- CDC awards $3 billion to improve public health infrastructure: The CDC announced this week that it has awarded state and local public health agencies a total of $3.2 billion to support hiring and training new workers, along with other infrastructure needs. The agency published a breakdown of all the agencies that received awards, although it has not included specific details on what funds will be used for in each place. Local reporters, if your health department received funding, this might be worth looking into!
- CDC expands wastewater testing for polio: Another notable CDC announcement this week: the agency is expanding its wastewater surveillance for polio to two new areas, Oakland County, Michigan and Philadelphia. Testing wastewater for polio is more complicated than testing it for the coronavirus, as STAT News’ Helen Branswell explains in this article; as a result, the CDC is expanding this surveillance in a more limited capacity than what it’s doing for other viruses, like monkeypox and the flu.
- Majority of COVID-19 deaths are now among vaccinated people: A new report from the Kaiser Family Foundation explains why more than 50% of COVID-19 deaths in the U.S. in recent months were among people who had received at least two vaccine doses. According to KFF, factors driving this trend include the rising share of Americans who are vaccinated, waning protection from initial doses, and low uptake of booster shots—particularly of the Omicron-specific boosters that provide better protection against newer variants. More reason to get the new booster if you haven’t yet!
- Paid sick leave correlates with higher vaccination rates: Speaking of vaccination: a new study from researchers at Drexel University and Boston University found that large U.S. cities with city-wide paid sick leave policies had higher vaccination rates than those without such policies. The correlation was particularly evident in neighborhoods with higher social vulnerability, the researchers found. Expanding paid sick leave could help reduce inequities in vaccination coverage, the paper’s authors recommend.
- No monoclonal antibody drugs are currently authorized in the U.S.: This week, the FDA announced that bebtelovimab, a monoclonal antibody made by Eli Lilly, is no longer authorized for COVID-19 treatments in the U.S. The drug was designed based on older versions of the Omicron variant and doesn’t perform well against BQ.1 and BQ.1.1, the sublineages that are currently causing the majority of new cases in the U.S. As a result, no monoclonal antibodies are currently authorized, though Paxlovid and other treatments are still available.
Tag: monoclonal antibodies
-
Sources and updates, December 4
-
Contracted staffing issues in Missouri reveal broader crisis in hospitals

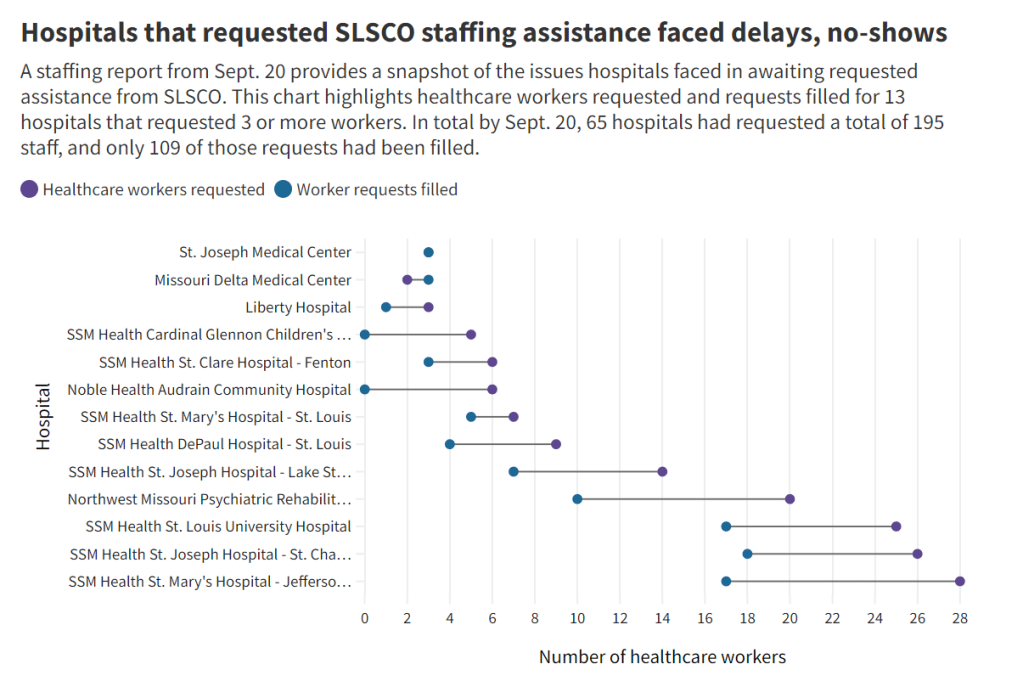
Chart from the Missouri Independent story. Early this week, I had a big story published in The Missouri Independent, as part of the Documenting COVID-19 project’s ongoing collaboration with that nonprofit newsroom. This piece goes in-depth on the Missouri health department’s contract with SLSCO, a Texas-based construction company that expanded to provide healthcare support during the pandemic.
While this was a local story, to me, the piece provides important insights about the type of support that is actually needed in U.S. hospitals right now: not temporary assistance, but long-term, structural change.
The Missouri agency hired SLSCO to provide two services, with a total contract of $30 million:
- Provide staffing support (nurses, technicians, etc.) to hospitals across the state struggling in the wake of the Delta surge.
- Set up, staff, and operate six monoclonal antibody infusion sites where Missourians infected with the coronavirus could easily access the treatment.
SLSCO made lofty promises to the Missouri health department, citing its ability to quickly send hundreds of workers to facilities that required assistance. But in fact, the hospital staffing assistance was marred by delays, no-shows, and high rates.
Here are a few paragraphs from the story:
Fewer hospitals signed on to receive staff than the Department of Health and Senior Services anticipated. Within the first few weeks, some hospitals faced no-shows, while the company’s hourly rates — up to $215 an hour for some nurses and $550 an hour for doctors — were too high for other hospitals to afford after state funds ran out, according to emails obtained by The Independent and the Documenting COVID-19 project through records requests. (Copies of SLS’ contract and emails between state agencies can be found here.)
“153 staff requested and only 10 deployed,” wrote Alex Tuttle, the governor’s legislative budget director, after receiving a staffing report early in the contract period. “Am I reading that right?”
From mid-August through November, just 206 staff were ultimately sent to 53 hospitals, said Lisa Cox, a spokeswoman for DHSS. The healthcare support had left by the time omicron hit in the winter.
The monoclonal antibody infusion sites were more successful; in fact, the Missouri health department ended up redirecting funding from the staffing support to the infusion sites. The six sites served a total of 3,688 patients over a two-month period.
However, the sites could have served a lot more patients: these clinics could have treated up to 136 patients each day but peaked at about 90, with numbers often much lower, according to my analysis of data from the health department. Due to these low numbers, the state of Missouri ended up spending more than $5,600 for each patient. One monoclonal antibody expert I talked to for the piece called this an “exorbitant” cost.
Now, I don’t mean to hate on monoclonal antibody treatments here—these drugs are truly a great way to boost the immune systems of COVID-19 patients who may be at higher risk for severe symptoms. Maggie Schaffer, a case management nurse who helped set up one of the infusion sites, told me that people who had this treatment typically are “feeling like a whole new person” within a day or two.
However, the treatments are very expensive and inefficient; one patient’s infusion appointment can take hours. The drugs themselves cost around $2,100 per dose, about 100 times as much as one vaccine. Health departments and facilities that offer monoclonal antibodies need to focus on getting the word out to patients so that these expensive supplies aren’t wasted.
At the same time, temporary healthcare staff can be great to help a facility out a surge—but they are not a long-term solution. In particular, nurses at a hospital may be frustrated by watching new staff come in from out of town and receive much higher pay rates; the “traveling nurse phenomenon,” as this is called, may contribute to burnout and staff leaving to go become traveling workers themselves.
What do hospitals actually need to do to address their staffing crisis? Here are a few ideas from Tener Veenema, a nursing expert focused on health systems a professor of nursing who researches health systems and emergency preparedness at Johns Hopkins’ Bloomberg School of Public Health:
- Higher pay and assistance with education bills.
- Regulations on things like work hours, the number of patients one nurse can be responsible for at once.
- Mental health assistance that nurses are actually given time and space to access.
I’ll end the post with this quote from Veenema, which is also the last line of the story:
“If we don’t fix the toxic work environment, this issue of mandatory overtime, inadequate staffing levels, lack of time to access mental health resources,” Veenema said, “then you’re simply shooting more new nurses out of the cannon, but into the lake where they’re going to drown.”