- Vaccination disparities in long-term care facilities: A new study in the CDC’s Morbidity and Mortality Weekly Report shares vaccination patterns from about 1,800 nursing homes, assisted living facilities, and other long-term care facilities across the U.S., focusing on the bivalent booster (or, last fall’s vaccine). The CDC researchers found significant disparities in these vaccinations: vaccine coverage was lowest among Black and Hispanic residents compared to other demographics, and was lowest in the South and Southeast compared to other regions. Future vaccination campaigns need to make it easy for these groups to get their shots, the authors suggest; but based on how the 2023 rollout has gone so far, this trend seems likely to continue.
- Reasons for poor bivalent booster uptake: Speaking of last fall’s boosters, a study from researchers at the University of Arizona suggests reasons why people didn’t get the shots last year. Researchers surveyed about 2,200 Arizona residents who had received at least one COVID-19 vaccine dose. Among the survey respondents who didn’t get last year’s booster, the most common reason for not doing so was a belief that a prior infection made the shot unnecessary (40%), concerns about vaccine side effects (32%), believing the booster wouldn’t provide additional protection over prior shots (29%), and safety concerns (23%). As with the study above, this paper shows weaknesses in the U.S.’s recent vaccine promotion strategies.
- At-home tests are useful but far from perfect: Researchers at Nagoya University and the University of Oxford used mathematical models to study how different safety measures impact chances of COVID-19 outbreaks. The researchers developed models based on contact tracing data reflecting how Omicron spreads through groups. Rapid, at-home, antigen tests are a useful but imperfect method for reducing outbreak risk, the study found, with daily testing reducing the risk of a school or workplace outbreak by 45% compared to a scenario in which new cases are identified by symptoms only. “In high-contact settings, or when a new variant emerges, mitigations other than antigen tests will be necessary,” one of the scientists said in a statement.
- Long-term symptoms from non-COVID infections: The prevalence of Long COVID has led many scientists to develop new interest in chronic conditions that may arise after other common infections, such as the flu and other respiratory viruses. One recent study from Queen Mary University of London identifies a potential pattern, using data from COVIDENCE UK, a long-term study tracking about 20,000 people through monthly surveys. Researchers compared symptoms between people who had a COVID-19 diagnosis and those with other respiratory infections, looking at the month following infection. They found similar risks of health issues in the one-month timeframe for both groups, though specific symptoms (loss of taste and smell, dizziness) were more specific to Long COVID. Of course, some people in the “non-COVID” group could have had COVID-19 without a positive test; still, the data indicate more, longer-term research is needed.
- Autoimmune disorders following COVID-19: In another Long COVID-related paper, researchers at Yonsei University and St. Vincent’s Hospital in South Korea found that patients had increased risks of autoimmune and autoinflammatory disorders following COVID-19 cases. The study used patient records from South Korea’s national public health system, comparing about 354,000 people who had COVID-19 diagnoses to 6.1 million controls. COVID-19 patients had a significant risk of new autoimmune issues within several months after infection; new diagnoses included alopecia (or hair loss), Crohn’s disease (inflammatory bowel issues), sarcoidosis (overactive immune system), and more. These conditions should be considered by doctors evaluating potential Long COVID patients, the researchers wrote in their paper.
- New climate vulnerability index: This last item isn’t directly COVID-19 related, but may be useful in evaluating community risks for public health threats. The Environmental Defense Fund, Texas A&M University, and other partners have launched the U.S. Climate Vulnerability Index, a database providing Census tract-level information about how our changing climate will impact different communities. Communities are ranked from low to high climate vulnerability, with detailed data available on sociodemographic characteristics as well as potential extreme weather events and health trends.
Tag: vaccine equity
-
Sources and updates, October 8
-
COVID-19 vaccine issues: Stories from COVID-19 Data Dispatch readers across the U.S.

Last year, just 17% of the U.S. population received a bivalent booster. Will this year’s uptake be better? Last week, I asked you, COVID-19 Data Dispatch readers, to send me your stories of challenges you experienced when trying to get this fall’s COVID-19 vaccines. I received 35 responses from readers across the country, demonstrating issues with insurance coverage, pharmacy logistics, and more.
I’ve published the full responses in the table below. Here are a few common themes that I saw in these stories:
- Pharmacies aren’t receiving enough vaccines. Several readers shared that their pharmacies had inadequate vaccine supply to accommodate all the people who made vaccination appointments, or who wanted appointments. Vaccine supply may also be unpredictable—a pharmacy may think they’re getting more shots, but in fact not receive them—leading to appointment cancellations.
- Insurance providers weren’t prepared for this vaccine rollout. Despite months of advance notice that a fall COVID-19 vaccine was coming, many insurance companies apparently failed to prepare billing codes or other system updates that would allow them to cover the shots. A couple of people who shared insurance issue stories are on Medicare—representing a population (i.e. seniors) who should be at the front of the vaccine line.
- Very limited, confusing vaccine availability for young kids. Several readers shared that they were able to get vaccinated, but their children under 12 have not received a vaccine yet. While the FDA and CDC have authorized this fall’s COVID-19 vaccines for all Americans ages six months and older, younger children require a different vaccine formulation from adults. And this formulation appears either entirely unavailable or very difficult to access, depending on where you live.
- People living in less dense areas may need to travel. A few readers shared that, as they searched for vaccine appointments in their areas, the closest pharmacies with doses available were miles away—over 10 miles, in one case. This is a significant barrier for people fitting vaccine appointments into their work schedules.
- Information may be inconsistent. Vaccine availability listed in one place (such as a pharmacy chain’s website or the federal vaccines.gov website) may be inaccurate in another. Some readers shared that they spent extra time on the phone with pharmacies or health providers to get accurate information—another barrier.
- Pharmacies don’t have enough staff for this. Even readers who were able to receive COVID-19 vaccines often had to wait a long time at their pharmacies. Several shared that their pharmacies appeared to be understaffed, dealing with the COVID-19 shots along with routine prescriptions and other duties. The days of mass vaccination sites, efficiently run by public health departments, are long over.
- Kaiser Permanente members face delays. One company that appears to be causing outsized problems is Kaiser Permanente, one of the biggest insurers and health providers on the West Coast. Several readers shared that Kaiser was not providing new COVID-19 vaccines until early October, and would not cover the shots if their members went to another location. That’s a big delay, and it may be further impacted by a coming strike at the company.
- These vaccines are expensive. If you decide to pay for a COVID-19 shot out-of-pocket (as some readers did), it costs almost $200. Even the federal government is paying about triple the cost of last year’s COVID-19 vaccines per shot, for the doses it is covering, STAT News reports. The U.S. may have received a “bad deal” here, STAT suggests, considering all of the federal funding that’s supported vaccine research and development.
As I wrote last week, some news outlets have covered these challenges, but this issue really deserves more attention. The updated COVID-19 vaccines are basically the U.S. government’s only strategy to curb a surge this winter, and they should be easily, universally accessible. Instead, many people eager to get vaccinated are going through multiple rounds of appointments, phone calls, pharmacy lines, and more.
For every one of these readers who has persisted in getting their shot, there are likely many other people who tried once and then gave up. And those people who don’t receive the vaccine will be at higher risk of severe illness, death, and long-term symptoms from COVID-19 this fall and winter. This is a public health failure, plain and simple.
And it’s important to emphasize that this failure is not surprising. Many health commentators predicted that these challenges would arise as the federal public health emergency ended and COVID-19 tools transitioned from government-funded to covered-by-insurance. For more context on why this is happening, I recommend the Death Panel podcast’s latest episode, “Scenes from the Class Struggle at CVS.”
If you’re a reporter who would like to connect with one of the COVID-19 Data Dispatch readers who shared a story, please email me at betsy@coviddatadispatch.com. Most of the people in the database below shared an email or other contact info.
[table id=10 responsive=collapse responsive_breakpoint=all /] -
Ending emergencies will lead to renewed health equity issues

The header image from a story I recently had published in Amsterdam News about declining access to COVID-19 services. Last week, I gave you an overview of the changes coming with the end of the federal public health emergency (PHE), highlighting some shifts in publicly available COVID-19 services and data. This week, I’d like to focus on the health equity implications of the PHE’s end.
COVID-19 led the U.S. healthcare system to do something unprecedented: make key health services freely available to all Americans. Of course, this only applied to a few specific COVID-related items—vaccines, tests, Paxlovid—and people still had to jump through a lot of hoops to get them. But it’s still a big deal, compared to how fractured our healthcare is for everything else.
The PHE allowed the U.S. to make those COVID-19 services free by giving the federal government authority to buy them in bulk. The federal government also provided funding to help get those vaccines, tests, and treatments to people, through programs like mass vaccination sites and mobile Paxlovid delivery. Through these programs, healthcare and public health workers got the resources to be creative about breaking down access barriers.
Now that the emergency is ending, those extra supplies and resources are going away. COVID-19 is going to be treated like any other disease. And as a result, people who are already vulnerable to other health issues will become more at risk for COVID-19.
I wrote about this health equity problem in a recent story for Amsterdam News, a local paper in New York City that serves the city’s Black community. The story talks about how COVID-19 services in NYC are changing with the end of the PHE, and who will be most impacted by those changes. It’s part of a larger series in the paper covering the PHE’s end.
Most of the story is NYC-specific, but I wanted to share a few paragraphs that I think will resonate more widely:
Jasmin Smith, a former contact tracer who lives in Brooklyn, worries that diminished public resources will contribute to increased COVID-19 spread and make it harder for people with existing health conditions to participate in common activities, like taking the subway or going to the grocery store.
COVID-19 safety measures “make the world more open to people like myself who are COVID-conscious and people who might be immunocomprmised, disabled, chronically ill,” Smith said. “When those things go away, your world becomes smaller and smaller.”
The ending federal public health emergency has also contributed to widespread confusion and anxiety about COVID-19 services, [said Dr. Wafaa El-Sadr, a professor of epidemiology and global health at Columbia University’s Mailman School of Public Health]. “People have so many questions about this transition,” she said, and local leaders could do more to answer these questions for New Yorkers.
The near future of COVID-19 care in the U.S. could reflect existing health disparities for other endemic diseases, like the seasonal flu and HIV/AIDS, [said Steven Thrasher, a professor at Northwestern University and author of the book, The Viral Underclass]. For example, people with insurance and a primary care physician are more likely to get their annual flu shots, he said, while those without are more likely to face severe outcomes from the disease.
After May 11, COVID-19 outcomes are likely to fall along similar lines. “More people have died of AIDS after there were HIV medications,” Thrasher said. “More people have died of COVID when there were vaccines in this country than before.”
For more news and commentary on COVID-19 emergencies ending, I recommend:
- Other stories in Amsterdam News’ The Long Emergency series
- Only the Global-Health Emergency Has Ended (The Atlantic)
- Does the end of Covid emergency declarations mean the pandemic is over? (STAT News)
- End of PHE: A shift in data (Your Local Epidemiologist)
- The Sociological Production of the End of the Pandemic (Death Panel)
-
Sources and updates, April 23
- External review of the CDC: The People’s CDC, a group of public health experts, scientists, and educators dedicated to advocating for increased COVID-19 precautions, released a new report reviewing the federal CDC’s actins during the pandemic. The report incorporates feedback from a survey of almost 500 experts and from over 200 reports. Overall, the People’s CDC “found that the CDC has prioritized individual choice and short-term business interests over sharing accurate scientific evidence with the public and protecting population health.” (Disclaimer: I was one of the experts surveyed for this report!)
- Use of COVIDTests.gov: This new paper, published in the CDC’s Morbidity and Mortality Weekly Report (MMWR), reports on how Americans used COVIDTests.gov, the USPS/HHS effort to distribute free at-home tests. Since the site’s launch in January 2022, about one in three U.S. households received a test kit from this program, the research team found. They also found that this program may have helped improve equity in COVID-19 test access, as Black and white Americans utilized the free tests at similar rates. Of course, the program has been discontinued as of this spring.
- Impact of racial discrimination on vaccination: Speaking of health equity: another report published in MMWR this week shares a correlation between discrimination and vaccination status. Researchers at the CDC and their collaborators analyzed data from the CDC’s National Immunization Survey, including about 1.2 million survey results from April 2021 through November 2022. Among the respondents, people who reported experiencing racial or ethnic discrimination in a healthcare setting were less likely to be vaccinated for COVID-19. The findings confirm many health experts’ equity concerns from early in the vaccine rollout.
- Declining childhood vaccinations worldwide: Vaccine equity is a concern on the global scale, too. A new report from UNICEF shows that 67 million children worldwide missed at least one vaccination between 2019 and 2021, as healthcare systems were strained. The report also presents new data on global confidence in childhood vaccines: in some countries, this confidence has dropped by up to 44 percentage points. Vaccine confidence only improved in three countries (China, India, and Mexico). “The threat of vaccine hesitancy may be growing,” UNICEF warns.
- Healthcare workers present while sick: One more paper that caught my attention this week: researchers at the Veterans Affairs healthcare system in Boston tracked a cohort of about 4,000 healthcare workers between December 2020 and September 2021. In addition to PCR testing, the workers conducted daily COVID-19 symptom reviews, and received guidance to stay home or leave work if they didn’t feel well. But the researchers found that many workers didn’t actually stay home: among 255 workers who had symptomatic COVID-19 during the study period, almost half reported that they were present, at work, at the time they received a positive test result. The paper indicates why it’s important to keep masks in healthcare settings, even when community cases are lower.
-
Sources and updates, December 4
- CDC awards $3 billion to improve public health infrastructure: The CDC announced this week that it has awarded state and local public health agencies a total of $3.2 billion to support hiring and training new workers, along with other infrastructure needs. The agency published a breakdown of all the agencies that received awards, although it has not included specific details on what funds will be used for in each place. Local reporters, if your health department received funding, this might be worth looking into!
- CDC expands wastewater testing for polio: Another notable CDC announcement this week: the agency is expanding its wastewater surveillance for polio to two new areas, Oakland County, Michigan and Philadelphia. Testing wastewater for polio is more complicated than testing it for the coronavirus, as STAT News’ Helen Branswell explains in this article; as a result, the CDC is expanding this surveillance in a more limited capacity than what it’s doing for other viruses, like monkeypox and the flu.
- Majority of COVID-19 deaths are now among vaccinated people: A new report from the Kaiser Family Foundation explains why more than 50% of COVID-19 deaths in the U.S. in recent months were among people who had received at least two vaccine doses. According to KFF, factors driving this trend include the rising share of Americans who are vaccinated, waning protection from initial doses, and low uptake of booster shots—particularly of the Omicron-specific boosters that provide better protection against newer variants. More reason to get the new booster if you haven’t yet!
- Paid sick leave correlates with higher vaccination rates: Speaking of vaccination: a new study from researchers at Drexel University and Boston University found that large U.S. cities with city-wide paid sick leave policies had higher vaccination rates than those without such policies. The correlation was particularly evident in neighborhoods with higher social vulnerability, the researchers found. Expanding paid sick leave could help reduce inequities in vaccination coverage, the paper’s authors recommend.
- No monoclonal antibody drugs are currently authorized in the U.S.: This week, the FDA announced that bebtelovimab, a monoclonal antibody made by Eli Lilly, is no longer authorized for COVID-19 treatments in the U.S. The drug was designed based on older versions of the Omicron variant and doesn’t perform well against BQ.1 and BQ.1.1, the sublineages that are currently causing the majority of new cases in the U.S. As a result, no monoclonal antibodies are currently authorized, though Paxlovid and other treatments are still available.
-
Sources and updates, November 6
- New data on Omicron boosters: This week, we got two major updates on the safety and effectiveness of the bivalent, Omicron-specific booster shots from Pfizer and Moderna. First, a study in the CDC’s Morbidity and Mortality Weekly Report examined safety, finding that side effects of the new boosters similar to the side effects of previous vaccines, according to the agency’s vaccine surveillance systems. For example, about 60% of vaccine recipients experienced pain, swelling, or itching in the arms where they received the shot. And second, Pfizer and BioNTech shared new data about the companies’ bivalent booster, suggesting that the new booster produces four times more neutralizing antibodies against BA.4 and BA.5 compared to the original booster shot. The study focused on older adults (over age 55) but is still helpful evidence that the new boosters are more effective against currently-circulating variants.
- NIH RECOVER is preparing its first clinical trial: RECOVER, the National Institutes of Health’s flagship study to understand and eventually treat Long COVID, announced this week that it’s preparing clinical trials to test potential treatments. The first of these trials was recently posted to ClinicalTrials.gov (a site for tracking studies that have received federal funding). This trial will focus on testing Paxlovid for Long COVID patients, and RECOVER anticipates it will begin enrolling patients in early 2023. Patients have previously expressed concerns that RECOVER is moving pretty slowly with trials, considering how many Americans are impacted by Long COVID.
- Patients Rising Now Congressional Scorecard: Speaking of government action on medical issues: Patients Rising Now, an advocacy organization focused on patients with chronic illnesses, recently published its first scorecard for Congressional representatives. The resource grades every Senator and House member in the 117th Congress based on how their voting record aligns with the organization’s priorities. While COVID-19 is not specifically mentioned in the grades, this scorecard could have implications for future pandemic-related votes.
- COVID-19 vaccination and race/ethnicity inequities: A new paper from researchers at the University of Minnesota and Boston University examined how vaccination impacted COVID-19 mortality patterns in Minnesota. During the Delta and Omicron surges, the researchers found, mortality among middle-aged people of color was higher than mortality among white people in an age group ten years older. The paper shows that COVID-19 remains “a pandemic of the disadvantaged,” author Elizabeth Wrigley-Field wrote on Twitter. (Disclaimer: through my work at MuckRock, I am collaborating with BU researcher Andrew Stokes, one of the paper’s coauthors.)
- RSV vaccine(s) could be coming soon: Finally, a bit of good news about another respiratory virus: two potential vaccines for RSV are likely to be under FDA review in the coming months. Pfizer recently reported promising results from a clinical trial of a vaccine for pregnant people, who pass antibodies to their children (thus reducing infant RSV risk). And U.S. pharmaceutical company GSK reported results from a trial testing its RSV vaccine for older adults.
-
Sources and updates, October 23
- Genomic surveillance from international travelers: A new CDC dashboard page provides data from the agency’s program sequencing COVID-19 test samples from people arriving in the U.S. on international flights, aiming to identify and track new variants. This program—a partnership between the agency, Ginkgo Bioworks, and XpresSpa Group—started during the Delta wave in 2021 with flights from India, but has since expanded to include over 1,000 volunteers a week at four major airports. The CDC’s new page reports test positivity for travelers’ samples and variants detected through sequencing.
- Implications of commercializing COVID-19 vaccines, treatments, tests: Researchers at the Kaiser Family Foundation analyzed how the federal government’s decreasing support for key COVID-19 products (vaccines, treatments, and tests) could impact Americans’ access. The government’s supply of these products has been depleted through 2022, and researchers anticipate the national Public Health Emergency will end in early 2023. As a result, Americans will soon likely need to rely on commercial products, leading to major challenges for low-income and uninsured people. (I wrote more about data implications of the PHE ending here.)
- Disparities in flu hospitalizations and vaccinations: Much COVID-19 coverage, including in this publication, has focused on inequitable vaccine uptake. In early 2021, more white Americans were getting vaccinated than minority groups, potentially contributing to higher rates of severe disease in those groups through the second year of the pandemic. A new CDC study in the agency’s Morbidity and Mortality Weekly Report (MMWR) finds that a similar trend has occurred for flu over the last ten years: Black, Hispanic, and Native Americans had lower flu vaccine coverage than white Americans from 2009-10 through 2021-22 seasons, and the same groups had higher flu hospitalization rates. The study suggests equitable vaccination is a problem that goes beyond the pandemic.
- Vaccine coverage among healthcare workers: Another CDC MMWR study that caught my attention this week provides results from a survey of healthcare workers, conducted in spring 2022. Among about 3,700 workers who responded to the survey, about four in five reported receiving a flu shot and two in three reported receiving a COVID-19 booster (during the 2021-22 flu season). Workers with vaccine mandates at their jobs had higher coverage than these averages, while long-term care workers had lower coverage. The results indicate more effort is needed to protect healthcare workers and their patients.
- HospitalFinances.org is revamped, newly available: In 2018, the Association of Health Care Journalists (AHCJ) first launched HospitalFinances.org, a database of financial information on nonprofit hospitals pulling from 990 tax forms. The site has been offline for the past year due to a hosting issue, but is now back thanks to researchers at the University of Missouri (which hosts AHCJ). While this resource isn’t specifically COVID-related, it could be useful to reporters investigating hospitals in their areas.
-
COVID-19 risk factors that should lead to Omicron booster priority

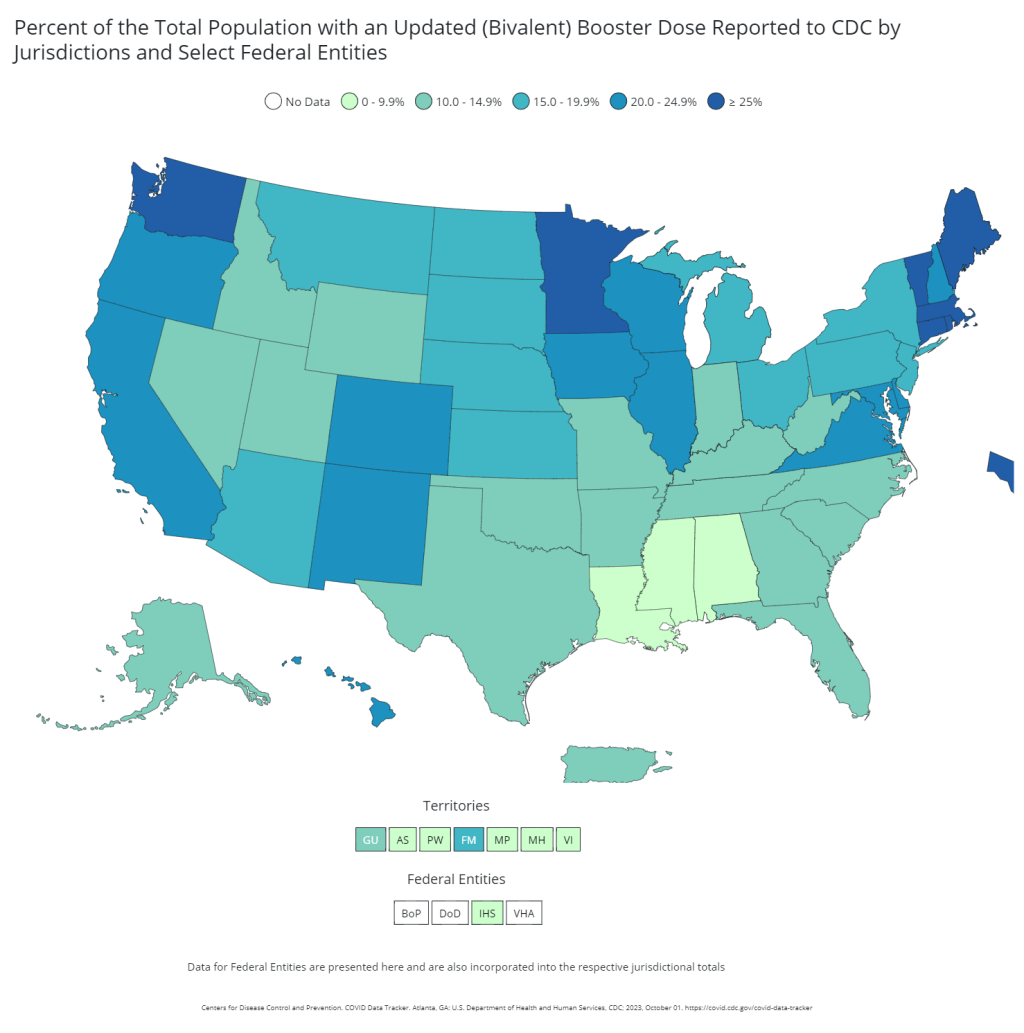
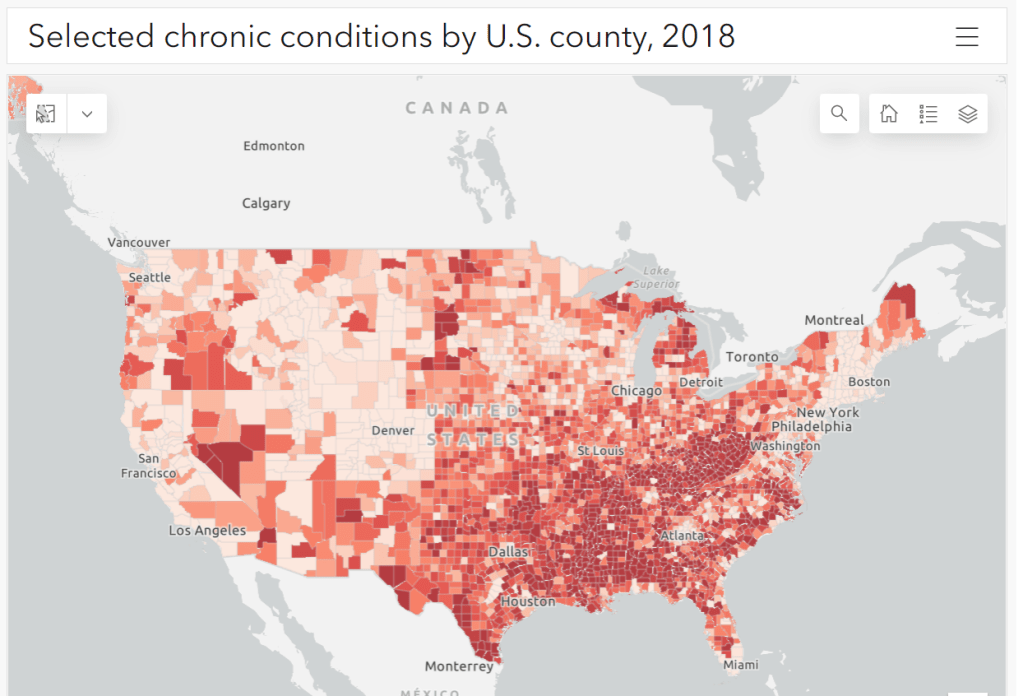
Parts of the South and Midwest have higher rates of chronic conditions (colored darker red on the map) that confer higher risk for severe COVID-19. Chart via the CDC. The U.S. has started a new booster shot campaign, this time using vaccines designed to specifically target super-contagious subvariants Omicron BA.4 and BA.5. (For more details on the shots themselves, see last week’s post.)
Unlike previous vaccination campaigns, these boosters are available to all adults across the country who have been previously inoculated. There was no prioritization for seniors, healthcare workers, or other higher-risk adults. The official guidance from the federal government is actually pretty straightforward, for once: everyone should get the new booster. And get a flu shot soon, too, possibly even at the same time as your COVID-19 shot.
But all previously-vaccinated Americans are not facing similar levels of COVID-19 risk. Many of the same qualifications that might have warranted you an earlier dose in spring 2021 should now lead you to prioritize your Omicron booster, even if you might have been infected recently. At the same time, people who fall in these groups (or who share their households) have a good reason to continue using other safety measures after their boosters.
Here are the major qualifications for higher risk, with data to back them up:
- Seniors, especially those over age 70: More than 90% of Americans over age 65 have received at least their primary vaccine series, according to the CDC, while over 70% have received at least one booster. Yet older Americans continue to have the highest rates of hospitalizations and deaths. For example, those older than 70 have consistently been hospitalized at several times the rate of younger adults (when adjusted for population). The same pattern is true for deaths among adults over age 75. Seniors who receive the new booster shots will face a lower risk of severe COVID-19 this fall and winter.
- Black, Indigenous, and other Americans of color, especially seniors: Despite dedicated vaccination campaigns and other health equity efforts, Americans of color have continued to be hit harder by the pandemic than white Americans. Higher rates of chronic conditions in minority populations combined with other socioeconomic factors (POC are more likely to work essential jobs, to lack healthcare, etc.) have led to disproportionately high hospitalization and death rates. And the U.S.’s booster shot campaigns so far have been inequitable, as shown in a recent study by demography experts. Reaching these populations should be a priority for the new Omicron boosters.
- Immunocompromised people: National estimates consider about 3% of Americans to be moderately or severely immunocompromised, meaning that their immune systems have limited capacity to respond to infections without medical assistance. This group includes cancer patients, organ transplant recipients, people with autoimmune diseases, and more. (This Yale Medicine article provides more information.) Immunocompromised people might have already had multiple booster shots but are still eligible to receive an Omicron booster as soon as possible, the CDC recommends.
- People with Long COVID and related conditions: While there isn’t as much established data in this area, I have seen a lot of anecdotal reports from Long COVID patients who work hard to avoid new coronavirus infections—concerned about reinfection’s possibility to worsen their symptoms. On the flip side, vaccination might lead to improvement in Long COVID patients, as the shot boosts a patient’s immune system in responding to lingering reservoirs of virus. The Atlantic covered this possibility when Long COVID patients were first eligible for vaccination in early 2021, and other studies since then have backed it up. More research is needed, but at the very least, Long COVID patients receiving a new booster will have lower risk of a new severe case.
- People with other preexisting health conditions: The CDC has an extensive list of medical conditions that can confer additional risk for severe COVID-19, with plenty of links to other CDC pages and medical sites where you can learn more about relevant evidence. I won’t go through them all here (that’s a topic for another week’s issue), but I do recommend checking out the CDC’s information and linked sources if you have a condition on the list. You can also explore this map of chronic condition rates by county.
More vaccination data
-
Sources and updates, July 10
- CDC adds (limited) Long COVID data to its dashboard: This week, the CDC’s COVID Data Tracker added a new page, reporting data from a study of “post-COVID conditions” (more colloquially known as Long COVID). The study, called Innovative Support for Patients with SARS-CoV-2 Infections (INSPIRE), follows patients who test positive for up to 18 months and tracks their continued symptoms. Among about 4,100 COVID-positive patients in the study, over 10% still had symptoms at three months after their infections, and over 1% still had symptoms at 12 months. This is just one study among many tracking Long COVID, but it is an important step for the CDC to add these data to their dashboard.
- Air change guidance by state: In recognition of the role ventilation can play in reducing COVID-19 spread, some states have put out recommendations for minimum air changes per hour (ACH), a metric for tracking indoor air quality. Researcher Devabhaktuni Srikrishna has compiled the recommendations on his website, Patient Knowhow, with a map showing ACH guidance by state. (I recently interviewed Srikrishna for an upcoming story about ventilation.)
- COVID-19 is a leading cause of death in the U.S.: A new study from researchers at the National Institutes of Health’s National Cancer Institute confirms that COVID-19 was the third-leading cause of death in the U.S., in both 2020 and 2021. The researchers utilized death records from the CDC in their analysis, comparing COVID-19 to common causes such as cancer and heart disease. COVID-19 was a top cause of death for every age group over age 15, the study found.
- COVID-19 disparities in Louisiana: Another notable study this week: researchers at the University of Maryland, College Park examined the roles of social, economic, and environmental factors in COVID-19 deaths in Louisiana, focusing on Black residents. “We find that Black communities in parishes with both higher and lower population densities experience higher levels of stressors, leading to greater COVID-19 mortality rate,” the researchers wrote. The study’s examination of environmental racism in relation to COVID-19 seems particularly novel to me; I hope to see more research in this area.
- Tracking coronavirus variants in wastewater: And one more new study: a large consortium of researchers, led by scientists at the University of California San Diego, explores the use of wastewater surveillance to track new variants. Variants can show up in wastewater up to two weeks earlier than they show up in samples from clinical (PCR) testing, the researchers found. In addition, some variants identified in wastewater are “not captured by clinical genomic surveillance.”
- Global COVID-19 vaccine and treatment initiative ending: The ACT-Accelerator, a collaboration between the World Health Organization and other health entities and governments, has run out of funding. This is bad news for low- and middle-income countries that relied on the program for COVID-19 vaccines and treatments—many of which are still largely unvaccinated, more than a year after vaccines became widely available in high-income countries. Global health equity initiatives will likely continue in another form, but funding will be a continued challenge.
-
Pandemic preparedness: Improving our data surveillance and communication
Screenshot of the new Biden COVID-19 plan. As COVID-19 safety measures are lifted and agencies move to an endemic view of the virus, I’m thinking about my shifting role as a COVID-19 reporter. To me, this beat is becoming less about reporting on specific hotspots or control measures and more about preparedness: what the U.S. learned from the last two years, and what lessons we can take forward—not just for the future COVID-19 surges that are almost certainly coming, but also for future infectious disease outbreaks.
To that end, I was glad to see the Biden administration release a new COVID-19 plan focused on exactly this topic: preparedness for new surges, new variants, and new infectious diseases beyond this current pandemic.
From the plan’s executive summary:
Make no mistake, President Biden will not accept just “living with COVID” any more than we accept “living with” cancer, Alzheimer’s, or AIDS. We will continue our work to stop the spread of the virus, blunt its impact on those who get infected, and deploy new treatments to dramatically reduce the occurrence of severe COVID-19 disease and deaths.
The Biden plan was released last week, in time with the president’s State of the Union address. I read through it this morning, looking for goals and actions connected to data collection and reporting.
Here are a few items that stuck out to me, either things that the Biden administration is already doing or should be doing:
- Improving surveillance to identify new variants: The U.S. significantly improved its variant sequencing capacity in 2021, multiplying the number of cases sequenced by more than tenfold from the beginning to the end of the year. But the new Biden plan promises to take these improvements further, by adding more capacity for sequencing at state and local levels—and, crucially, “strengthening data infrastructure and interoperability so that more jurisdictions can link case surveillance and hospital data to vaccine data.” In plain language, that means: making it easier to track breakthrough cases (which I have argued is a key data problem in the U.S.).
- Expanding wastewater surveillance: As I’ve written before, in the current national wastewater surveillance network, some states are very well-represented with over 50 collection sites; while other states are not included in the data at all. The Biden administration is committed to bring more local health agencies and research institutions into the surveillance network, thus expanding our national capacity to get early warnings about surges.
- Standardizing state and local data systems: I’ve written numerous times that the U.S. suffers from a lack of standardization among its 50 different states and hundreds of local health agencies. According to the new plan, the Biden administration plans to facilitate data sharing, aggregating, and analyzing data across state and local agencies—including wastewater monitoring and other potential methods of surveillance that would provide early warnings of new surges. This would be huge if it actually happens.
- Modernize the public health data infrastructure: One thing that could help health agencies better coordinate and share data: modernizing their data systems. That means phasing out fax machines and mail-in reports (which, yes, some health departments still use) and investing in new electronic health record technologies, while hiring public health workers who can manage such systems.
- Use a new variant playbook to evaluate new virus strains: Also in the realm of variant preparedness, the Biden administration has developed a new “COVID-19 Variant Playbook” that may be used to quickly determine how a new variant impacts disease severity, transmissibility, vaccine effectiveness, and other factors. The new playbook may be used to quickly update vaccines, tests, and treatments if needed, by working in partnership with health systems and research institutions.
- Collecting demographic data on vaccinations and treatments: The Biden plan boasts that, “Hispanic, Black, and Asian adults are now vaccinated at the same rates as White adults.” However, CDC data shows that this trend does not hold true for booster shots: eligible white Americans are more likely to be boosted than those in other racial and ethnic groups. The administration will need to continue collecting demographic data to identify and address gaps among vaccinations and treatments; indeed, the Biden plan discusses continued efforts to improve health equity data.
- Tracking health outcomes for people in high-risk settings: Along with its health equity focus, the Biden plan discusses a need to better track and report on health outcomes in nursing homes, other long-term care facilities, and other congregate settings like correctional facilities and homeless shelters. Congregate facilities continue to be major COVID-19 hotspots whenever there’s a new outbreak, so improving health standards in these settings should be a major priority.
- Studying and combatting vaccine misinformation, vaccine safety: The new plan acknowledges the impact of misinformation on vaccine uptake in the U.S., and commits the Biden administration to addressing this trend. This includes a Request for Information that will be issued by the Surgeon General’s office, asking researchers to share their work on misinformation. Meanwhile, the administration will also continue monitoring vaccine safety and reporting these data to the public.
- Test to Treat: One widely publicized aspect of the Biden plan is an initiative called “Test to Treat,” which would allow people to get tested for COVID-19 at pharmacies, health clinics, long-term care facilities, and other locations—then, if they test positive, immediately receive treatment in the form of antiviral pills. If this initiative is widely funded and adopted, the Biden administration should require all participating health providers to share testing and treatment data. This would allow researchers to evaluate whether this testing and treatment rollout has been equitable across different parts of the country and minority groups.
- Website for community risk levels and public health guidance: The Biden plan includes the launch of a government website “that allows Americans to easily find public health guidance based on the COVID-19 risk in their local area and access tools to protect themselves.” The CDC COVID-19 dashboard was recently redesigned to highlight the agency’s new Community Level guidance, which is likely connected to this goal. Still, the CDC dashboard leaves much to be desired when it comes to comprehensive information and accessibility, compared to other trackers.
- A new logistics and operational hub at HHS: In the last two years, the Department of Health and Human Services (HHS) built up an office for coordinating the development, production, and delivery of COVID-19 vaccines and treatments. The new Biden plan announced that this office will become a permanent part of the agency, and may be used for future disease outbreaks. At the same time, the Biden administration has added at-home tests, antiviral pills, and masks to America’s national stockpile for future surges; and it is supporting investments in laboratory capacity for PCR testing.
- Tracking Long COVID: Biden’s plan also highlights Long COVID, promoting the need for government efforts to “detect, prevent, and treat” this prolonged condition. The plan mentions NIH’s RECOVER initiative to study Long COVID, discusses funding new care centers for patients, and proposes a new National Research Action Plan on Long COVID that will bring together the HHS, VA, Department of Defense, and other agencies. Still, the plan doesn’t discuss actual, financial support for patients who have been out of work for up to two years.
- Supporting health and well-being among healthcare workers: The new Biden plan acknowledges major burnout among healthcare workers, and proposes a new grant program to fund mental health resources, support groups, and other systems of combatting this issue. Surveying healthcare workers and developing systematic solutions to the challenges they face could be a major aspect of preparing for future disease outbreaks. The Biden plan also mentions investing in recruitment and pipeline programs to support diversity, equity, and inclusion among health workers.
- More international collaboration: The new Biden plan also focuses on international aid—delivering vaccine donations to low-income nations—and collaboration—improving communication with the WHO and other global organizations that conduct disease surveillance. This improved communication may be especially key for identifying and studying new variants in a global pandemic surveillance system.
This week, a group of experts—including some who have advised the Biden administration— followed up on the Biden plan with their own plan, called “A Roadmap for Living with COVID.” The Roadmap plan also emphasizes data collection and reporting, with a whole section on health data infrastructure; here, the authors emphasize establishing centralized public health data platforms, linking disparate data types, designing data infrastructure with a focus on health equity, and improving public access to data.
Both the Biden administration’s plan and the Roadmap plan give me hope that U.S. experts and leaders are thinking seriously about preparedness. However, simply releasing a plan is only the first step to making meaningful changes in the U.S. healthcare system. Many aspects of the Biden plan involve funding from Congress… and Congress is pretty unwilling to invest in COVID-19 preparedness right now. Just this week, a $15 billion funding plan collapsed in the legislature after the Biden administration already made major concessions.
Readers, I recommend calling your Congressional representatives and urging them to support COVID-19 preparedness funding. You can also look into similar measures in your state, city, or other locality. We need to improve our data in order to be prepared for future disease outbreaks, COVID-19 and beyond.
More national data