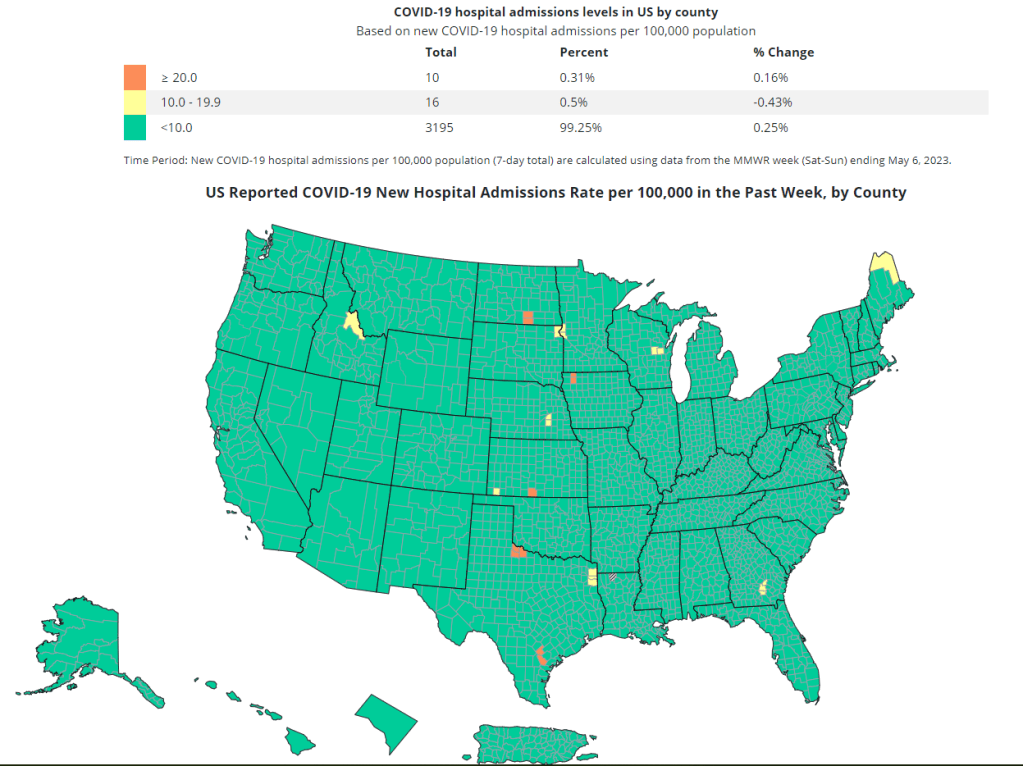
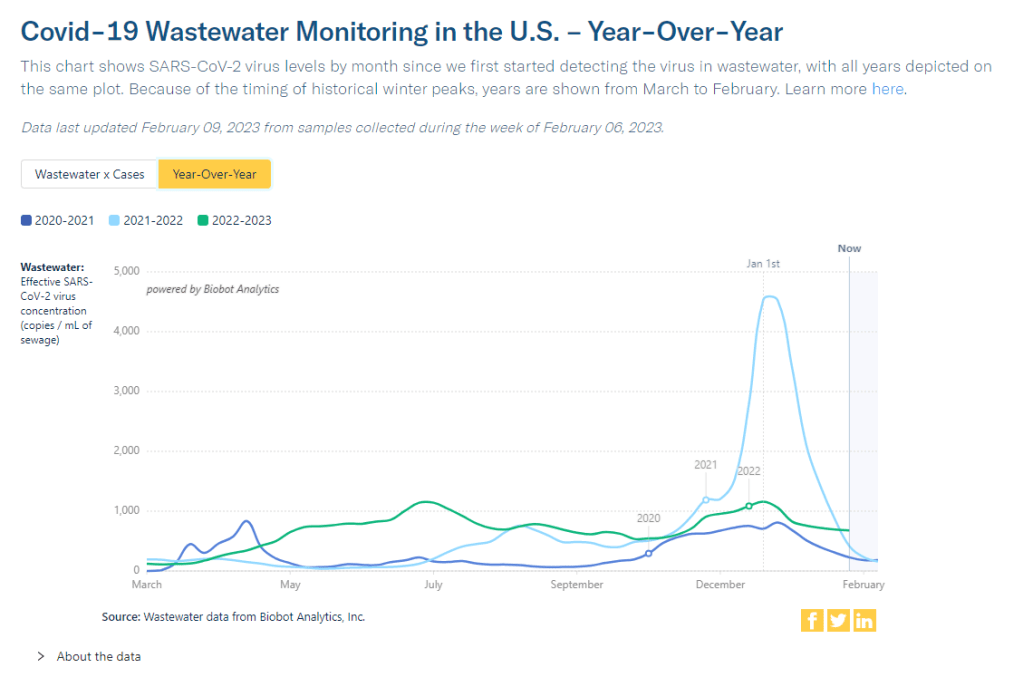
- Plenty of other metrics (including wastewater surveillance, hospitalizations, and the virus’ continued evolution) suggest that COVID-19 is still circulating and still making people sick. The U.S. is likely heading into a summer surge right now, in fact.
- Leonhardt fails to mention Long COVID, one of the most dire outcomes of COVID-19. Even though millions of people are still dealing with prolonged symptoms.
So, for whom is the pandemic really “over”? It might be over for Leonhardt himself, but it’s not over for people with Long COVID, people still mourning lost loved ones, high-risk people still taking every precaution, people who will get infected this summer, and so many more. All of these people challenge the NYT’s misleading narrative.