- CDC adds data on new booster shots: The latest addition to the CDC’s COVID Data Tracker is the Omicron-specific, bivalent booster shots, authorized a couple of weeks ago. So far, the CDC has only provided a total count of Omicron booster recipients (4.4 million, as of September 21) and incorporated these boosters into total counts of Americans who’ve received “first” and “second boosters. A note at the top of the dashboard explains the CDC is working to provide more granular data about the new boosters as separated out from past boosters.
- Evidence Commons (ASU): Researchers at Arizona State University’s College of Health Solutions have compiled this detailed dashboard of scientific publications related to COVID-19 tests, supported with funding from the Rockefeller Foundation. The dashboard incorporates information from over 3,000 papers, sorted by the type of test under study, methodology, analysis location, and more. It’s a helpful tool to sort through diagnostic details that are often buried in technical documents.
- Helix announces new CDC partnership: Speaking of testing, the viral sequencing and population genomics company Helix announced this week that it has an “extended agreement” with the CDC to sequence coronavirus samples for the agency’s analysis. While Helix has been working with the CDC on variant tracking for some time, the new partnership extends this important effort: Helix (and research partners) will sequence over 3,000 coronavirus samples per week for the next year, “with the option to double the number of samples during surge moments,” according to the company’s press release.
- Pathogen Genomics Centers of Excellence: The CDC has also directed new surveillance funding to five state health departments that will test out new genomics technologies and respond to infectious disease outbreaks. These five departments—Georgia, Massachusetts, Minnesota, Virginia, and Washington—are receiving $90 million over the next five years; the funding came out of $1.7 billion allocated for genomic surveillance in the American Rescue Plan. I’m glad to see this sustained funding going beyond COVID-19, though I wish more than five states were getting the money!
- Long-term nervous system damage from COVID-19: Ziyad Al-Aly and his team at the Veterans Affairs St. Louis Healthcare System have published a new paper on long-term impacts from a COVID-19 infection. The study used a large dataset of electronic health records from a national VA database, including 154,000 people with COVID-19 and over five million controls. COVID-19 patients had an elevated risk of strokes, cognition and memory problems, seizures, mental health disorders, encephalitis, and more. While the VA population isn’t the best representation for the U.S. population as a whole (it skews older and male), the study still provides evidence for long-term neurological complications from COVID-19.
- Long COVID estimates in Europe: And one more piece of Long COVID news for this week: the World Health Organization’s European division has produced new estimates on Long COVID for the continent. Between 10% and 20% of COVID-19 cases in Europe have led to mid- or long-term symptoms, the WHO found, impacting up to 17 million people. The study also found women are more likely to develop Long COVID.
Tag: genomic sequencing
-
Sources and updates, September 25
-
FAQ: BA.4 and BA.5, potentially the most transmissible Omicron subvariants yet

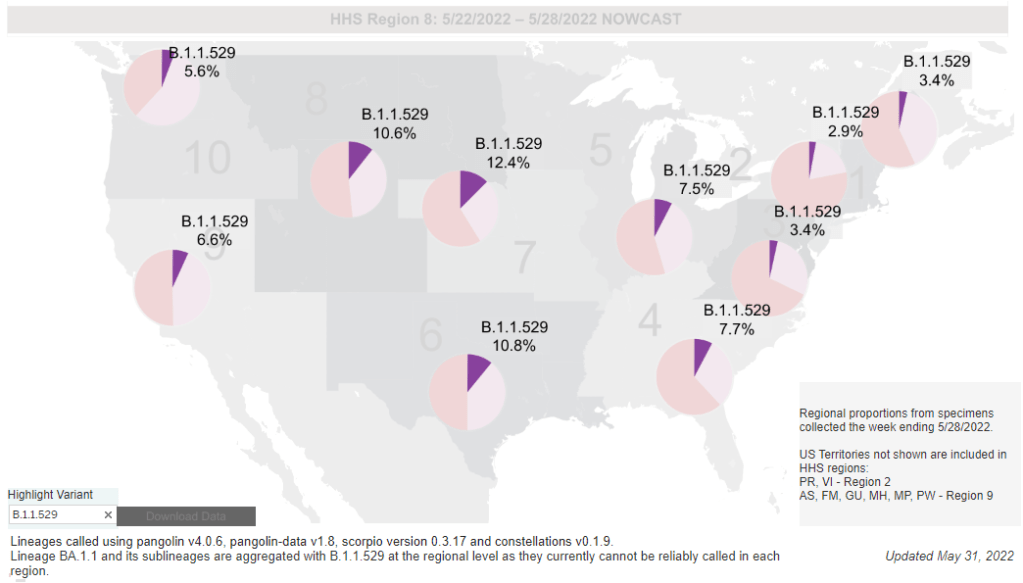
While the CDC is not yet reporting BA.4 and BA.5 separately, the subvariants are included in B.1.1.529; this grouping is driving increased transmission in some Midwestern and Southern states. Chart via the CDC variant dashboard. America’s current COVID-19 surge is being driven by BA.2 and its sublineage BA.2.12.1. But there are other versions of Omicron out there to which we need to pay attention—namely, BA.4 and BA.5. Here’s a brief FAQ on these two subvariants, including why scientists are concerned about them and where they’re spreading in the U.S.
What are BA.4 and BA.5?
Remember how, when South African scientists first sounded the alarm about Omicron in November, they identified three subvariants—BA.1, BA.2, and BA.3? BA.1 first spread rapidly around the world, followed by BA.2.
Then, in the winter, South African scientists again identified new Omicron subvariants, called BA.4 and BA.5. These two variations split from the original Omicron lineage, and tend to be discussed together because they have similar mutations. (Specifically, they have identical spike protein mutations; this article discusses the mutations in more detail).
It’s important to note that, while South African scientists characterized these subvariants, they likely didn’t originate in the country. South Africa has a better variant surveillance system than many other countries, particularly compared to its neighbors, allowing the country’s scientists to quickly identify variants of concern. BA.4 and BA.5 also caused a new surge in South Africa, allowing for study of the subvariants’ performance.
Why are scientists concerned about these subvariants?
Early studies of BA.4 and BA.5 indicate that not only are these subvariants more transmissible than other forms of Omicron, they’re also more capable of bypassing immunity from prior infection or vaccination.
Last week, I shared a new preprint from a Japanese research consortium that found BA.4 and BA.5 are more capable of resisting protection from a prior Omicron infection than BA.1. This study, while not yet peer-reviewed, followed similar research from a South African team that found antibodies from an Omicron BA.1 infection offered limited immunity against BA.4 and BA.5, compared to a new BA.1 or BA.2 infection.
Another study by researchers at Columbia University also follows this trend. These researchers tested antibodies from people who’d been vaccinated and boosted against BA.4 and BA.5; they found these two subvariants are “more than four times as likely to escape antibodies in people who’ve been vaccinated and boosted compared with BA.2 viruses,” CNN reports.
While the differences between BA.4/BA.5 and BA.1/BA.2 are less dramatic than the differences between the Omicron family and Delta, scientists hypothesize that there is still enough distinction between these two Omicron sub-groups that people who already had Omicron BA.1 or BA.2/BA.2.12.1 could potentially get reinfected by BA.4 or BA.5.
What are BA.4 and BA.5 doing in South Africa and other countries?
BA.4 and BA.5 have been detected in over 30 countries, according to CNN. But scientists have again focused on South Africa, as this country has better surveillance than many others—particularly as PCR testing declines around the world.
In South Africa, the BA.4/BA.5 wave that started in April has peaked and is now on the decline. Hospital admissions and deaths were lower in this recent wave than in the Omicron BA.1 wave in November and Decenter, largely thanks to high levels of immunity in the country. Still, the continued Omicron infections suggest that reinfection is a real concern for these subvariants.
South Africa never really had a BA.2 wave, so BA.4 and BA.5 mostly competed with other Omicron lineages in that country. But in the U.K., which did face BA.2, recent data suggest that BA.4 and BA.5 have a growth advantage over even BA.2.12.1. In other words, BA.4 and BA.5 could potentially outcompete BA.2.12.1 to become the most transmissible Omicron subvariants yet.
What are BA.4 and BA.5 doing in the U.S.?
The subvariants are definitely here and spreading, but we have limited visibility into where and how much thanks to declined testing and surveillance. The CDC has yet to separate out BA.4 and BA.5 on its variant dashboard; according to White House COVID-19 Data Director Cyrus Shahpar, this is because the CDC has yet to identify these subvariants as causing 1% or more of new national cases in a given week.
But the CDC does include BA.4 and BA.5 in its Omicron B.1.1.529 category, which has grown from causing 1% of new cases in the first week of May to causing 6% of new cases in the last week of the month. The number of cases sequenced in a week has dropped this spring compared to the first Omicron surge, leading me to wonder: are BA.4/BA.5 really causing fewer than 1% of new cases each, or do we just not have the data to detect them yet?
CDC data do show that the B.1.1.529 group (which includes BA.4/BA.5) is causing over 10% of new cases in the Plain States, Gulf Coast, and Mountain West—compared to under 5% in the Northeast, where BA.2.12.1 is more dominant. This data aligns with local reports of BA.4 and BA.5 spreading in wastewater in some Midwestern states that track variants in their sewage. For example, scientists at the Metropolitan Council in the Twin Cities recently said they expect BA.4 and BA.5 to “replace BA.2.12.1 as the dominant variants” in the next few weeks.
What could BA.4 and BA.5 mean for future COVID-19 trends in the U.S.?
As I noted above, data from the U.K. suggest that BA.4 and BA.5 could outcompete BA.2—and even BA.2.12.1—to become the dominant Omicron subvariants in the U.S. Early data from U.S. Omicron sequences are showing a similar pattern, reported variant expert Trevor Bedford in a recent Twitter thread.
“Focusing on the US, we see that BA.2.12.1 currently has a logistic growth rate of 0.05 per day, while BA.4 and BA.5 have logistic growth rates of 0.09 and 0.14 per day,” Bedford wrote. The country’s rising case counts can be mostly attributed to BA.2.12.1, he said, but BA.4 and BA.5 are clearly gaining ground. And, he noted, these two subvariants may be able to reinfect many people who already had BA.1 or BA.2.
In short: even more Omicron breakthrough infections and reinfections could be coming our way. Even if BA.2.12.1 transmission dips (as it seems to be doing in the Northeast), we could quickly see new outbreaks driven by BA.4 and BA.5—leading overall case numbers to plateau or rise again.
“For the summer, going into the winter, I expect these viruses to be out there at relatively high levels,” Dr. Alex Greninger from the University of Washington’s clinical virology lab told CNN. “Just the number of cases, the sheer disruptions of the workforce — It’s just a very high, high burden of disease.”
More variant reporting
-
A BA.2 surge is approaching: Here’s what you should know about this variant

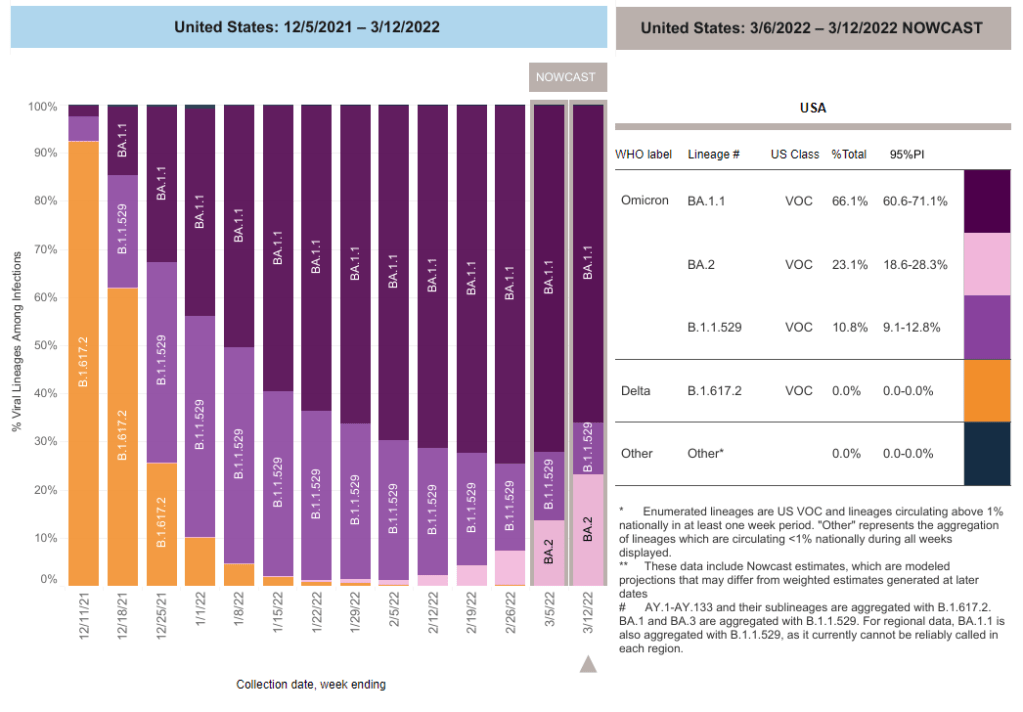
BA.2 caused about one in four U.S. COVID-19 cases in the week ending March 12, according to CDC estimates. Two years into the pandemic, we now know some basic truisms about the coronavirus. For example: outdoor events are always safer than indoor events; older age is the most significant risk factor for severe symptoms; hospitalization trends typically follow case trends by a couple of weeks; and whenever Europe has a new surge, the U.S. is likely to also see a surge in the next month or so.
That last truism is particularly relevant right now, because Europe is experiencing a new surge. Cases are increasing in the U.K., Germany, the Netherlands, and many other countries. The new surge is likely due to European leaders’ decisions to end all COVID-19 safety measures in their countries, combined with the rise of Omicron sublineage BA.2.
As BA.2 prevalence increases here in the U.S.—and our leaders also end safety measures—we seem poised to follow in Europe’s footsteps once again. But a BA.2 surge is likely to look different from the intense Omicron surge that we experienced in December and January, in part because of leftover immunity from that Omicron surge.
Let’s go over what we know about BA.2, and what might happen in the next few weeks.
What is BA.2?
It’s important to note that this isn’t a new variant, at least not compared to the original Omicron strain. As I noted in a FAQ post about this strain back in January, South African scientists who originally characterized Omicron in November 2021 identified three sub-lineages: BA.1, BA.2, and BA.3.
BA.1 spread rapidly through the world, driving the surge that we experienced here in the U.S. in December through February. But BA.2, it turns out, is actually more transmissible than BA.1—allowing it to now outcompete that strain and contribute to case increases in countries that already faced major BA.1 surges.
How does BA.2 differ from BA.1, or original Omicron?
The main difference between these two strains is that BA.2 is more contagious: scientists estimate that BA.2 is about 30% more transmissible than other Omicron strains, if not more. (Note that this is a smaller difference than Omicron’s advantage over Delta and other earlier variants.)
In a recent report, the U.K. Health Security Agency estimated that someone infected with BA.2 would infect about 13.6% of their households and 5.3% of contacts outside of their households, compared to 10.7% of households and 4.2% outside contacts for other Omicron strains. The modest difference between these rates demonstrates why BA.2 is not outcompeting other Omicron strains as quickly as Omicron outcompeted Delta a couple of months ago.
Another notable feature of BA.2 is that, unlike BA.1, it can’t be identified with a PCR test. BA.1 has a mutation called S drop-out, which causes a special signal in PCR test results, allowing the variant to be flagged without sequencing; BA.2 doesn’t have this mutation. To be clear, a PCR test will still return a positive result for someone who is infected with BA.2—it’ll just take an additional sequencing step to identify that they have this particular strain.
Finally, one major challenge during the Omicron BA.1 surge has been that two of the three monoclonal antibody treatments used in the U.S. did not work well for people infected with Omicron. BA.2 may exacerbate this challenge, as some studies have suggested that the third treatment—called sotrovimab—continued working against BA.1, but may not hold up against BA.2. Luckily though, Eli Lilly (which developed one of the treatments that failed for BA.1) has produced an updated monoclonal antibody cocktail that does work for both Omicron strains.
How is BA.2 similar to BA.1, or original Omicron?
Two major pieces of good news here: 1) our existing COVID-19 vaccines work similarly well against BA.2 as they do against BA.1, and 2) prior infection with BA.1 seems to be protective against infection with BA.2.
Essentially, studies are showing that the two strains are close enough in their genetic profiles that antibodies from a BA.1 infection will provide some immunity against a BA.2 infection. And the same thing goes for vaccination, at least when it comes to protection against severe disease. A recent CDC study showed that, even during the Omicron surge, COVID-19 patients who had received three vaccine doses were far less likely to require mechanical ventilation or die from the disease than those who weren’t vaccinated.
There’s a flip side to this, though: for both BA.1 and BA.2, prior infection with a previous variant is not very protective against an Omicron infection. CDC seroprevalence data suggest that between 40% and 45% of Americans got infected with BA.1 during the winter surge; this means the remaining 55% to 60% of the population is susceptible to BA.2. Vaccines protect against severe disease and death from BA.2, but they don’t protect against BA.2 infection to the degree that they did against past variants.
BA.2 and BA.1 are also similar in their severity. Both strains are less likely to cause severe disease than Delta; BA.1 had a 59% lower risk of hospital admission and 69% lower risk of death than Delta in the U.K., according to a new paper published this week in the Lancet.
It’s important to remember, however, that Delta was actually more severe than other variants that preceded it. As a result, “Omicron is about as mild/severe as early 2020 SARSCoV2,” wrote computational biologist Francois Balloux in his Twitter thread (referring to both BA.1 and BA.2).
What are the warning signs for a BA.2 surge in the U.S.?
First of all, many U.S. experts consider case increases in Europe to be an early indicator of increases in the U.S. As I said at the top of the post, Europe is seeing a surge right now, and many of the countries reporting case increases have estimated over 50% of their cases are caused by BA.2.
In the U.S., our BA.2 levels are lower: the CDC’s most recent estimates suggested that BA.2 was causing about 23% of new cases nationwide as of March 12. If BA.2 continues growing at the same rate we’ve seen in recent weeks, we have one or two more weeks before this variant hits 50% prevalence in the U.S.
“The tipping point seems to be right around 50%,” Keri Althoff, an epidemiologist at Johns Hopkins Bloomberg School of Public Health, told CNN. “That’s when we really start to see that variant flex its power in the population” as far as showing its severity.
At the same time, several Asian countries are also seeing major BA.2 surges at the moment. For example, Hong Kong was able to deal with early Omicron cases earlier in the winter, former COVID Tracking Project lead Erin Kissane pointed out in her Calm Covid newsletter; but now, the territory is facing a terrible BA.2 wave, driving what is now the world’s highest case fatality rate.
Here in the U.S., we’re also seeing warning signals in the form of rising coronavirus levels in wastewater. (Wastewater is considered an early indicator for surges, because coronavirus material often shows up in sewer systems before people begin to experience symptoms or get tested.) About one-third of sewershed collection sites in the CDC’s wastewater monitoring network are reporting increased virus prevalence in the two-week period ending March 15.
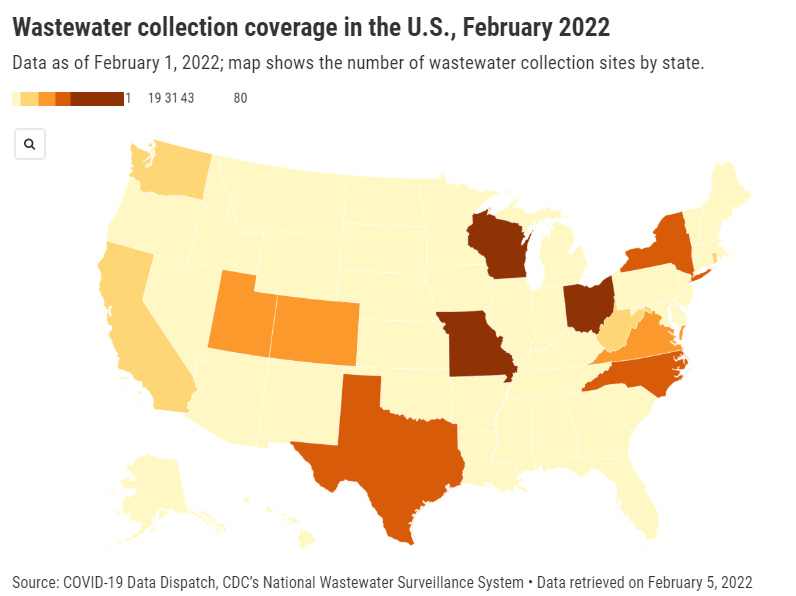
The CDC wastewater data must be interpreted cautiously, however, as this surveillance network is biased towards states like Missouri and Ohio, which have over 50 collection sites included in the national network. 12 states still do not have any collection sites in the network at all, while 23 states have fewer than 10. This recent Bloomberg article includes more context on interpreting wastewater data.
New York City is one place that’s reporting increased viral levels in wastewater, at the same time as the city health department reports that case numbers have plateaued—or may even be ticking up. An excellent time to loosen all mask and vaccination requirements, am I right?
What might a BA.2 surge in the U.S. look like?
Between the warning signals from Europe and the newly-lax safety measures throughout the U.S., it seems very likely that we will see a BA.2 surge in the coming weeks. The bigger question, though, is this surge’s severity: to what extent will it cause severe disease and death?
As I mentioned above, estimates suggest that about 40% to 45% of Americans have some Omicron antibodies from an infection earlier in the winter. At the same time, about 65% of the population is fully vaccinated and 45% of those fully vaccinated have received a booster shot, according to the CDC.
That’s a lot of people who are protected against severe COVID-19 symptoms, if they get infected with BA.2. But the U.S. has lower vaccination coverage than other countries, particularly when it comes to boosters. For example, in the U.K., 86% of eligible people are fully vaccinated and 67% are boosted, according to CNN. These lower vaccination rates contributed to the U.S.’s high mortality rate during the Omicron surge compared to other wealthy countries.
While the vaccines offer great protection, the U.S. appears to have given up on many other COVID-19 safety measures, like masks, social distancing, and limits on in-person gatherings. Without reinstating some of these measures, we would essentially be left without any tools to slow down the spread of BA.2; and even if some states and cities put safety measures in place, they’ll likely face more pushback now than they did in earlier surges.
To quote from Kissane’s newsletter:
In practical terms, with work and school happening in-person and without high-filtration (or any) masks or serious ventilation requirements in the US and most of Europe, governments in North America and Europe have made increased covid exposure essentially mandatory for most citizens.
I want to emphasize that for most vaccinated people, this increased risk probably won’t be a huge deal even if BA.2 causes a new case surge—they’ve either already racked up enough immunity to fight off BA.2 or they’ll be sick for a week.
One big caveat to this, though: we don’t have great data yet on how Omicron (or BA.2 specifically) might contribute to Long COVID rates; collecting data on this condition is very challenging and takes a lot of time. Studies suggest that vaccination reduces an individual’s risk of long-term symptoms if they get infected, but it does not eliminate this risk.
What can you do to prepare for this potential surge?
Here are a few things that I’m doing to prepare for a potential BA.2 surge in the coming weeks:
- Promoting vaccination—particularly booster shots—to family members and friends.
- Stocking up on good-quality masks (i.e. N95s and KN95s) and rapid tests. (Reminder, order a new round of free tests from covidtests.gov if you haven’t yet!)
- Researching my options for COVID-19 treatments (antiviral pills and monoclonal antibodies) in the event that I get infected.
- Getting tested frequently, particularly before attending indoor events (such as gathering with a few other friends, or going out to a movie theater.)
- Watching wastewater and case trends in my area, and preparing to cut down on riskier behaviors if(/when) cases start rising.
As always, if you have any COVID-19 questions (about BA.2 or otherwise) that you’d like me to address, please reach out.
More variant reporting
-
Pandemic preparedness: Improving our data surveillance and communication
Screenshot of the new Biden COVID-19 plan. As COVID-19 safety measures are lifted and agencies move to an endemic view of the virus, I’m thinking about my shifting role as a COVID-19 reporter. To me, this beat is becoming less about reporting on specific hotspots or control measures and more about preparedness: what the U.S. learned from the last two years, and what lessons we can take forward—not just for the future COVID-19 surges that are almost certainly coming, but also for future infectious disease outbreaks.
To that end, I was glad to see the Biden administration release a new COVID-19 plan focused on exactly this topic: preparedness for new surges, new variants, and new infectious diseases beyond this current pandemic.
From the plan’s executive summary:
Make no mistake, President Biden will not accept just “living with COVID” any more than we accept “living with” cancer, Alzheimer’s, or AIDS. We will continue our work to stop the spread of the virus, blunt its impact on those who get infected, and deploy new treatments to dramatically reduce the occurrence of severe COVID-19 disease and deaths.
The Biden plan was released last week, in time with the president’s State of the Union address. I read through it this morning, looking for goals and actions connected to data collection and reporting.
Here are a few items that stuck out to me, either things that the Biden administration is already doing or should be doing:
- Improving surveillance to identify new variants: The U.S. significantly improved its variant sequencing capacity in 2021, multiplying the number of cases sequenced by more than tenfold from the beginning to the end of the year. But the new Biden plan promises to take these improvements further, by adding more capacity for sequencing at state and local levels—and, crucially, “strengthening data infrastructure and interoperability so that more jurisdictions can link case surveillance and hospital data to vaccine data.” In plain language, that means: making it easier to track breakthrough cases (which I have argued is a key data problem in the U.S.).
- Expanding wastewater surveillance: As I’ve written before, in the current national wastewater surveillance network, some states are very well-represented with over 50 collection sites; while other states are not included in the data at all. The Biden administration is committed to bring more local health agencies and research institutions into the surveillance network, thus expanding our national capacity to get early warnings about surges.
- Standardizing state and local data systems: I’ve written numerous times that the U.S. suffers from a lack of standardization among its 50 different states and hundreds of local health agencies. According to the new plan, the Biden administration plans to facilitate data sharing, aggregating, and analyzing data across state and local agencies—including wastewater monitoring and other potential methods of surveillance that would provide early warnings of new surges. This would be huge if it actually happens.
- Modernize the public health data infrastructure: One thing that could help health agencies better coordinate and share data: modernizing their data systems. That means phasing out fax machines and mail-in reports (which, yes, some health departments still use) and investing in new electronic health record technologies, while hiring public health workers who can manage such systems.
- Use a new variant playbook to evaluate new virus strains: Also in the realm of variant preparedness, the Biden administration has developed a new “COVID-19 Variant Playbook” that may be used to quickly determine how a new variant impacts disease severity, transmissibility, vaccine effectiveness, and other factors. The new playbook may be used to quickly update vaccines, tests, and treatments if needed, by working in partnership with health systems and research institutions.
- Collecting demographic data on vaccinations and treatments: The Biden plan boasts that, “Hispanic, Black, and Asian adults are now vaccinated at the same rates as White adults.” However, CDC data shows that this trend does not hold true for booster shots: eligible white Americans are more likely to be boosted than those in other racial and ethnic groups. The administration will need to continue collecting demographic data to identify and address gaps among vaccinations and treatments; indeed, the Biden plan discusses continued efforts to improve health equity data.
- Tracking health outcomes for people in high-risk settings: Along with its health equity focus, the Biden plan discusses a need to better track and report on health outcomes in nursing homes, other long-term care facilities, and other congregate settings like correctional facilities and homeless shelters. Congregate facilities continue to be major COVID-19 hotspots whenever there’s a new outbreak, so improving health standards in these settings should be a major priority.
- Studying and combatting vaccine misinformation, vaccine safety: The new plan acknowledges the impact of misinformation on vaccine uptake in the U.S., and commits the Biden administration to addressing this trend. This includes a Request for Information that will be issued by the Surgeon General’s office, asking researchers to share their work on misinformation. Meanwhile, the administration will also continue monitoring vaccine safety and reporting these data to the public.
- Test to Treat: One widely publicized aspect of the Biden plan is an initiative called “Test to Treat,” which would allow people to get tested for COVID-19 at pharmacies, health clinics, long-term care facilities, and other locations—then, if they test positive, immediately receive treatment in the form of antiviral pills. If this initiative is widely funded and adopted, the Biden administration should require all participating health providers to share testing and treatment data. This would allow researchers to evaluate whether this testing and treatment rollout has been equitable across different parts of the country and minority groups.
- Website for community risk levels and public health guidance: The Biden plan includes the launch of a government website “that allows Americans to easily find public health guidance based on the COVID-19 risk in their local area and access tools to protect themselves.” The CDC COVID-19 dashboard was recently redesigned to highlight the agency’s new Community Level guidance, which is likely connected to this goal. Still, the CDC dashboard leaves much to be desired when it comes to comprehensive information and accessibility, compared to other trackers.
- A new logistics and operational hub at HHS: In the last two years, the Department of Health and Human Services (HHS) built up an office for coordinating the development, production, and delivery of COVID-19 vaccines and treatments. The new Biden plan announced that this office will become a permanent part of the agency, and may be used for future disease outbreaks. At the same time, the Biden administration has added at-home tests, antiviral pills, and masks to America’s national stockpile for future surges; and it is supporting investments in laboratory capacity for PCR testing.
- Tracking Long COVID: Biden’s plan also highlights Long COVID, promoting the need for government efforts to “detect, prevent, and treat” this prolonged condition. The plan mentions NIH’s RECOVER initiative to study Long COVID, discusses funding new care centers for patients, and proposes a new National Research Action Plan on Long COVID that will bring together the HHS, VA, Department of Defense, and other agencies. Still, the plan doesn’t discuss actual, financial support for patients who have been out of work for up to two years.
- Supporting health and well-being among healthcare workers: The new Biden plan acknowledges major burnout among healthcare workers, and proposes a new grant program to fund mental health resources, support groups, and other systems of combatting this issue. Surveying healthcare workers and developing systematic solutions to the challenges they face could be a major aspect of preparing for future disease outbreaks. The Biden plan also mentions investing in recruitment and pipeline programs to support diversity, equity, and inclusion among health workers.
- More international collaboration: The new Biden plan also focuses on international aid—delivering vaccine donations to low-income nations—and collaboration—improving communication with the WHO and other global organizations that conduct disease surveillance. This improved communication may be especially key for identifying and studying new variants in a global pandemic surveillance system.
This week, a group of experts—including some who have advised the Biden administration— followed up on the Biden plan with their own plan, called “A Roadmap for Living with COVID.” The Roadmap plan also emphasizes data collection and reporting, with a whole section on health data infrastructure; here, the authors emphasize establishing centralized public health data platforms, linking disparate data types, designing data infrastructure with a focus on health equity, and improving public access to data.
Both the Biden administration’s plan and the Roadmap plan give me hope that U.S. experts and leaders are thinking seriously about preparedness. However, simply releasing a plan is only the first step to making meaningful changes in the U.S. healthcare system. Many aspects of the Biden plan involve funding from Congress… and Congress is pretty unwilling to invest in COVID-19 preparedness right now. Just this week, a $15 billion funding plan collapsed in the legislature after the Biden administration already made major concessions.
Readers, I recommend calling your Congressional representatives and urging them to support COVID-19 preparedness funding. You can also look into similar measures in your state, city, or other locality. We need to improve our data in order to be prepared for future disease outbreaks, COVID-19 and beyond.
More national data
-
Omicron updates: BA.2, vaccine effectiveness, and more

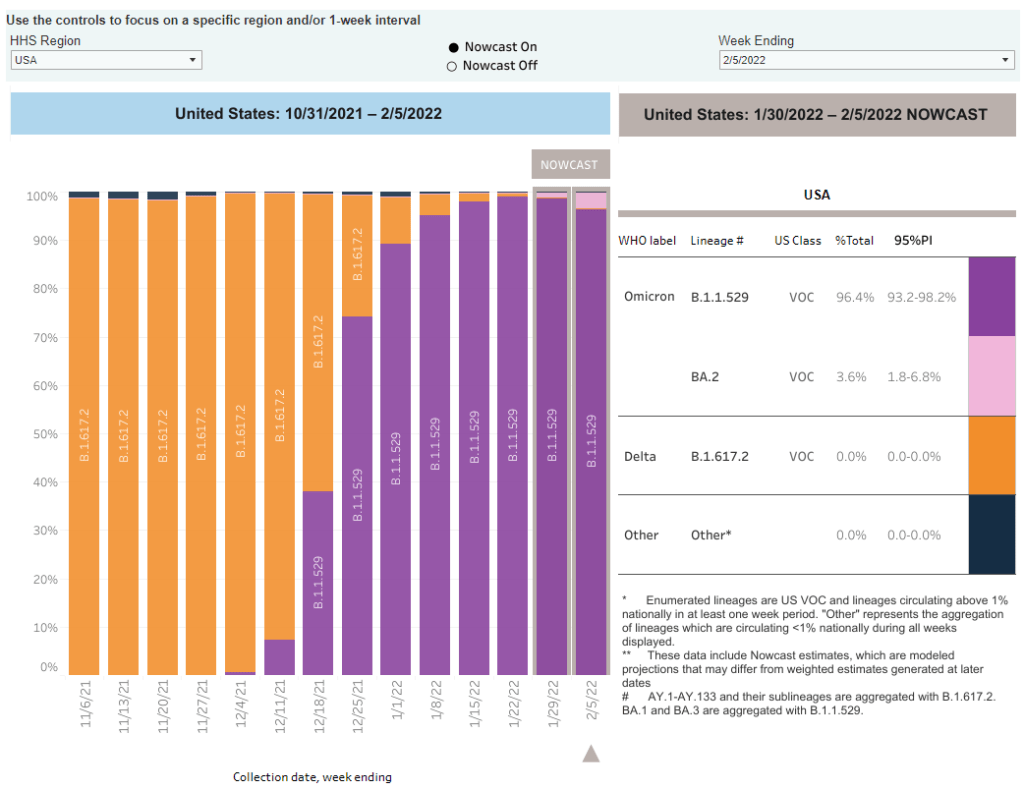
As of February 5, the CDC is now including BA.2 in its variant prevalence estimates. Screenshot from the CDC dashboard. A few Omicron-related news items for this week:
- The CDC added BA.2 to its variant prevalence estimates. As I mentioned in today’s National Numbers post, the CDC is now splitting out its estimates of Omicron prevalence in the U.S. into original Omicron, also called B.1.1.529 or BA.1, and BA.2—a sister strain that’s capable of spreading faster than original Omicron. BA.2 has become the dominant variant in some parts of Europe and Asia, but seems to be present in the U.S. in fairly low numbers so far: the CDC estimates it caused about 3.6% of new cases nationwide in the week ending February 5, with a 95% confidence interval of 1.8% to 6.8%. The remainder of new cases last week were caused by original Omicron.
- CDC describes its expanded genomic surveillance efforts in an MMWR study released this week. Between June 2021 and January 2022, the agency has extended its ability to monitor new variants spreading in the U.S., incorporating public repositories like GISAID into CDC data collection and developing modeling techniques that can produce more timely estimates of variant prevalence. (Remember: all variant data are weeks old, so the CDC uses modeling to predict the present.) According to the MMWR study, genomic sequencing capacity in the U.S. tripled from early 2021 to the second half of the year.
- Vaccine effectiveness from a booster shot wanes several months after vaccination. In another MMWR study released this week, the CDC reports on mRNA vaccine effectiveness after two and three doses, based on data from a hospital network including hundreds of thousands of patients in 10 states. During the U.S.’s Omicron surge, researchers found, vaccine effectiveness against COVID-19 hospitalization was 91% two months after a third dose—but declined to 78% four months afterward. It’s unclear whether this declining effectiveness is a direct result of Omicron getting past the vaccine’s defenses, or whether we’d see similar declines with other variants. Also, the CDC’s findings are not stratified by age or other factors that make people more vulnerable to severe COVID-19.
- Updated monoclonal antibody treatment from Eli Lilly gets FDA authorization. During the Omicron surge, one challenge for healthcare providers has been that, out of three monoclonal antibody treatments authorized by the FDA, only one retained effectiveness against this variant. (Monoclonal antibody treatments provide a boost to the immune system for vulnerable patients.) This week, however, the FDA authorized an updated version of Eli Lilly’s treatment that does work against Omicron, including against the BA.2 lineage. The federal government has purchased 600,000 courses of this new treatment.
- More data released on South Africa’s mild Omicron wave. A new paper published in JAMA this week, from researchers at a healthcare provider in South Africa, compares COVID-19 hospitalizations during the Omicron surge to past surges. Among patients who visited the 49 hospitals in this provider’s network, about 41% of those who went to an emergency department with a positive COVID-19 test were admitted to the hospital during the Omicron surge—compared to almost 70% during South Africa’s prior surges. The paper provides additional evidence that Omicron is less likely to cause severe COVID-19 than past variants, though this likelihood is tied in part to high levels of vaccination and past infection in South Africa and other countries.
- Omicron has been identified in white-tailed deer. New York City was an early Omicron hotspot in the U.S.; and the variant has been passed onto white-tailed deer in Staten Island, according to a new preprint posted this week (and not yet peer-reviewed). Scientists have previously identified coronavirus infections in 13 states, but finding Omicron is particularly concerning for researchers. “The circulation of the virus in deer provides opportunities for it to adapt and evolve,” Vivek Kapur, a veterinary microbiologist who was involved in the Staten Island study, told the New York Times.
More variant reporting
-
The CDC is finally publishing wastewater data—but only ten states are well-represented
This week, the CDC added wastewater tracking to its COVID-19 data dashboard. Wastewater has been an important COVID-tracking tool throughout the pandemic, but it gained more public interest in recent months as Omicron’s rapid spread showed the utility of this early warning system. While the CDC’s new wastewater tracker offers a decent picture of national COVID-19 trends, it’s basically useless for local data in the majority of states.
Wastewater, as you might guess from the name, is water that returns to the public utility system after it’s been used for some everyday purpose: flushing a toilet, bathing, washing dishes, and so forth. In wastewater surveillance, scientists identify a collection point in the sewer system—either beneath a specific building or at a water treatment plant that handles sewage from a number of buildings. The scientists regularly collect wastewater samples from that designated point and test these samples for COVID-19 levels.
When someone is infected with the coronavirus, they are likely to shed its genetic material in their waste. This genetic signal shows up in wastewater regardless of people’s symptoms, so a wastewater sample may return a positive result for the coronavirus earlier than other screening tools like rapid antigen tests. And, because wastewater samples are typically collected from public sewer networks, this type of surveillance provides information for an entire community—there’s no bias based on who’s able to get a PCR or rapid test.
Scientists and organizations who utilize wastewater testing consider it an early warning system: trends in wastewater often precede trends in reported COVID-19 cases. For example, the coronavirus RNA levels identified in Boston’s wastewater shot up rapidly before Boston’s actual Omicron case numbers did, then also went down before case numbers did. Similarly, Missouri’s wastewater surveillance system—which includes genetic sequencing for variants—identified Delta cases last summer weeks before PCR testing did.
Wastewater surveillance is also a popular strategy for colleges and universities, which can set up collecting sites directly underneath student dormitories. Barnard College, where I went to undergrad, is one school that’s employed this strategy. At one point in the fall 2021 semester, the college instructed students living in the Plimpton residence hall (where I lived as a sophomore!) to get individual PCR COVID-19 tests because the wastewater surveillance program had found signals of the virus under their dorm.

Screenshot of the CDC’s new wastewater dashboard, retrieved on February 6. The CDC has been coordinating wastewater surveillance efforts since September 2020, Dr. Amy Kirby, team lead for the National Wastewater Surveillance System, said during a CDC media briefing on Friday. “What started as a grassroots effort by academic researchers and wastewater utilities has quickly become a nationwide surveillance system with more than 34,000 samples collected representing approximately 53 million Americans,” Kirby said.
It’s a little unclear why it took the CDC so long to set up a dashboard with this wastewater data when surveillance efforts have been underway for a year and a half. Still, many researchers and reporters are glad to see the agency finally publishing this useful information. The dashboard represents wastewater collection sites as colored dots: blue dots indicate that coronavirus RNA levels have dropped at this site in the last two weeks; yellow, orange, and red dots indicate RNA levels have risen; and gray dots indicate no recent data. You can download data from a dropdown beneath the dashboard and on the CDC’s data portal site.
“More than 400 testing sites around the country have already begun their wastewater surveillance efforts,” Kirby said at the media briefing. But she failed to mention that, out of these sites—the actual total is 471, according to the CDC dashboard—more than 200 are located in just three states: Missouri, Ohio, and Wisconsin. Missouri, with 80 sites, has a long-established system to monitor wastewater, through a collaboration between state agencies and the University of Missouri. Ohio has 71 sites of its own, while Wisconsin has 61.
After these Midwest wastewater powerhouses, other states with a relatively high number of collection sites include North Carolina with 38, Texas with 35, New York with 32, Utah with 31, Virginia with 29, Colorado with 21, and California with 17. No other state has more than 10 wastewater collection sites, and 18 states do not have any wastewater collection sites at all.
So, the CDC dashboard is pretty useful if you live in one of these ten states with a high number of collection sites. Otherwise, you just have to… wait for more sites in your area to get added to the dashboard, I guess? (Kirby did say during the media briefing that several hundred more collection sites are in development.) Even within the states that are doing a lot of wastewater surveillance, though, reporting is uneven at more local levels; for instance, many New York sites are concentrated in New York City and surrounding suburbs.
In this way, biased wastewater surveillance coverage in the U.S. echoes biased genetic sequencing coverage, an issue I’ve written about many times before. (See the genetic surveillance section of this post, for example.) Some states, like California, New York, and others with high-tech laboratories set up for sequencing, have identified variants for a much higher share of their COVID-19 cases than states with fewer resources.
The CDC gives wastewater treatment plants, local health departments, and research laboratories the ability to join its national surveillance network. But again, this is much easier for institutions in some places than others. Consider the resources available for wastewater sampling in New York City compared to in rural parts of the Midwest and South.
In addition, for places that do have robust wastewater surveillance systems, there are some caveats to the data, the CDC expert told reporters. Data may be hard to interpret “in communities with minimal or no sewer infrastructure and in communities with transient populations, such as areas with high tourism,” she said. “Additionally, wastewater surveillance cannot be used to determine whether a community is free from infections.”
If you’re looking for more wastewater data beyond the CDC tracker, here are two sources to check out:
- Biobot’s Nationwide Wastewater Monitoring Network, which I included in last week’s Featured Sources: This wastewater epidemiology company collects samples from water treatment facilities across the country; their dashboard includes both estimates of coronavirus levels in the U.S. overall and estimates for specific counties in which data are collected. Biobot’s data are available for download on Github. (Interestingly, it seems that some of the counties included in Biobot’s dashboard are not currently included in the CDC’s dashboard; I’ll be curious to see if that changes in the coming weeks.)
- COVIDPoops19 dashboard: This dashboard, run by researchers at the University of California Merced, provides a global summary of wastewater surveillance efforts. It includes over 3,300 wastewater collection sites tied to universities, public health agencies, and other institutions; click on individual sites to see links to dashboards, align with related news articles and scientific papers.
More federal data
-
BA.2 FAQ: What you should know about this Omicron offshoot

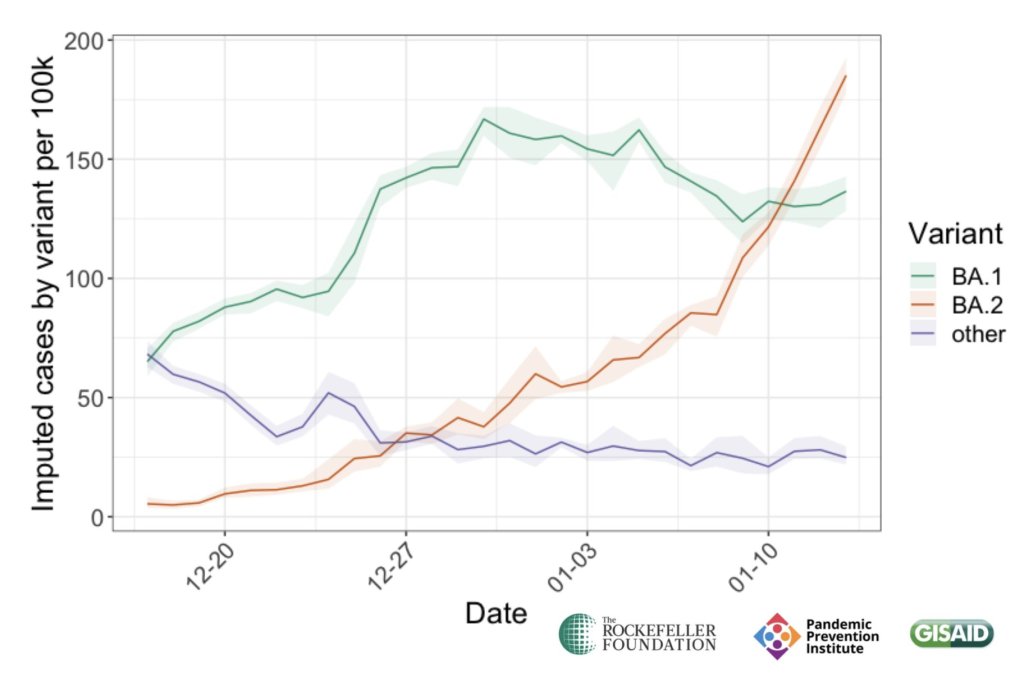
BA.2 has become the dominant strain in Denmark, one of the countries that sounded the alarm about this Omicron offshoot. Chart via the Pandemic Prevention Institute, posted on Twitter on January 26. An offshoot strain of the Omicron variant has been making headlines this week as it spreads rapidly in some European and Asian countries. While the strain, called BA.2 by virologists, has not yet been identified in the U.S. in large numbers, it’s already spreading here, too: scientists have picked it up in wastewater samples in some parts of the country.
This strain clearly has a growth advantage over the original Omicron strain (also called BA.1), but it’s not cause for major concern at this point. Scientists are working to identify whether BA.2 has a higher capacity for breaking through immunity from past infection or vaccination; so far, early data suggest that it does not significantly differ from BA.1 on this front, though it may have a slight advantage.
Here’s a brief FAQ on what we know about the strain so far.
When and where did BA.2 emerge?
I’ve been careful not to call BA.2 a “new strain” or a “new variant” here because it’s not actually new—at least, it’s not any newer than Omicron BA.1. When South African scientists first sounded the alarm about Omicron in late November 2021, BA.2 was already present among the country’s cases of this variant.
In fact, a paper from South African scientists describing the Omicron wave in their country, published in Nature in early January, specifies that the earliest specimen of BA.2 was sampled on November 17; the earliest specimen of BA.1 was sampled on November 8. Around the same time, South African scientists also identified a third lineage, called BA.3—this one hasn’t yet become a cause for concern.
Why are scientists concerned about BA.2?
In the past couple of weeks, epidemiologists have identified that BA.2 is spreading faster in some countries than BA.1, the original Omicron strain. This means BA.2 has what scientists call a “transmission advantage” over BA.1: it is capable of getting from person to person fast enough that it may be able to outcompete BA.1.
For example, in Denmark, BA.2 became the dominant strain in mid-January, taking over from BA.1. The takeover has coincided with an additional increase in COVID-19 cases in the country after Denmark’s Omicron wave initially appeared to peak a couple of weeks ago—but it’s hard to determine whether this second increase is solely due to BA.2 or also connected to an announcement that Denmark will end its COVID-19 restrictions on February 1.
This past week, the World Health Organization (WHO) announced that investigations into BA.2, including its potential virulence and ability to escape prior immunity, “should be prioritized independently (and comparatively) to BA.1.” The WHO has yet to designate BA.2 as a separate variant of concern from BA.1, however; at the moment, both strains are still included under the Omicron label.
How does BA.2 compare to BA.1, the original Omicron strain?
As I’ve explained in previous posts about the variant, Omicron has the most antigenic drift of any coronavirus variant identified thus far—meaning that it’s the most genetically different from the initial Wuhan version of the virus. Omicron BA.1 has about 60 mutations compared to the Wuhan strain, but BA.2 has even more: about 85 mutations, according to a recent Your Epidemiologist post.
BA.2 is clearly more transmissible than BA.1, as we’ve seen from its rapid spread in countries including Denmark, the U.K., France, the Netherlands, India, and the Philippines. Scientists estimate that “BA.2 may be 30% to 35% more transmissible than BA.1,” STAT News reports.
The question scientists hope to answer, then, is why BA.2 has this transmission advantage over BA.1. Do BA.2’s additional mutations lend it some adaptation in how it interacts with human cells, enabling faster spread? Or is BA.2 more capable of evading protection from past infection or vaccination compared to BA.1, leading it to cause more reinfections and breakthrough cases?
While we don’t know the answers to these questions yet, early data are indicating that there’s no major difference in disease severity between BA.1 and BA.2. In other words, BA.2 isn’t more likely to cause severe symptoms.
“There is no evidence that the BA.2 variant causes more disease, but it must be more contagious,” Danish Health Minister Magnus Heunicke said at a news conference last week, Reuters reported.
Why do some articles call BA.2 a “stealth variant?”
You might have seen some headlines referring to BA.2 as a “stealth variant” or a “stealth version of Omicron.” This is because of one major difference between BA.2 and BA.1: while BA.1 can be identified with a PCR test due to a key mutation that’s visible on PCR test results, BA.2 does not have this mutation.
As a result, BA.2 can be more time-consuming for COVID-19 testing labs to identify: labs need to sequence a sample’s genome to identify this strain rather than simply look out for an indicator on a PCR test. It’s unclear how much of a difference this will make in the U.S.’s ability to track BA.2, however, as many labs across the country are already performing routine full-genome sequencing of coronavirus samples.
How well do vaccines work against BA.2?
So far, it seems like there is no significant difference in vaccine protection between BA.1 and BA.2, at least when it comes to severe symptoms—which makes sense, scientists say, given how well vaccines have worked against every major variant to emerge thus far.
Early findings in this area come from the U.K., which designated BA.2 as a “Variant Under Investigation” (separate from BA.1) about a week and a half ago. This past Friday, the U.K.’s Health Security Agency released a report with information on BA.2, including how it compares to BA.1 or original Omicron.
Overall, U.K. epidemiologist Meaghan Kall wrote in a Twitter thread summarizing the report, early evidence suggests that “BA.2 is no more immune evasive than Omicron,” though confidence in this statement is low. The report found that, for Brits who had received booster shots, vaccine effectiveness against symptomatic COVID-19 disease was 70% for BA.2 and 63% for BA.1. The confidence intervals on these effectiveness estimates overlapped, indicating that vaccines perform similarly against BA.2 and BA.1.
When it comes to disease severity, Kall wrote, the U.K. doesn’t have enough data to compare BA.2 and BA.1; early data on this topic (suggesting BA.2 is not more severe) have come from Denmark and India.
How will BA.2 impact the U.S.’s COVID-19 trajectory?
BA.2 has already outcompeted BA.1 in some parts of Europe and Asia, and epidemiologists expect that countries like the U.K. and the U.S. could also follow this pattern—though it will likely be a longer, slower replacement process compared to the intense way Omicron pushed out Delta. A bigger unknown here is what effect this strain may have on case numbers, hospitalizations, and deaths.
Countries and regions now passing the peaks of their Omicron BA.1 waves have extremely high levels of population immunity. As a result, people who are fully vaccinated with boosters and/or recently infected with Omicron BA.1 likely will have a lot of immune system protection against BA.2, though we don’t yet have good data on exactly how robust this protection is.
So, could BA.2 cause the current downturn in U.S. COVID-19 cases to reverse? It’s possible, explains Andrew Joseph in a recent STAT News article. However, thanks to our high immunity levels, a further spike in cases could be “broadly limited to infections” rather than causing major increases in hospitalizations and deaths. In the coming weeks, we’ll get a better sense of how well prior Omicron infections protect against BA.2 and other key information that will inform our understanding of how this strain may change the country’s COVID-19 trajectory.
Right now, COVID-19 experts are closely monitoring BA.2, but they’re not hugely concerned. As Dr. Jetelina put it in a recent Your Local Epidemiologist post, the bigger worry right now is that another variant could “pop out of nowhere” like Omicron did in November.
More variant reporting
-
Omicron updates: Where will these massive case numbers leave us?

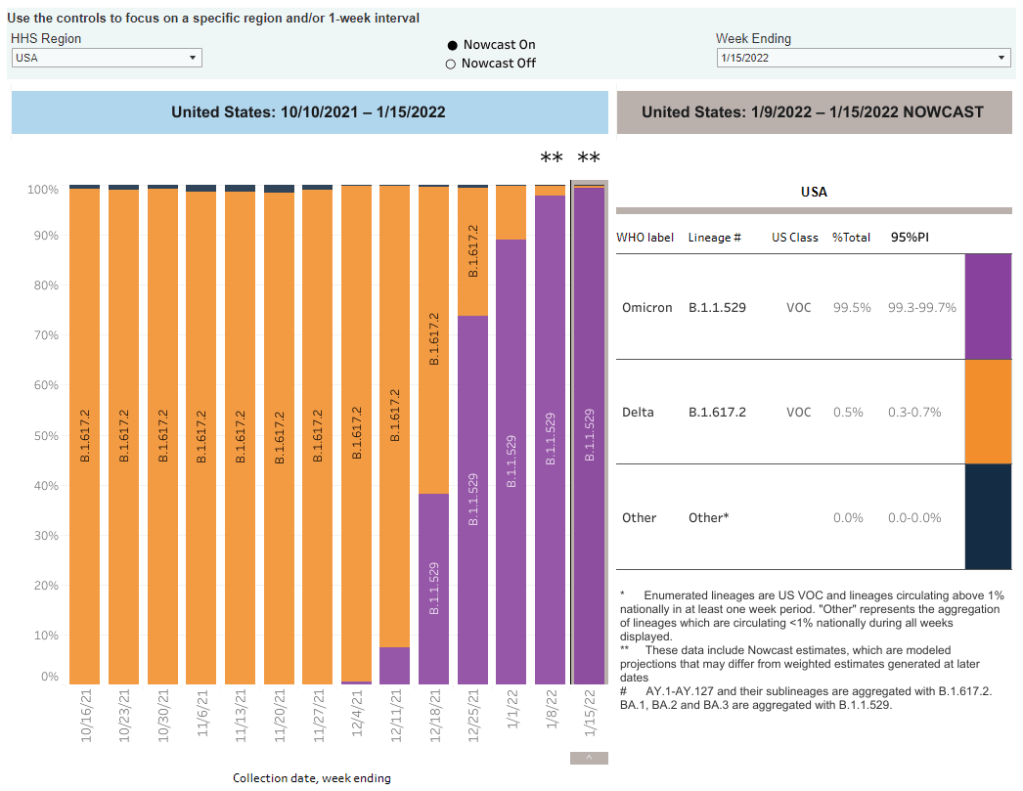
Omicron went from 1% of U.S. cases to nearly 100% of cases in about six weeks. Chart via the CDC, retrieved January 23. Major news items for this week include the potential peak of the U.S.’s Omicron surge and real-world data from the CDC on how well booster shots work against this variant.
- Omicron is now causing nearly 100% of new COVID-19 cases in the U.S. The latest CDC estimates of variant prevalence put Omicron at 99.5% of new cases in the U.S. as of January 15, with Delta causing the remaining 0.5% of cases. I have to say, it’s incredibly striking not only how quickly Omicron outcompeted Delta (it went from 1% of new cases to nearly 100% in just six weeks), but also how both of these highly contagious variants have dominated the country so thoroughly that they’re now the only two variants present here at all. For comparison, Alpha only got to 70% of cases at its peak. These trends show how drastically both Delta and Omicron changed the trajectory of the pandemic.
- While the U.S. may be peaking, massive numbers of people are getting infected. As I noted in today’s National Numbers, America’s Omicron wave may have peaked this week, with the country’s massive case growth appearing to turn around. Computational biologist Trevor Bedford wrote a recent Twitter thread about this peak, pointing out that a huge share of the U.S. population was infected with Omicron in the past month: “between 18% and 23% of the country was infected by Omicron by Jan 17, with the large majority infected in a span of just ~4 weeks,” he hypothesized. By mid-February, Bedford says, this number could be “36%-46%.”
- The high infection numbers may give us “a bit of a break from the Covid roller coaster.” With so many people infected in such a short time, Omicron will have a huge impact on the “immunological landscape” of the U.S, Helen Branswell explains in a recent article for STAT News. Millions will have immunity from a recent infection, vaccination, or both; and Omicron’s unique biology may mean that people who caught this variant will be protected from other strains. As a result, the end of this wave may lead into “a bit of a break” from COVID-19, Branswell writes, with low case numbers for a few weeks or months. It’s hard to say whether this “break” will constitute the end of the pandemic, though—we don’t know how long post-Omicron immunity lasts.
- Rapid at-home tests work well at detecting Omicron, though they’re far from perfect. As I’ve noted in past issues, there have been some questions recently about how well rapid antigen tests work at identifying Omicron infections. In a recent Your Local Epidemiologist post, Dr. Katelyn Jetelina walked through the data from several recent studies on this topic. The highlights: rapid tests likely won’t work well in the very beginning of an infection, so wait to test until five days after an exposure; if you test positive, trust the result; test repeatedly for higher accuracy; and, if you have the tests, wait for two negative results before coming out of isolation.
- New CDC wastewater report shows how early Omicron was spreading in the U.S. The CDC published a report this week sharing findings from wastewater surveillance systems in a few states and localities. (Wastewater surveillance means the states are regularly testing samples from sewage to identify coronavirus levels coming from residents’, well, waste.) In New York City, Omicron was first detected in wastewater on November 21, the weekend before Thanksgiving. In California, Colorado, and Houston, Texas, the variant was detected in late November or early December.
- An additional booster shot may not be enough to completely prevent Omicron infection, a small Israeli study suggests. Israel was one of the first countries to offer third vaccine doses to its residents, and now it’s also one of the first countries offering fourth doses. A new study presents the impact of these shots among about 270 healthcare workers. The additional doses produced more antibodies in the patients, but “this is probably not enough for the Omicron,” one of the study’s authors told Reuters—at least when it comes to completely preventing infection.
- But: booster shots still reduce chances of infection significantly, compared to people who are unvaccinated. Another new CDC report published this week compares COVID-19 cases among vaccinated, boosted, and unvaccinated people in 25 U.S. jurisdictions. In late December, after Omicron started spreading widely, adults who were unvaccinated had a five times higher risk of COVID-19 infection compared to those who were fully vaccinated with a booster shot, the CDC found.
- Booster shots also have a huge impact on risks of severe symptoms and hospitalization. One more CDC report released this week: scientists analyzed the impact of booster shots on emergency department visits and other hospitalization metrics in ten states. When both Delta and Omicron were the dominant variants in the U.S., the CDC researchers found, third doses had 94% efficacy rates in protecting people against COVID-related emergency department visits, and 82% efficacy rates in protecting against urgent care visits. Efficacy against hospitalization was also over 90%. In short: if you’re eligible for your booster, go get it!
- Booster shots of Pfizer and Moderna vaccines could be critical for countries that used other brands. Last week, I shared a report that found 22 million mRNA vaccine doses are needed as booster shots in low-income countries, to protect the world against Omicron. This past week, a new study in Nature supported this report: a group of scientists in Hong Kong found that Pfizer doses are safe and highly effective booster shots for people who initially received the Chinese CoronaVac vaccine. The authors suggest that mRNA vaccines should be used as boosters in countries that originally distributed CoronaVac.
- New research identifies a mutation that may contribute to Omicron’s super-contagiousness. A new study from the National Institutes of Health (NIH) found that a mutation present in the Alpha and Delta variants allows the coronavirus to more easily bind to human cells. When the coronavirus binds more easily, it can spread faster within the body; this rapid multiplication helps the virus quickly spread outside the body as well, increasing contagiousness. Though this study was done before the Omicron variant emerged, Omicron has this same mutation, explained lead author Dr. Lawrence Tabak in a post for the NIH Director’s Blog.
More variant reporting
-
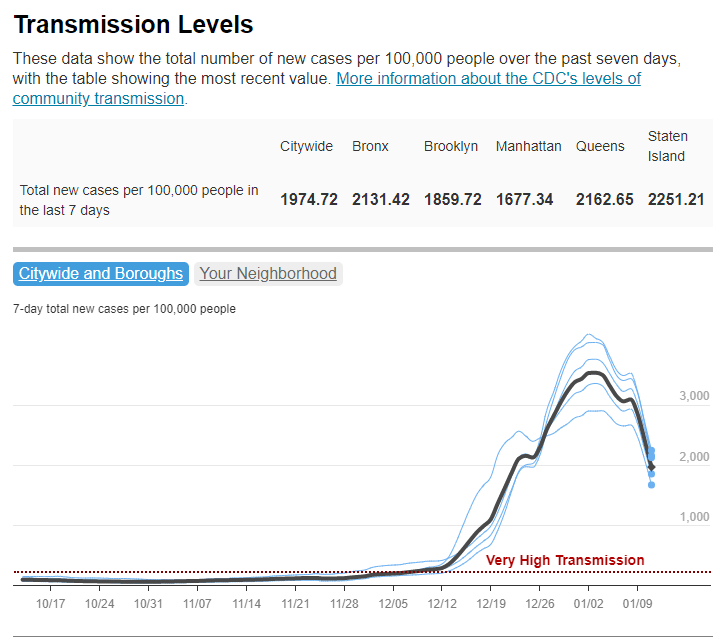
Omicron updates: Possible peaks, viral loads, vaccines
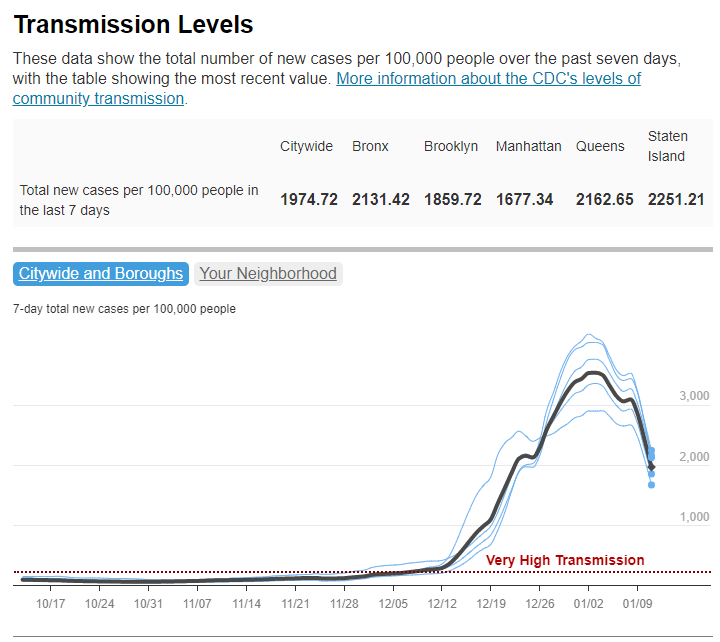
Has Omicron peaked in NYC? It sure seems like it, according to city data; screenshot retrieved from NYC Health dashboard on January 16. These update posts are getting shorter as time goes on, but we’re still learning about this variant! A few news items from this week:
- Omicron is now causing almost 100% of new COVID-19 cases in the U.S. In the CDC’s latest variant proportions update, the agency estimated that 98% of new COVID-19 cases were caused by Omicron in the week ending January 8. The CDC also revised estimates for previous weeks, though the revisions were not as significant as they have been in the past—suggesting that the numbers are now fairly close to accurate, but will continue to be tweaked as more sequencing data come in.
- Major Northeast hotspots appear to be peaking. Last week, I wrote that New York City’s Omicron wave seemed to have reached its peak. The trend has continued into this week: the new case rate and test positivity rate have both fallen consistently since peaking on January 3. Similarly, in Boston, the Omicron levels detected in the city’s wastewater have declined steeply since early January. The daily case rate is also going down in Washington, D.C., and in the Northeast region overall. Still, hospitals are still overwhelmed throughout the region, and it’s unlikely that cases will go down as quickly or as decisively as they went up.
- New NYC report provides data on the city’s Omicron wave. Speaking of NYC: the city’s public health department recently put out a new report detailing the variant’s impact. The variant “has accounted for nearly all coronavirus samples sequenced in NYC” since Christmas, the report’s authors write. Also, while a smaller share of Omicron cases led to hospitalization compared to the Delta wave, more people have been hospitalized overall because of sheer case numbers. Unvaccinated New Yorkers, Black New Yorkers, and those over age 75 have been most likely to require hospitalization.
- Real-world study suggests rapid at-home tests work well at detecting Omicron. A new study from the University of California, San Francisco, released this week as a preprint, analyzed rapid antigen tests’ capacity to detect Omicron by comparing rapid test results to PCR test results. The results: antigen tests correctly identified 95% of cases with high viral loads and 98% of symptomatic cases. In about one-third of the cases identified through PCR, patients tested negative on antigen tests; but this is in line with the tests’ accuracy for other variants.
- Data from the NBA suggest Omicron’s viral load is pretty variable. Another new study posted as a preprint this week analyzed data from the National Basketball Association (NBA). The league’s regular testing policy allowed Harvard researchers to study viral loads in Omicron-positive patients, revealing that this variant had “lower peak viral load and more variable early viral growth durations than Delta,” according to one of the authors. In other words, some of the basketball players were highly contagious early into their Omicron infections, while others were less so; and the players had less virus in their bodies overall at the peak of their infections than in previous Delta infections. Also, a large number of the players were still contagious five days after they were diagnosed—which doesn’t bode well for the CDC’s new isolation guidance.
- More confirmation that vaccinated people are protected from severe disease from Omicron. Another new study, this one published in Nature through the journal’s advance preview system for COVID-19 reports, confirms previous research about T cell response to Omicron. T cells are a key part of the immune system’s long-term memory apparatus; they help protect against severe symptoms and death. The study found that, in patients who were fully vaccinated (or, to a lesser degree, had a previous infection), T cells could recognize Omicron and protect people against its worst impacts.
- Omicron adds urgency to the need to vaccinate the world—ideally, with mRNA vaccines. A report from advocacy groups PrEP4All and Partners In Health, written with scientists at Harvard, Columbia, and other institutions, found that 22 billion additional mRNA vaccine doses are needed to control the pandemic, now that Omicron has become the dominant variant in the world. The report specifies that mRNA vaccines are needed because other vaccine types are not capable of preventing Omicron infection, and likely are less effective against severe disease. “Future viral variants may become even more transmissible, immune evasive, and virulent than Delta or Omicron,” the report cautions.
More variant reporting
-
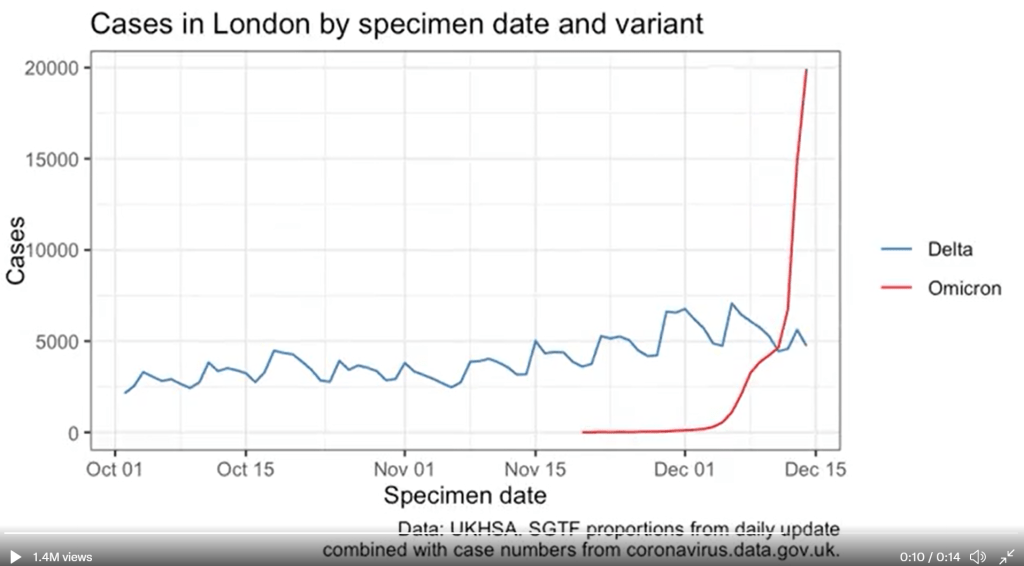
Omicron updates: Spreading rapidly in the U.S.
We keep learning about this dangerous variant as it spreads through the U.S. and the world. A few major updates from this week:
- Omicron is spreading rapidly in the U.S. Last Tuesday, the CDC announced that Omicron had gone from causing 0.4% of new COVID-19 cases nationwide in the week ending December 4, to 2.9% of cases in the week ending December 11. That’s a seven-fold increase over the course of a week; the variant appears to be doubling every two to three days, based on data from the U.K. We can assume that it will be the dominant variant in the U.S. by the end of December, if not sooner.
- U.K. data provides information on just how fast Omicron can spread. The U.K.’s comprehensive genomic surveillance system, combined with its unified national public health system, allows British researchers to analyze their country’s Omicron cases in high detail. According to the latest briefing from the U.K. Health Security Agency (summarized by Meaghan Kall): risk of reinfection with Omicron is three to four times higher than with Delta; risk of household transmission with Omicron is two to three times higher than with Delta; and the variant is doubling every two days—or even every 1.5 days, in some parts of the U.K.

Omicron’s rapid spread in London, compared with prior Delta cases. Chart by Theo Sanderson; see his Twitter for the full animated version. - New research from Hong Kong provides insight into why Omicron spreads so fast. Preliminary data from a Hong Kong University research team suggests that, within 24 hours of an Omicron infection, the virus “multiplied about 70 times faster inside respiratory-tract tissue than the Delta variant,” reports Megan Molteni at STAT News. More virus in the respiratory tract means more virus getting out into the air, Molteni explains. At the same time, the variant seems to be worse at multiplying within lung tissue, which may contribute to milder disease. While the Hong Kong study has yet to be peer reviewed, this finding aligns with reports of superspreading events among fully vaccinated people.
- Skepticism about “Omicron being mild” continues despite more reports. Early this week, the largest health insurance company in South Africa posted results of a study examining the country’s Omicron wave. The study found that risk of hospitalization was 29% lower for Omicron patients than it had been during the country’s spring 2020 COVID-19 surge. While this finding follows other reports out of South Africa, experts are still skeptical: in part because it can take weeks for a coronavirus infection to progress to hospitalization, and in part because South Africa’s population has a lot of prior immunity from past surges and vaccinations. Also, a “milder” variant that’s more transmissible can still lead to significantly more hospitalizations.
- We’re getting more evidence that vaccination protects against severe disease from Omicron. Basically: two shots are good, three shots are better. “Though these data are preliminary, they suggest that getting a booster will help protect people already vaccinated from breakthrough or possible severe infections with Omicron during the winter months,” writes NIH Director Dr. Francis Collins in a recent blog post summarizing both laboratory and real-world studies. If you’re eligible for a booster and haven’t yet gotten it, now is a great time.
- But: We don’t know how well vaccines protect against Long COVID from an Omicron infection. As many experts continue to say that Omicron cases are mild for those who are vaccinated, the Long COVID experts and advocates I follow have pointed out that a mild breakthrough case can still lead to this prolonged condition. “Omicron is a huge individual threat,” wrote Long COVID researcher Hannah Davis on Twitter recently. “A 15-30% chance of being disabled for at least a year, but likely for the rest of your life, is a bigger threat than most of us ever faced ever before the pandemic.”
- New York City is an Omicron hotspot in the U.S. As I noted in today’s National Numbers post, this variant has clearly hit NYC, as seen in record case numbers and felt in long lines for testing throughout the city. According to CDC estimates, Omicron was causing about 13% of new cases reported in New York and New Jersey in the week ending December 11. One week later, knowing how fast Omicron has outcompeted Delta in the U.K. and elsewhere, we can assume that it’s now causing the majority of cases in this region.
- Other U.S. states and regions may be behind in their Omicron sequencing, so assume it’s spreading in your area even if it hasn’t been officially identified yet. As I’ve written before, genomic surveillance in the U.S. is geographically very spotty. NYC is a clear hotspot, but it’s also a city with a lot of sequencing infrastructure. In other parts of the country, Omicron may not have been formally identified yet—but that doesn’t mean it isn’t spreading. Take Orlando, Florida as an example: wastewater sampling in the surrounding county found that Omicron was completely dominating the community this week, according to AP, even though “practically no cases of clinical infection” have been reported.
- Good news: South Africa’s case numbers are now trending down. As of yesterday, COVID-19 case numbers in Gauteng, the center of South Africa’s COVID-19 outbreak, as well as in other parts of the country, seem to be turning around. Computational biologist Trevor Bedford offered some potential explanations in an interview with New York Magazine: limited testing capacity and milder disease may lead to underreporting of COVID-19 cases in South Africa; less of the population may be susceptible due to prior immunity; and the variant may spread so fast that it can quickly burn through social networks and other avenues of transmission. We’ll need to see whether South Africa’s decline holds, and whether we see similar patterns in other Omicron hotspots.
- The U.S. is not prepared for an Omicron surge. If you haven’t yet, take some time today to read Ed Yong’s latest feature in The Atlantic, which discusses how the U.S. has failed to learn from past COVID-19 outbreaks and prepare for the Omicron surge that has already arrived. “Rather than trying to beat the coronavirus one booster at a time, the country needs to do what it has always needed to do—build systems and enact policies that protect the health of entire communities, especially the most vulnerable ones,” Yong writes.
- Omicron has altered the trajectory of the pandemic. Another piece to take time for today is this article in Science by Kai Kupferschmidt, discussing the “really, really tough winter” that scientists now see coming. Kupferschmidt explains that, even if many Omicron cases are mild, the variant is still spreading fast enough that it could land a lot of people in the hospital. In addition, the variant “may bring other, unpleasant evolutionary surprises” if future coronavirus variants evolve out of Omicron, Kupferschmidt writes.
More variant reporting