- New vaccination data from the CDC: The CDC has started publishing vaccination data reflecting how many Americans have received COVID-19, flu, and RSV shots in fall 2023. These numbers are estimates, based on the CDC’s National Immunization Survey, as the agency is no longer directly compiling COVID-19 vaccinations from state and local health agencies. (See this post from last month for more details.) According to the estimates, about 28% of American adults have received a 2023 flu shot, compared to 10% who have received a 2023 COVID-19 shot. The numbers reflect poor communication about and accessibility challenges with this year’s COVID-19 vaccines.
- FDA approves a rapid COVID-19 test: Following the end of the federal public health emergency this spring, the FDA has advised companies that produce COVID-19 tests to submit their products for full approval, transitioning out of the emergency use authorizations that these tests received earlier in the pandemic. The FDA has now fully approved an at-home COVID-19 test: Flowflex’s rapid, antigen test. This is the second at-home test to receive approval, following a molecular test a few months ago. The Floxflex test “correctly identified 89.8% of positive and 99.3% of negative samples” from people with COVID-like respiratory symptoms, according to a study that the FDA reviewed for this approval.
- WHO updates COVID-19 treatment guidance: This week, the World Health Organization updated its guidance on drugs and other treatment options for severe COVID-19 symptoms. A group of WHO experts has regularly reviewed the latest evidence and updated this guidance since fall 2020. The update includes guidelines on classifying COVID-19 patients based on their risk of potential hospitalization, recommendations for drugs such as nirmatrelvir and corticosteroids, and recommendations against other drugs such as invermectin and hydroxychloroquine. Clinicians can explore the guidance through an interactive tool that summarizes the expert group’s findings.
- Gargling with salt water to reduce symptoms: Speaking of COVID-19 treatments: gargling with salt water may help people with milder COVID-19 symptoms recover more quickly, according to a new study presented at the American College of Allergy, Asthma and Immunology’s annual conference. The researchers compared COVID-19 outcomes among people who did and did not use salt water for 14 days while sick; those who used the treatment had lower risks of hospitalization and reported shorter periods of symptoms. This study has not yet been peer-reviewed and more research will be needed, but it’s still helpful evidence to back up salt water as a potential treatment (something I’ve personally seen recommended anecdotally in the last couple of years).
- Allergies as potential Long COVID risk factors: Another study that caught my attention this week: researchers at the University of Magdeburg in Germany conducted a review of connections between allergies and Long COVID. The researchers compiled data from 13 past papers, including a total of about 10,000 study participants. Based on these studies, people who have asthma or rhinitis (i.e. runny nose, congestion, and similar symptoms, usually caused by seasonal allergies) are at higher risk for developing Long COVID after a COVID-19 case. The researchers note that this evidence is “very uncertain” and more investigation is needed; however, the study aligns with reports of people with Long COVID getting diagnosed with mast cell activation syndrome (or MCAS, an allergy-related condition).
- Dropping childhood vaccination rates: One more notable study, from the CDC’s Morbidity and Mortality Weekly Report (MMWR): vaccination rates for common childhood vaccines are declining among American kindergarteners, according to CDC research. CDC scientists reviewed data reflecting the childhood vaccinations that are required by 49 states and D.C. for the 2022-23 school year, and compared those numbers to past years. Overall, 93% of kindergarteners had completed their state-required vaccinations last school year, down from 95% in the 2019-20 school year, while vaccine exemptions increased to 3%. In 10 states, more than 5% of kindergarteners had exemptions to their required vaccines—signifying increased risk of vaccine-preventable disease outbreaks in schools, according to the CDC.
Tag: vaccine for kids
-
Sources and updates, November 12
-
COVID-19 vaccine issues: Stories from COVID-19 Data Dispatch readers across the U.S.

Last year, just 17% of the U.S. population received a bivalent booster. Will this year’s uptake be better? Last week, I asked you, COVID-19 Data Dispatch readers, to send me your stories of challenges you experienced when trying to get this fall’s COVID-19 vaccines. I received 35 responses from readers across the country, demonstrating issues with insurance coverage, pharmacy logistics, and more.
I’ve published the full responses in the table below. Here are a few common themes that I saw in these stories:
- Pharmacies aren’t receiving enough vaccines. Several readers shared that their pharmacies had inadequate vaccine supply to accommodate all the people who made vaccination appointments, or who wanted appointments. Vaccine supply may also be unpredictable—a pharmacy may think they’re getting more shots, but in fact not receive them—leading to appointment cancellations.
- Insurance providers weren’t prepared for this vaccine rollout. Despite months of advance notice that a fall COVID-19 vaccine was coming, many insurance companies apparently failed to prepare billing codes or other system updates that would allow them to cover the shots. A couple of people who shared insurance issue stories are on Medicare—representing a population (i.e. seniors) who should be at the front of the vaccine line.
- Very limited, confusing vaccine availability for young kids. Several readers shared that they were able to get vaccinated, but their children under 12 have not received a vaccine yet. While the FDA and CDC have authorized this fall’s COVID-19 vaccines for all Americans ages six months and older, younger children require a different vaccine formulation from adults. And this formulation appears either entirely unavailable or very difficult to access, depending on where you live.
- People living in less dense areas may need to travel. A few readers shared that, as they searched for vaccine appointments in their areas, the closest pharmacies with doses available were miles away—over 10 miles, in one case. This is a significant barrier for people fitting vaccine appointments into their work schedules.
- Information may be inconsistent. Vaccine availability listed in one place (such as a pharmacy chain’s website or the federal vaccines.gov website) may be inaccurate in another. Some readers shared that they spent extra time on the phone with pharmacies or health providers to get accurate information—another barrier.
- Pharmacies don’t have enough staff for this. Even readers who were able to receive COVID-19 vaccines often had to wait a long time at their pharmacies. Several shared that their pharmacies appeared to be understaffed, dealing with the COVID-19 shots along with routine prescriptions and other duties. The days of mass vaccination sites, efficiently run by public health departments, are long over.
- Kaiser Permanente members face delays. One company that appears to be causing outsized problems is Kaiser Permanente, one of the biggest insurers and health providers on the West Coast. Several readers shared that Kaiser was not providing new COVID-19 vaccines until early October, and would not cover the shots if their members went to another location. That’s a big delay, and it may be further impacted by a coming strike at the company.
- These vaccines are expensive. If you decide to pay for a COVID-19 shot out-of-pocket (as some readers did), it costs almost $200. Even the federal government is paying about triple the cost of last year’s COVID-19 vaccines per shot, for the doses it is covering, STAT News reports. The U.S. may have received a “bad deal” here, STAT suggests, considering all of the federal funding that’s supported vaccine research and development.
As I wrote last week, some news outlets have covered these challenges, but this issue really deserves more attention. The updated COVID-19 vaccines are basically the U.S. government’s only strategy to curb a surge this winter, and they should be easily, universally accessible. Instead, many people eager to get vaccinated are going through multiple rounds of appointments, phone calls, pharmacy lines, and more.
For every one of these readers who has persisted in getting their shot, there are likely many other people who tried once and then gave up. And those people who don’t receive the vaccine will be at higher risk of severe illness, death, and long-term symptoms from COVID-19 this fall and winter. This is a public health failure, plain and simple.
And it’s important to emphasize that this failure is not surprising. Many health commentators predicted that these challenges would arise as the federal public health emergency ended and COVID-19 tools transitioned from government-funded to covered-by-insurance. For more context on why this is happening, I recommend the Death Panel podcast’s latest episode, “Scenes from the Class Struggle at CVS.”
If you’re a reporter who would like to connect with one of the COVID-19 Data Dispatch readers who shared a story, please email me at betsy@coviddatadispatch.com. Most of the people in the database below shared an email or other contact info.
[table id=10 responsive=collapse responsive_breakpoint=all /] -
New COVID-19 vaccines are now available: 10 key facts and statistics about these shots

Data from a CDC presentation suggest that people of all ages, including children, receive a benefit from updated COVID-19 vaccines. We now have two new COVID-19 vaccines available for this year’s respiratory virus season, one from Pfizer and one from Moderna, which are expected to perform well against current variants. The FDA approved both vaccines this week, and the CDC recommended them for almost all Americans. A third option, from Novavax, may become available in the coming weeks as well.
The federal government aims to present this fall’s shots as the next iteration in routine, annual COVID-19 vaccines—similar to the routine we’re all used to for flu shots. In fact, I’ve seen some news suggesting that the federal health agencies don’t want us to call these shots “boosters,” instead calling them “updated” shots or annual shots.
But this fall’s vaccine rollout is likely to be anything but routine, as it’s the first rollout following the end of the federal COVID-19 public health emergencies. The government is no longer purchasing shots and distributing them for free; now, insurance companies will have to cover the shots.
As a result, many Americans—especially those without health insurance—will have a harder time accessing these vaccines than they have for previous shots. Plus, the federal emergency’s end will make it harder for us to track how the vaccines are performing, as the coronavirus continues to evolve into new variants.
With all of these complications in mind, here are ten key facts and statistics that you should know about this fall’s COVID-19 vaccines.
Pfizer and Moderna’s shots have been approved and recommended for all Americans, ages six months and older.
Despite some debates among scientists about whether younger people really need updated COVID-19 shots, the FDA has approved these vaccines—and the CDC has recommended them— for all age groups. This is important because CDC recommendations are often the basis for insurance coverage, as experts explained at a webinar hosted by the National Press Foundation on Tuesday.
The shots exclusively target XBB.1.5, a coronavirus lineage that is common in the U.S. and globally right now.
According to the CDC’s genomic surveillance program, almost all cases in the U.S. in recent weeks have been caused by XBB.1.5 or related variants from the XBB lineage. Variants like EG.5 and FL.1.5.1 are also XBB descendants, which have been given nicknames to make it a bit easier for scientists to keep track of them.
It’s also important to note that, unlike last year’s boosters, this fall’s shots are monovalent vaccines—meaning they only target XBB.1.5. The shots no longer target the original strain of SARS-CoV-2 that first circulated in 2020. Scientists generally approve of this choice, as the virus has mutated so much since that time.
Moderna’s booster led to a 17-fold increase in antibodies against XBB.1.5 and XBB.1.6.
The vaccine companies presented data to the CDC’s vaccine advisory committee on Tuesday. Moderna’s presentation included results from a study testing its new vaccine against several different variants, using blood samples from people who received the booster.
About one month after vaccination with Moderna’s booster, the participants had about 17.5 times more neutralizing antibodies against XBB.1.5, 16.7 times more against XBB.1.6, 14 times more against EG.5.1, and 10 times more against BA.2.86. Pfizer also presented data, suggesting that their vaccine should similarly perform well against current variants.
The new vaccines should lead to similar side effects as we’re used to from past mRNA shots.
Based on data that the vaccine companies presented to the CDC’s committee, this fall’s Pfizer and Moderna vaccines should lead to similar side effects—headache, fatigue, muscle pain, etc.—as many of us have expected from past rounds of COVID-19 shots. The companies, along with the CDC and FDA, will continue to monitor these vaccines for any safety issues that may emerge as people start to get them.
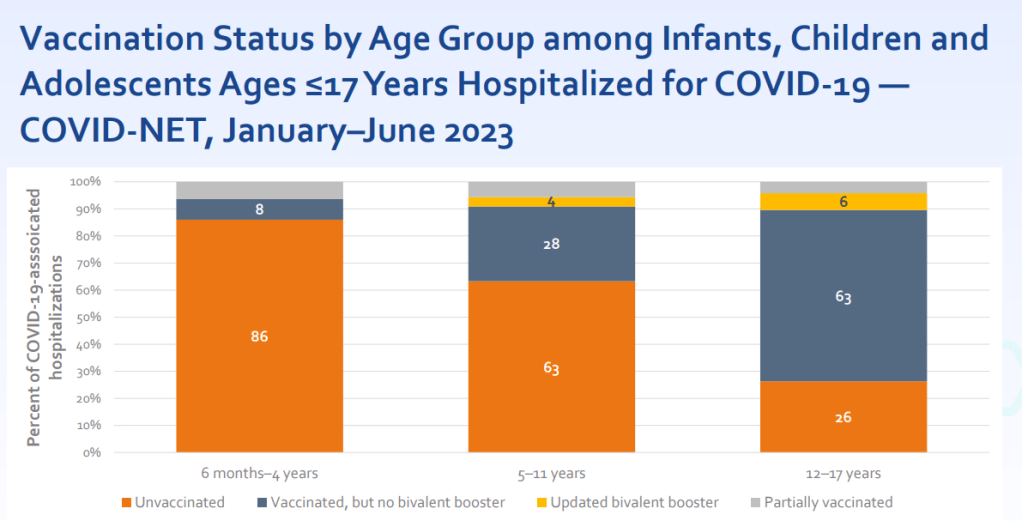
Young, unvaccinated children are at higher risk for COVID-19.
One of the CDC presentations focused on how this fall’s vaccines may benefit young children. Last fall and winter, hospitalization rates were higher for COVID-19 than for the seasonal flu across all young age groups, from infants (under six months) to 12-17 years old. The vast majority of the children hospialized were not vaccinated or hadn’t received last year’s booster.
For some CDC advisory committee members, these data were convincing in suggesting that this fall’s vaccine should be recommended for children, experts told STAT News. Vaccines updated to match current variants have a clear benefit for all age groups.
Long COVID remains a significant risk for Americans across age groups.
Another CDC presentation discussed Long COVID, as one of the potential adverse outcomes of a COVID-19 case. The CDC shared new data from a national survey conducted in 2022, which suggests that 9% of Americans ages 35 to 49 have experienced Long COVID symptoms (defined as symptoms lasting at least three months after a COVID-19 case). Adults ages 50-64 and 18-34 also reported high levels of Long COVID, at 7.4% and 6.8% ever experiencing symptoms, respectively.
Many studies have shown that vaccination lowers risk of Long COVID, though it does not by any means eliminate this risk. While it’s good to see the CDC incorporating Long COVID into its vaccine risk/benefit discussions, much more research is needed to better understand how to prevent this debilitating condition.
A Novavax vaccine is still in the pipeline.
Novavax also presented data to the CDC’s advisors this week, suggesting that its vaccine (also based on XBB.1.5) should perform similarly to the Pfizer and Moderna options. But unlike the Pfizer and Moderna vaccines, Novavax’s has yet to receive FDA approval. The company has said it’s still planning to distribute its vaccine this fall, but it’s unclear when the FDA may authorize it.
Some people are eager to receive the Novavax vaccine this fall, rather than Pfizer or Moderna’s, because this vaccine uses a different mechanism to boost the immune system. It may also lead to fewer side effects than the mRNA vaccine, making it a potentially good option for people who’ve had particularly strong reactions. (I know a couple of readers have sent me questions about this, and aim to do a deep-dive on Novavax in a future issue.)
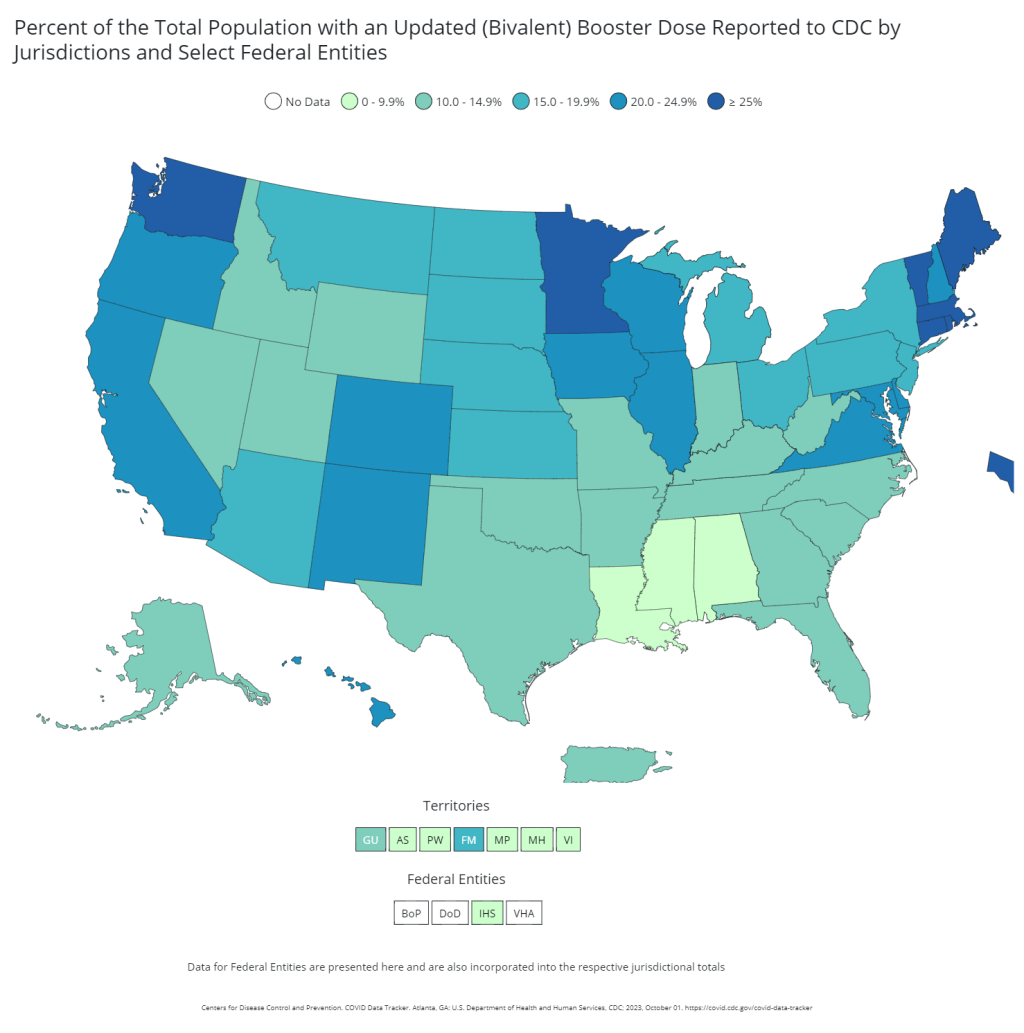
Only 17% of Americans received last fall’s bivalent booster.
The booster uptake last year was low, according to the CDC. Even among seniors, only 43% received the booster. Can we do better this year?
A POLITICO/Morning Consult poll found that about 60% of respondents said they “probably or definitely” would get this year’s vaccine. (The poll included about 2,000 registered voters from across the U.S.) But it’s likely that access issues could get in the way for many people, as getting this COVID-19 vaccine will be much more challenging than it’s been in past rollouts.
HHS program should provide free vaccines for 25-30 million adults.
The Department of Health and Human Services has officially launched its “Bridge to Access” program, designed to provide free COVID-19 shots to uninsured Americans. Through this program, the HHS is essentially buying a small number of shots and distributing them to pharmacies, federally supported health centers, and other providers. You should be able to view these providers at vaccines.gov, according to the HHS. But I’ll be curious to see how well that actually works.
This year’s vaccine rollout will be much harder to track.
In the past, I’ve written about how the U.S. has failed to monitor breakthrough cases, or COVID-19 infections that occur after someone is vaccinated (and the hospitalizations, deaths, and long-term symptoms that may result). This year, not only are we failing to track breakthrough cases—the U.S. no longer has any national case data at all. We also no longer have vaccination data, as the CDC is not collecting this information from state and local health systems.
So, how will we know how this year’s vaccine rollout goes? It’ll likely be a lot of guesswork, extrapolating from a few state/local health departments, polling data, and other smaller-scale research to estimate how many people are getting vaccinated nationally. This challenge is just another example of the damage that the federal government has done in the last year by dismantling many of its COVID-19 data systems.
-
Sources and updates, August 20
- New toolkit for estimating COVID-19 risk from wastewater: Researchers at Mathematica published a new, open-source toolkit for interpreting wastewater data. It includes an algorithm that scientists and health officials can use to identify when a new surge might be starting based on wastewater results, as well as a risk estimator tool that combines wastewater data with healthcare metrics. The researchers developed this toolkit using data from North Carolina during the Delta and Omicron surges; their paper in PNAS last month describes it further, as does a blog post by the Rockefeller Foundation (which funded the project). This tool doesn’t provide real-time updates, as it only includes wastewater data through December 2022, but it offers a helpful model for using this source to inform public health policies.
- Vaccine delays for uninsured Americans: The CDC estimates that new COVID-19 boosters will become available in late September or early October, as I wrote last week. But Americans without health insurance may have to wait longer to get the shots or pay a hefty price tag, according to recent reporting from POLITICO. A federal government program with national pharmacy chains, which will provide the shots for free to uninsured people, is not slated to start until mid-October. Instead, uninsured people will need to pay out-of-pocket or find one of a small number of federal health centers to get vaccinated; this is likely to discourage vaccinations, POLITICO reports. And the number of uninsured people is only growing thanks to Medicaid redeterminations.
- Budget cuts at the CDC could mean layoffs: A recent op-ed in STAT News, written by two researchers familiar with the CDC’s organizational structure, warns that budget cuts at the agency could lead to a significant reduction in public health workers. The CDC’s budget was cut as part of the federal government’s debt ceiling negotiations last month, the authors explain. It faces a cut of about 10%, or $1.5 million a year, which could lead to significant layoffs. The reduced jobs are particularly likely to impact staff at the state and local levels, the op-ed’s authors argue, rather than at the CDC’d headquarters in Atlanta. “Reductions there will cut public health services and will have their greatest impact on the most vulnerable populations,” they write.
- Vaccine effectiveness for young children: Speaking of the CDC: the agency published a study this week in its Morbidity and Mortality Weekly Report describing COVID-19 vaccine effectiveness for the youngest children who are eligible (i.e. under five years old). Researchers at the CDC and partners at healthcare centers across the country tracked COVID-related emergency department and urgent care visits among young children, from July 2022 through July 2023. Effectiveness for the primary series was low: Moderna’s two-dose series scored just 29% effective at preventing ED and urgent care visits, while Pfizer’s three-dose series was 43% effective. Children who received a bivalent (Omicron-specific) follow-up dose were much more protected, however: this regimen was 80% effective. Bivalent boosers should be a priority for young kids along with adults, the study suggests.
- Immune system changes following COVID-19: Another notable study from this week, from scientists at Weill Cornell Medicine and other institutions, describes how severe COVID-19 cases may damage patients’ immune systems. The researchers analyzed how specific genes were expressed in immune system cells taken from people who had severe cases of COVID-19. They found expression changes as long as a year after patients’ initial infections, and connected those changes to inflammation, organ damage, and other long-term issues. These genetic changes may point to one cause for Long COVID symptoms, though the study is somewhat limited by its focus on patients who had severe symptoms early on (as most people with Long COVID have initially milder cases).
- Smell and taste loss following COVID-19: While smell loss has long been considered a classic COVID-19 symptom, a new study shows that taste loss is also common, even among people who don’t lose their sense of smell. Researchers at the Monell Chemical Senses Center (a nonprofit center in Philadelphia) studied these symptoms through an online survey, which included about 10,000 participants between June 2020 and March 2021. COVID-positive participants were more likely to report smell issues, taste issues, and both together, compared to people who didn’t get sick, the researchers found. Their survey methodology—which included asking people to self-assess their senses by smelling common household objects—could be used for further large-scale studies of these symptoms, the researchers write.
-
Sources and updates, May 21
- New funding from CDC’s forecasting center: The CDC’s Center for Forecasting and Analytics (CFA) announced a new funding opportunity for state and local health agencies to develop new disease modeling tools. CFA is a relatively new center itself; it launched last year with the goal of modernizing the U.S.’s disease forecasting capacities (see my FiveThirtyEight article about the center for more details). This funding opportunity will, I expect, enable the CFA’s growing staff to work directly with health agencies on advancing analytical methods. I look forward to seeing the results of those projects.
- Experts argue to keep masks in healthcare: A new commentary article, published this week in the Annals of Internal Medicine, argues in favor of keeping mask requirements in healthcare settings. The experts (from the National Institutes of Health and George Washington University) point to real-world experience, suggesting transmission between patients and healthcare workers is less likely when everyone is wearing a mask, preferably one of high quality. This article coincides with an advocacy campaign to keep masks in healthcare, including virtual and in-person actions across the U.S.
- CDC releases provisional drug overdose data for 2022: The CDC’s National Center for Health Statistics has released overdose data for 2022, reporting that nearly 110,000 Americans died of overdoses for the second year in a row. Overdoses have leveled off from 2021, but the 2022 data still represent a sharp increase from pre-pandemic trends. Some states in the South and West Coast (such as Texas, Oklahoma, Wyoming, Washington) saw the sharpest increases from 2021 to 2022, according to the CDC. These data are all preliminary and will be updated later in the year.
- Pediatric COVID-19 boosters could save school days: A new modeling study, published this week in JAMA Network Open, suggests that the U.S. could have seen about 10,000 fewer kids hospitalized with COVID-19 and 5.5 million fewer school days lost during the 2022-2023 respiratory virus season, if kids received booster shots in large numbers. The researchers arrived at these estimates through a model that simulated COVID-19 booster vaccination rates at similar levels to annual flu vaccination in kids. Future booster campaigns should focus on children in addition to older adults, the authors argue.
- RSV vaccine for infants moves ahead: Speaking of pediatric vaccinations: the FDA’s vaccine advisory committee met last week to discuss a new vaccine candidate from Pfizer, which would protect infants from RSV. Unlike most pediatric vaccines, this shot would be delivered to pregnant parents in order to protect their babies at birth. While the FDA’s advisors endorsed the vaccine for its effectiveness, some committee members expressed concerns over safety. Helen Branswell at STAT has more details.
-
Sources and updates, April 23
- External review of the CDC: The People’s CDC, a group of public health experts, scientists, and educators dedicated to advocating for increased COVID-19 precautions, released a new report reviewing the federal CDC’s actins during the pandemic. The report incorporates feedback from a survey of almost 500 experts and from over 200 reports. Overall, the People’s CDC “found that the CDC has prioritized individual choice and short-term business interests over sharing accurate scientific evidence with the public and protecting population health.” (Disclaimer: I was one of the experts surveyed for this report!)
- Use of COVIDTests.gov: This new paper, published in the CDC’s Morbidity and Mortality Weekly Report (MMWR), reports on how Americans used COVIDTests.gov, the USPS/HHS effort to distribute free at-home tests. Since the site’s launch in January 2022, about one in three U.S. households received a test kit from this program, the research team found. They also found that this program may have helped improve equity in COVID-19 test access, as Black and white Americans utilized the free tests at similar rates. Of course, the program has been discontinued as of this spring.
- Impact of racial discrimination on vaccination: Speaking of health equity: another report published in MMWR this week shares a correlation between discrimination and vaccination status. Researchers at the CDC and their collaborators analyzed data from the CDC’s National Immunization Survey, including about 1.2 million survey results from April 2021 through November 2022. Among the respondents, people who reported experiencing racial or ethnic discrimination in a healthcare setting were less likely to be vaccinated for COVID-19. The findings confirm many health experts’ equity concerns from early in the vaccine rollout.
- Declining childhood vaccinations worldwide: Vaccine equity is a concern on the global scale, too. A new report from UNICEF shows that 67 million children worldwide missed at least one vaccination between 2019 and 2021, as healthcare systems were strained. The report also presents new data on global confidence in childhood vaccines: in some countries, this confidence has dropped by up to 44 percentage points. Vaccine confidence only improved in three countries (China, India, and Mexico). “The threat of vaccine hesitancy may be growing,” UNICEF warns.
- Healthcare workers present while sick: One more paper that caught my attention this week: researchers at the Veterans Affairs healthcare system in Boston tracked a cohort of about 4,000 healthcare workers between December 2020 and September 2021. In addition to PCR testing, the workers conducted daily COVID-19 symptom reviews, and received guidance to stay home or leave work if they didn’t feel well. But the researchers found that many workers didn’t actually stay home: among 255 workers who had symptomatic COVID-19 during the study period, almost half reported that they were present, at work, at the time they received a positive test result. The paper indicates why it’s important to keep masks in healthcare settings, even when community cases are lower.
-
Sources and updates, February 12
- CDC committee recommends adding COVID-19 to childhood vaccine schedule: The CDC’s Advisory Committee on Immunization Practices (ACIP), which makes guidance on vaccination policies, issued a report this week recommending that COVID-19 vaccines be added to the standard childhood immunization regimen. Under the new guidelines, most children ages six months and older should receive two doses of a Moderna or Pfizer vaccine, followed by a bivalent/Omicron-specific booster shot. Immunocompromised children are eligible for additional doses.
- KFF’s latest COVID-19 Vaccine Monitor focuses on winter surge: The Kaiser Family Foundation recently released the January 2023 update of its Vaccine Monitor project, which tracks U.S. sentiment around COVID-19 vaccines (and other pandemic topics) over time. In the latest round of surveys, KFF researchers found that about 38% of U.S. adults reported that “their households experienced either COVID-19, the flu, or RSV over the past month or so.” About 46% of adults reported that the news of these viruses made them more likely to take safety precautions. The report also includes data on bivalent booster shot uptake, behavior among immunocompromised people, and more.
- New variants have yet to emerge from China, study suggests: A new paper from researchers at the Beijing Center for Disease Prevention and Control, published in The Lancet this week, found that COVID-19 cases in China during November and December 2022 were primarily driven by the Omicron subvariants BA.5.2 and BF.7. Both of these lineages entered China from other countries, rather than evolving during the country’s surge following the end of its “zero COVID” policies. The new paper is good news for global health experts who’ve been worried about new variants emerging from China, though outside reviewers have cautioned that it’s only one small snapshot of cases in the country, according to reporting by POLITICO EU.
- Wastewater surveillance has a global health equity problem: Another study that caught my attention this week was a paper from the COVIDPoops19 team at the University of California Merced, summarizing findings from their global wastewater dashboard. The team reviewed wastewater surveillance projects at over 200 universities, 1,400 sites, and 55 countries, and found that monitoring primarily occurred in high-income countries. The researchers also examined open access to data, finding that high-income countries were better at sharing information with researchers and with the public. For wastewater-based epidemiology to reach its full potential, “show us the data,” the team writes in their paper’s abstract.
- Microbiome research shows promise for understanding ME/CFS: In one more piece of research news: two recent studies suggest that the gut microbiome could play a role in causing myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), a debilitating chronic disease that often occurs after viral infection. In research projects funded by the National Institutes of Health, scientists found specific changes to gut bacteria that were associated with ME/CFS patients. These changes could potentially be used as biomarkers to diagnose ME/CFS and as starting points for treatment. The new research also has potential implications for Long COVID, as many Long COVID patients meet the diagnostic criteria for ME/CFS.
-
Sources and updates, January 8
- NIH launches at-home testing telehealth program: This week, the National Institutes of Health announced the first location for “Home Test to Treat,” a new program that will make it easier for people in vulnerable communities to receive Paxlovid after testing positive on at-home, rapid tests. The Biden administration first announced this program in September, but it’s formally launching now with Berks County, Pennsylvania as the first participating community. As Paxlovid shifts to a drug that must be privately purchased instead of provided for free by the federal government, more programs like this one will be needed to fill access gaps.
- Study estimates global Long COVID prevalence: A large team of researchers, led by population health scientists at the University of Washington, conducted an extensive review of Long COVID symptoms. The analysis used 54 prior studies and two medical record databases, incorporating data from 1.2 million people in total. Overall, about 6% of patients reported at least one class of Long COVID symptoms three months after their initial infections, with the vast majority of cases occurring in people who had mild acute cases. The study was published in JAMA in October, but gained attention this week thanks to an article that its leading authors wrote in The Conversation.
- China’s COVID-19 data are unreliable: It’s been about a month since China loosened its COVID-19 protocols in the wake of protests and contagious Omicron subvariants, and the country is now facing a massive surge—with as many as one million new cases a day according to some modeling estimates. Yet COVID-19 deaths reported in the country have been very low, fewer than five a day. This discrepancy suggests that China’s authorities are not correctly counting their COVID-19 deaths, while the country’s dismantled testing infrastructure has also led to less reliable case numbers. Officials from the World Health Organization have formally called on the country to “be more forthcoming with information” about its COVID-19 surge, reports Helen Branswell at STAT News.
- CDC testing airplane wastewater on flights from China: In response to surveillance concerns, the CDC is working to test wastewater on flights arriving from China in select U.S. airports. This method is, of course, more efficient than testing every single traveler from the country in the interest of identifying any new variants that might arise. (Though it’s worth noting that some experts are skeptical about the potential of new variants arising in China.) Scientists from Concentric, a company that works with the CDC on traveler surveillance, previously talked about plane wastewater testing during our interview in November.
- Race/ethnicity differences among child vaccination rates: Finally, a notable study in this week’s CDC Morbidity and Mortality Weekly Report: researchers at the CDC and collaborators examined vaccination rates among children ages five to 17 using data from the National Immunization Survey. They found vaccination coverage (with at least one dose) was highest among Asian children (at about 75%), followed by Hispanic or Latino children (49%), white children (45%), and Black children (43%). The researchers also noted differences among vaccination rates by other socioeconomic factors, and by parents’ mask-wearing habits.
-
Sources and updates, December 11
- 2022 America’s Health Rankings released: This week, the United Health Foundation released its 2022 edition of America’s Health Rankings, a comprehensive report providing data for more than 80 different health metrics at national and state levels. The 2022 report includes new metrics tailored to show COVID-related disparities; for example, Black and Hispanic Americans had higher rates of losing friends and family members to COVID-19 compared to other groups. I’ve used data from past iterations of this report in stories before, and I’m looking forward to digging into the 2022 edition.
- FDA authorizes bivalent boosters for young kids: This week, the FDA revised the emergency use authorizations (EUAs) of both Pfizer’s and Moderna’s updated, Omicron-specific booster shots to include children between six months and five years old. Kids who previously got two shots of Moderna’s vaccine for this age group can receive a bivalent booster two months later, while kids who got two shots of Pfizer’s vaccine can receive a bivalent booster as their third dose. (Remember, Pfizer’s vaccine for this age group includes three doses.) The updated EUAs will help protect young children from Omicron infection, though uptake will likely be low.
- CDC updates breakthrough case data: Speaking of the updated boosters: the CDC recently added data on these shots to its analysis of COVID-19 cases and deaths by vaccination status. In September, people who had received a bivalent, Omicron-specific boosters had a 15 times lower risk of dying from COVID-19 compared to unvaccinated people; and in October, bivalent-boosted people had a three times lower risk of testing positive compared to the unvaccinated. The CDC will update these data on a monthly basis.
- Director Walensky discusses authority challenges: One bit of coverage from the Milken Future of Health Summit that caught my attention: CDC Director Dr. Rochelle Walensky talked about the agency’s limitations in collecting data from states, reports Rachel Cohrs at STAT News. Walensky specifically highlighted the challenges that the CDC might face in collecting data when the public health emergency for COVID-19 ends, something I’ve previously covered in this publication.
- Boston establishes neighborhood-level wastewater testing: Finally, one bit of wastewater surveillance news: the city of Boston is setting up 11 new sites to test wastewater, giving local public health officials more granular information about how COVID-19 is spreading in the region. The new initiative is a partnership with Biobot Analytics, the same wastewater testing company that has long worked with Boston, the CDC, and public health institutions across the country. (Boston was one of the first cities to start doing this testing.) Also, speaking of Biobot: the company just added a nice chart of coronavirus variants in U.S. wastewater over time to its dashboard.
-
Sources and updates, July 31
- KFF poll shows low vaccine uptake for young kids: This week, the Kaiser Family Foundation released an update from their COVID-19 Vaccine Monitor, an ongoing project tracking U.S. attitudes towards vaccines. This latest update focuses on children under age five, and the results are worrying: about 43% of parents with kids in this age group say they will “definitely not” get their child vaccinated, citing concerns about vaccine safety. Conservative parents and those who are unvaccinated themselves were particularly likely to be against vaccinating their young kids, KFF found.
- Vaccine side effects less common for second boosters: A new CDC study, published in this week’s Morbidity and Mortality Weekly Report, tracked reactions to COVID-19 boosters among Americans over age 50 using CDC monitoring systems. Among over 200,000 people who received third and fourth doses from the same vaccine manufacturer, side effects like a sore arm and fatigue were less common after the fourth dose compared to the third dose. Still, uptake for second boosters has been slow and potentially inequitable; the CDC recently published data on second boosters by race/ethnicity, showing that white Americans over age 50 are more likely to get this extra protection than non-white people in this age group.
- White House summit on next-generation COVID-19 vaccines: And one more piece of vaccine news for this week: the White House brought together federal officials, scientists, and pharmaceutical executives for a summit discussing next-generation COVID-19 vaccines. The summit highlighted vaccine candidates designed to work against many potential coronavirus variants, as well as those that would be delivered through the nose—potentially producing more protection against coronavirus infection and transmission. Either option would require a lot of funding from a Congress that has been hesitant to support COVID-19 efforts.
- States are letting health emergency declarations expire: While the federal declaration of COVID-19 as a public health emergency will remain in place at least through this fall, many states have let their declarations expire in recent months. These expirations impact the resources states are able to allocate for tracking and responding to COVID-19—ranging from data collection to telehealth access. The ending emergencies are certainly contributing to less frequent COVID-19 data updates in many states.
- New studies on COVID-19’s origins: Two major studies have conclusively linked the coronavirus’ early spread to the Huanan Seafood Market in Wuhan, China. These studies, both published in Science, were produced by an international group of virologists and evolutionary biologists at the Scripps Research Institute, the University of Arizona, the University of Sydney, the University of Edinburgh, and many other institutions. The experts traced early cases in the seafood market, finding evidence of spillover from animals to humans. The precise origins of COVID-19 are still unknown, but these studies go a long way in demonstrating early spread tied to animals, not a lab leak.