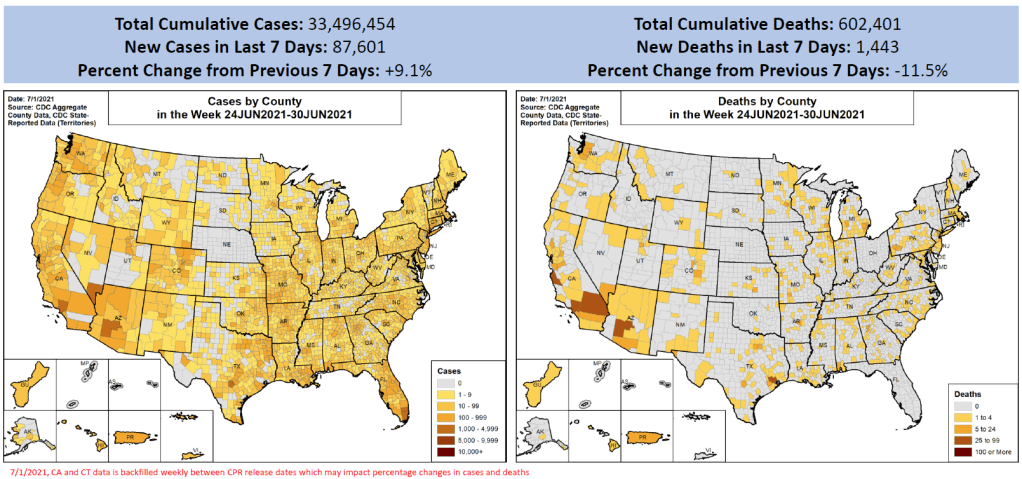
In the past week (June 26 through July 2), the U.S. reported about 88,000 new cases, according to the CDC. This amounts to:
- An average of 12,500 new cases each day
- 27 total new cases for every 100,000 Americans
- 9.1% more new cases than last week (June 19-25)
Last week, America also saw:
- 13,000 new COVID-19 patients admitted to hospitals (4.0 for every 100,000 people)
- 1,400 new COVID-19 deaths (0.4 for every 100,000 people)
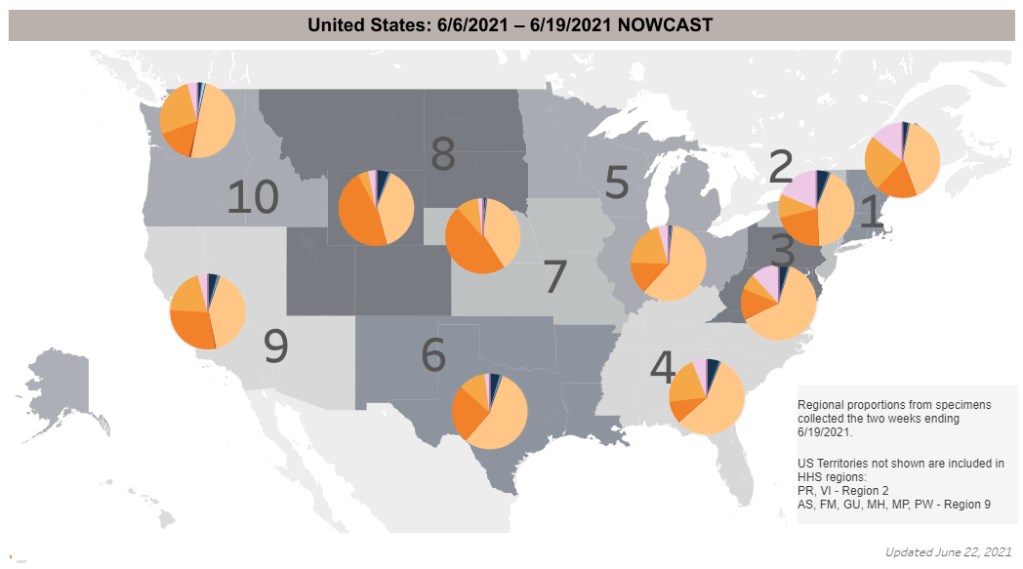
- 26% of new cases now Delta-caused (as of June 19)
- An average of 1.1 million vaccinations per day (per Bloomberg)
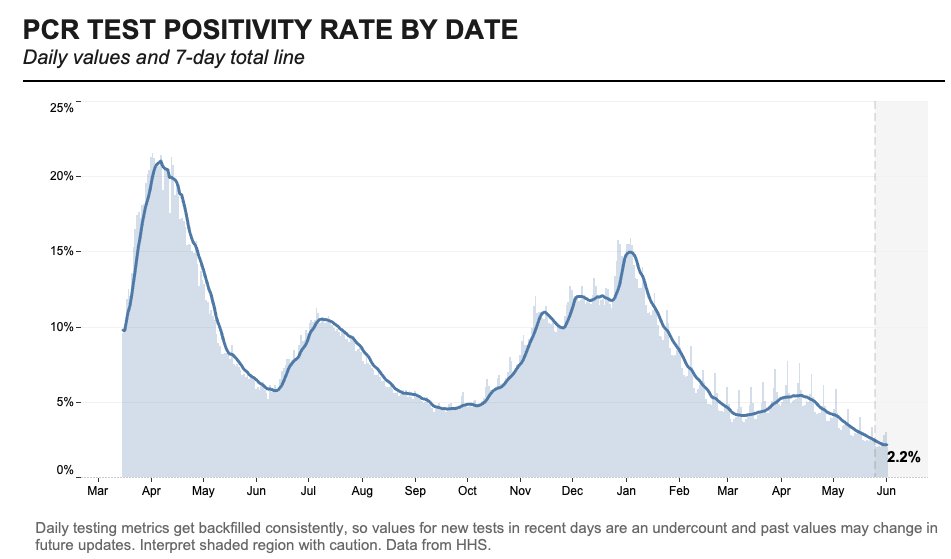
This is the first week since April that we’ve seen new COVID-19 case numbers go up in the U.S. It’s nominally a small bump—about 7,300 more cases than last week—but represents a 9% increase, and may be the beginning of a summer surge. (Even if we see a dip in the numbers this week due to the July 4 holiday.)
The culprit for this case rise is, of course, the Delta variant (B.1.617.2). According to CDC estimates, the variant makes up about 26% of new cases in the country. But, as I have explained in previous issues, the CDC data are old—that 26% estimate is as of June 19, about two weeks ago.
The Delta variant is doubling every two weeks, so we can assume that the variant now causes at least half of new cases in the U.S. Estimates from other genomic sequencing sources (which are more up-to-date than the CDC, though less comprehensive) indicate that the variant may now be causing up to 60% of new cases.
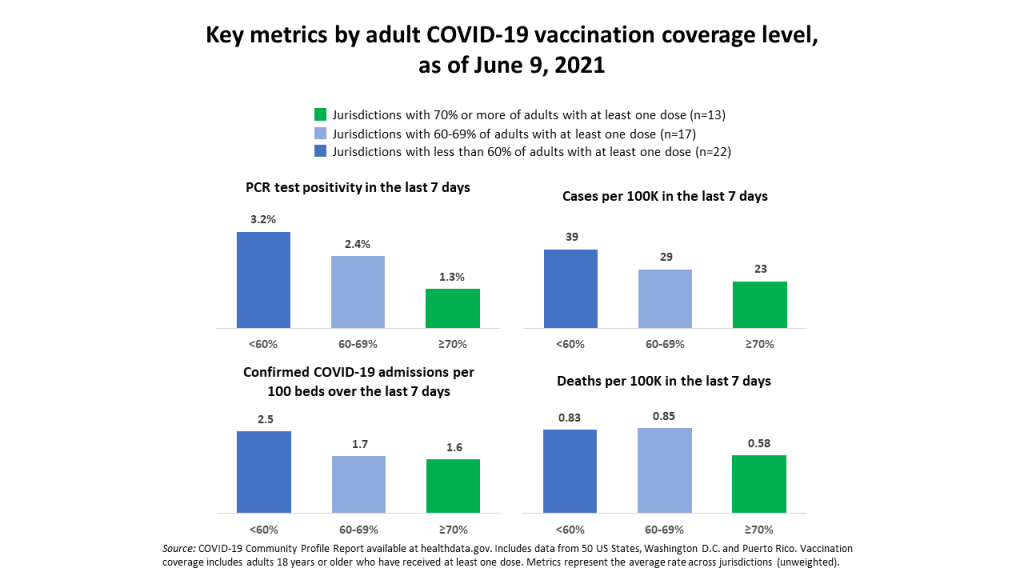
This variant poses the most danger to unvaccinated people; many of the current Delta outbreaks are happening in regions with lower vaccination rates. Nevada and Missouri, the two states with the highest new case counts last week, have about 42% and 39% of their populations fully vaccinated, respectively.
Some metropolitan areas in Missouri, Texas, and other parts of the Midwest have less than one-third of their populations fully vaccinated—and saw more than 200 new cases for every 100,000 people last week. That’s about seven times the national average for new cases.
Nationally, hospitalizations also rose very slightly this week, while deaths remained low, at about 200 new COVID-19 deaths each day. The vaccines continue to protect seniors and other more vulnerable people from severe disease. But it is likely that, in the coming weeks, these numbers will start to rise in the areas seeing Delta outbreaks. Many Midwest hospitals are already filling up.
More on vulnerable, non-vaccinated pockets later in this issue.