Editor’s note, November 27: Check out my new publication: The Sick Times, a new nonprofit news site chronicling the Long Covid crisis.
After more than three years, 165 weekly newsletters, and a lot of number-crunching, this is the last issue of the COVID-19 Data Dispatch. I am bidding farewell to this publication, with immense gratitude to everyone who has supported it. But this isn’t the last newsletter you’ll get from me about COVID-19 research and data; more on that below.
I’m ending the COVID-19 Data Dispatch for three reasons. First, there is simply less day-to-day COVID-19 data news these days than there was early in the pandemic. When I started writing this publication in summer 2020, there was a constant stream of data issues to explain, new resources coming online, confusing trends, and more. The stream has slowed a lot in the last year, especially after the federal public health emergency ended in May.
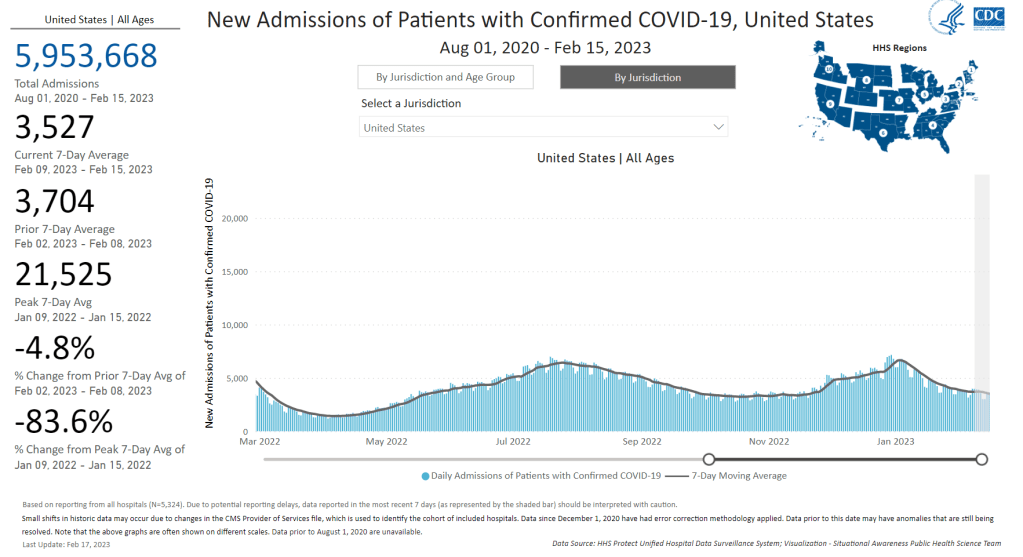
The COVID-19 pandemic certainly isn’t over, and COVID-19 is certainly still a significant health threat in the U.S. and all over the world. Millions of people continue to get this disease every week, of whom thousands go to the hospital, hundreds die, and many more are left with Long COVID. However, the specific focus area that I chose for this publication—data and surveillance—is no longer an active topic requiring dedicated coverage. Post-health emergency, U.S. data systems have settled into tracking COVID-19 with a similar lack of urgency to their tracking of other seasonal diseases, leaving me with less to write about on a weekly basis.
Second, writing a publication solo is a lot of work, and I’ve felt myself inching closer to burnout in recent months. I’ve primarily written the CDD on weekends, in my spare time from freelance projects. When I started this newsletter, the process worked well because CDD topics often lent themselves to later freelance articles and vice versa. These days, there’s less overlap, as media publications are less interested in COVID-19 news. While I’ve appreciated having this space to keep covering the topic, it has taken more time and energy to figure out what I’m writing from week to week. The weekly newsletter has felt less like a “passion project,” and more like a chore, which is always a red flag for me.
And the third reason is the most important: I’m getting ready to transition into a new publication. In the new publication, I will continue covering COVID-19—but with a new focus area. I’m also transitioning from a solo project to one with a team, which we hope will grow as the project receives donations and grant funding. I’m not sharing too many details here because this publication hasn’t been announced publicly yet, but you can expect to learn more about it soon.
Specifically: if you’re a COVID-19 Data Dispatch newsletter subscriber, expect an email from me in the coming days introducing my new publication. You’ll be welcome to unsubscribe from my emails if you aren’t interested in the new project; though I hope you’ll find that it will serve to help you navigate the continued pandemic just as the CDD has.
In the meantime, feel free to email me with any questions or concerns you have. And thank you for all the support over the last three years—for the comments, the questions, the donations, and the building of a small community that refuses to simply move on from the ongoing COVID-19 crisis. Thank you.