Like everyone else, I spent Wednesday afternoon watching rioters attack the nation’s Capitol. I was horrified by the violence and the ease with which these extremists took over a seat of government, of course, but a couple of hours in, another question arose: did this coup spread COVID-19?
The rioters came to Washington D.C. from across the country. They invaded an indoor space in massive numbers. They pushed legislators, political staff, and many others to hide in small offices for hours. They inspired heated conversations. And, of course, none of them wore masks. These are all perfect conditions for what scientists call a superspreading event—a single gathering that causes a lot of infections.
(The number can vary, based on how you define a superspreading event; for more background, see this post from November.)
My concerns were quickly echoed by many other COVID-19 scientists and journalists:
The very next day, Apoorva Mandavilli published a story asking just this question in the New York Times. She quotes epidemiologists who point out that the event was ripe for superspreading among both rioters and Capitol Hill politicians. Many legislators were stuck together in small rooms, having arguments, while some of the Republican representatives refused to wear masks. POLITICO got a video of several Republicans refusing masks in a crowded safe room.
By Friday, five Congressmembers had tested positive for COVID-19 in a week. It’s true, many of these legislators received vaccines in the first stage of the U.S. rollout in late December. But it takes several weeks for a vaccine to confer immunity, and we still don’t have strong evidence as to whether the Pfizer and Moderna vaccines prevent the coronavirus from spreading to other people. (They likely do, to some extent, but the evidence mainly shows that these vaccines prevent COVID-19 disease.)
Just this morning, Punchbowl News’ Jake Sherman reported that the attending physician for Congress sent a note to all legislators and staff, warning them that “people in the safe room during the riots may have been exposed to the coronavirus.” I will be carefully watching for more reports of legislators testing positive in the coming weeks. From our nation’s previous experience with COVID-19 outbreaks at the White House, it seems unlikely that the federal government will systematically track these cases—though the incoming administration may change this.
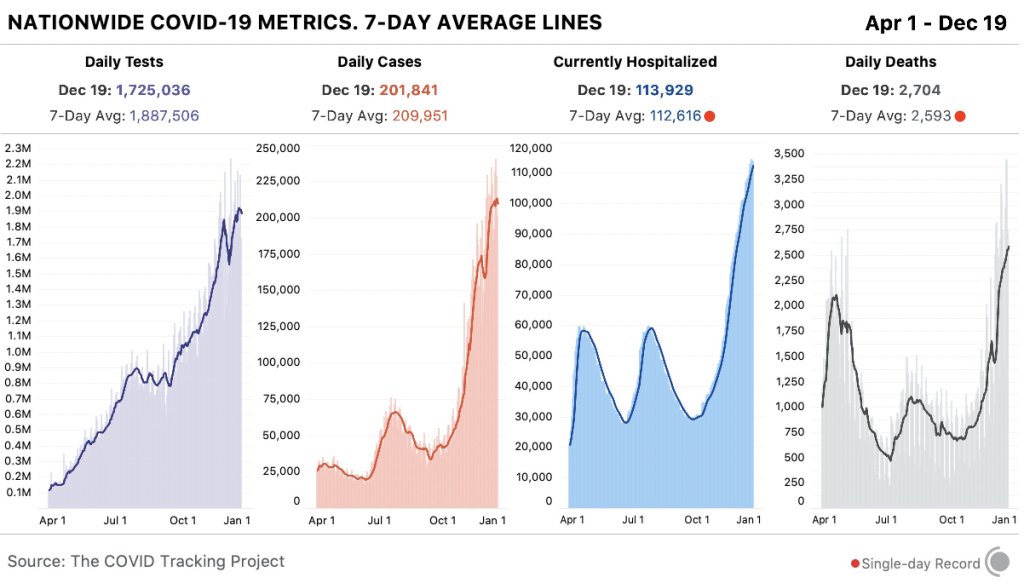
As for the rioters themselves, while the events of January 6 may well have been superspreading, we likely will never know the true extent of this day’s impact. As I’ve written previously, we identify superspreading events through contact tracing, the practice of calling up patients to quiz them on their activities and help identify others who may have gotten sick. When case numbers go up—as they are now—it becomes harder to call up every new patient. One county in Michigan is so understaffed right now, it’s telling COVID-19-positive residents to contact trace themselves.
But even if contact tracing were widely available in the communities to which those rioters are going home, can you really imagine them answering a phone call from a public health official? Much less admitting to an act of treason and risking arrest? No, these so-called patriots likely won’t even get tested in the first place.
It would take rigorous scientific study to actually tie the Capitol riot to COVID-19 spread to the homes of the rioters. (That said, if you see a study like that in the months to come: please send it my way.)
Finally, I have to acknowledge one more impact of the riot on D.C. at large: vaccine appointments were canceled after 4 PM that day. One of the most heinous aspects of that riot, to me, was how it pulled our collective attention away from the pandemic, precisely at a time when our collective health needs that attention most.