- New Long COVID review from PLRC and Scripps: Leading Long COVID researchers from the Patient-Led Research Collaborative and the Scripps Research Translational Institute collaborated on a review paper published this week in Nature, summarizing major findings from the literature so far. The paper includes summaries of major symptoms (ranging from cardiac damage to cognitive impairment), correlations between Long COVID and other chronic diseases (ME/CFS, POTS, etc.), treatment options for specific symptoms and/or biological mechanisms, and much more. I haven’t had a chance to read the paper in full yet, but I anticipate that it will be a valuable resource for future research.
- Vaccines still reduce risk of transmission: Another recent paper in Nature reports on the impact of vaccination among inmates in the California state prison system. Researchers at the University of California San Francisco analyzed COVID-19 surveillance data from 35 prisons during the early months of Omicron (December 2021 to May 2022). They found patients infected with Omicron after vaccination and/or a prior infection had lower risks of transmitting the virus to others. The study suggests that vaccination (and prior infection) is still helpful in reducing COVID-19 spread in addition to reducing severe symptoms, even at this point in the pandemic. (H/t Your Local Epidemiologist.)
- Coronavirus found in airplane wastewater on international flights: In a small study, researchers at the National Public Health Laboratory of Malaysia tested wastewater samples from 29 flights that arrived at Kuala Lumpur from outside the country. The researchers found that SARS-CoV-2 was present on 28 of the 29 flights—and testing for the remaining flight wasn’t yet complete, according to a local news outlet that covered the study. While this is a relatively small sample, the results suggest that COVID-19 is very prevalent in travel settings. The study also serves as a helpful example for future plane wastewater testing.
- New report highlights nursing home issues: A recent report from the American Health Care Association shares results from a survey of 524 nursing homes across the U.S. The findings show challenges with staffing and economic challenges; for example, 84% of the nursing homes surveyed reported “moderate to high levels of staffing shortages,” and 67% of the homes surveyed reported concerns that they may need to close their facilities due to staffing problems. (H/t POLITICO Pulse.)
- End of Ebola outbreak in Uganda: Finally, a bit of (non-COVID-19) good news: this week, health officials in Uganda declared the end of the country’s recent Ebola outbreak. The outbreak started in September 2022, and included a total of 164 cases and 55 deaths. The final patient of this outbreak was released from healthcare on November 30, according to the World Health Organization; Uganda successfully curbed the disease’s spread despite a lack of vaccines and treatments approved against the strain of Ebola that was spreading.
Tag: Long COVID
-
Sources and updates, January 15
-
Sources and updates, January 8
- NIH launches at-home testing telehealth program: This week, the National Institutes of Health announced the first location for “Home Test to Treat,” a new program that will make it easier for people in vulnerable communities to receive Paxlovid after testing positive on at-home, rapid tests. The Biden administration first announced this program in September, but it’s formally launching now with Berks County, Pennsylvania as the first participating community. As Paxlovid shifts to a drug that must be privately purchased instead of provided for free by the federal government, more programs like this one will be needed to fill access gaps.
- Study estimates global Long COVID prevalence: A large team of researchers, led by population health scientists at the University of Washington, conducted an extensive review of Long COVID symptoms. The analysis used 54 prior studies and two medical record databases, incorporating data from 1.2 million people in total. Overall, about 6% of patients reported at least one class of Long COVID symptoms three months after their initial infections, with the vast majority of cases occurring in people who had mild acute cases. The study was published in JAMA in October, but gained attention this week thanks to an article that its leading authors wrote in The Conversation.
- China’s COVID-19 data are unreliable: It’s been about a month since China loosened its COVID-19 protocols in the wake of protests and contagious Omicron subvariants, and the country is now facing a massive surge—with as many as one million new cases a day according to some modeling estimates. Yet COVID-19 deaths reported in the country have been very low, fewer than five a day. This discrepancy suggests that China’s authorities are not correctly counting their COVID-19 deaths, while the country’s dismantled testing infrastructure has also led to less reliable case numbers. Officials from the World Health Organization have formally called on the country to “be more forthcoming with information” about its COVID-19 surge, reports Helen Branswell at STAT News.
- CDC testing airplane wastewater on flights from China: In response to surveillance concerns, the CDC is working to test wastewater on flights arriving from China in select U.S. airports. This method is, of course, more efficient than testing every single traveler from the country in the interest of identifying any new variants that might arise. (Though it’s worth noting that some experts are skeptical about the potential of new variants arising in China.) Scientists from Concentric, a company that works with the CDC on traveler surveillance, previously talked about plane wastewater testing during our interview in November.
- Race/ethnicity differences among child vaccination rates: Finally, a notable study in this week’s CDC Morbidity and Mortality Weekly Report: researchers at the CDC and collaborators examined vaccination rates among children ages five to 17 using data from the National Immunization Survey. They found vaccination coverage (with at least one dose) was highest among Asian children (at about 75%), followed by Hispanic or Latino children (49%), white children (45%), and Black children (43%). The researchers also noted differences among vaccination rates by other socioeconomic factors, and by parents’ mask-wearing habits.
-
New CDC report vastly underestimates deaths with Long COVID

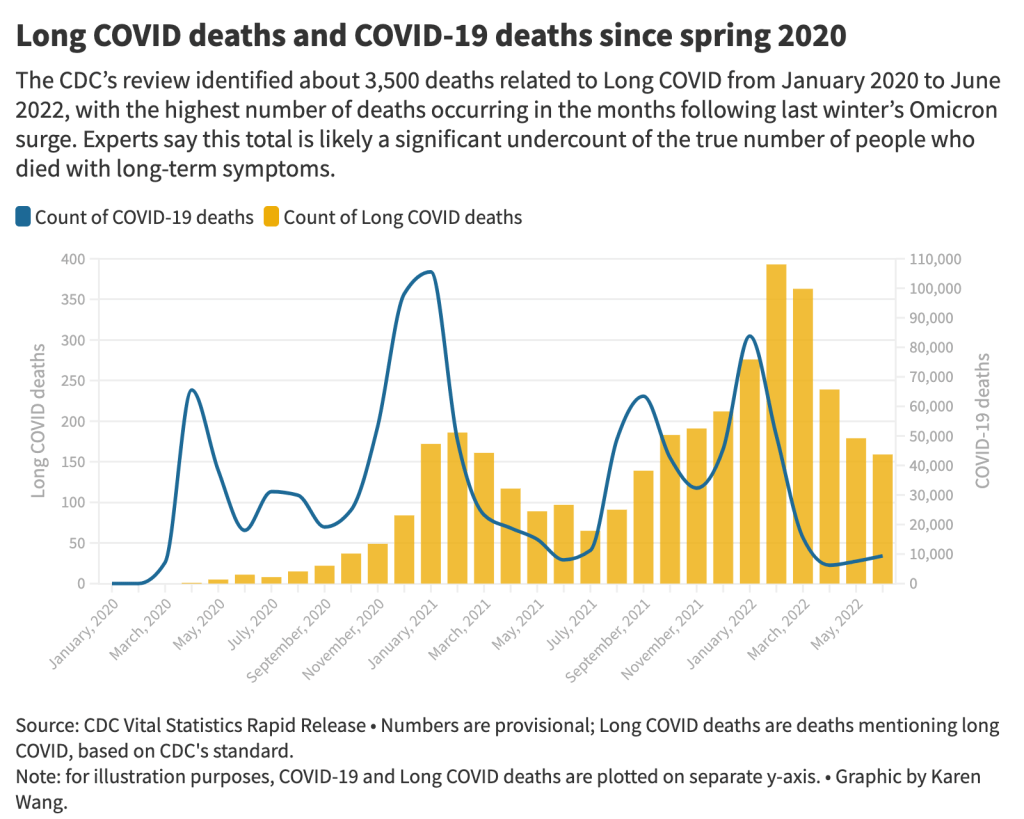
The 3,500 Long COVID-related deaths identified by the CDC’s review of death certificates are likely a significant undercount of mortality caused by this condition, experts say. Chart by Karen Wang; see the interactive version on MuckRock. On Wednesday, the CDC’s National Center for Health Statistics (NHCS) released a major report on deaths from Long COVID. To identify a small (but significant) number of deaths, NCHS researchers searched through the text of death certificates for Long COVID-related terms. Their study demonstrates how bad our current health data systems are at capturing the results of chronic disease.
My colleagues and I at MuckRock did a similar analysis to the CDC’s, searching death certificate data that we received through public records requests and partnerships in Minnesota, New Mexico, and counties in California and Illinois. You can read our full story here and explore the death certificate data we analyzed on GitHub.
Here are the main findings from both analyses:
- The CDC study is an important milestone in recognizing the reality of Long COVID: this is a serious, chronic disease that can lead to death for some patients. It’s not just an outcome of acute COVID-19.
- From its national death certificate search, NCHS identified 3,544 deaths with Long COVID as a cause or contributing factor. This is almost certainly a major undercount, experts told me (and told other reporters who wrote about the study.)
- This number is an undercount because we’re essentially seeing two poor-quality data systems intersect. Long COVID is undercounted in clinical settings because we lack standard diagnostic tools and widespread medical education about it—most doctors wouldn’t think to put it on a death certificate as a result. And the U.S.’s death investigation system is uneven and under-resourced, leading to inconsistencies in tracking even well-known medical conditions.
- On top of these problems, when Long COVID is diagnosed, it tends to be among people who had severe cases of acute COVID-19 followed by difficulty recovering, experts told me. David Putrino and Ziyad Al-Aly, two leading Long COVID researchers, both pointed to the NCHS’s trend towards identifying Long COVID deaths among older adults (over age 75) as an example of this pattern in action, since this group is at higher risk for more severe acute symptoms.
- The NCHS count of deaths thus misses Long COVID patients with symptoms similar to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), which often arises after a milder initial case. It also misses people who have vascular impacts from a COVID-19 case, like a premature heart attack or stroke months after infection—something Al-Aly and his team have studied in depth. And, crucially, the NCHS count misses people who died from suicide, after suffering from severe mental health consequences of Long COVID.
- While the NCHS count of Long COVID deaths is far too low to be accurate, the researchers did find more deaths as the pandemic went on—with the highest number in February 2022, following the first Omicron surge. This pattern could suggest increased recognition of Long COVID among the medical community.
- The NCHS primarily identified Long COVID deaths among white people, even though acute COVID-19 has disproportionately impacted people of color in the U.S. Experts say this mismatch could reflect gaps in access to a diagnosis and care for Long COVID: if white people are more likely to be seen by a doctor who can accurately diagnose them, they will be overrepresented in Long COVID datasets. Putrino called this “a health disparity on top of a health disparity.”
- MuckRock’s analysis of death certificate data in select states similarly found that most deaths labeled as Long COVID were among seniors and white people. The trends varied by state, though, reflecting differences in populations and in local death reporting systems. For example in New Mexico, which has a statewide medical examiner’s office (rather than a looser system of county coroners), three-fourths of the Long COVID deaths were among Hispanic or Indigenous Americans.
- Our story also includes details about the RECOVER initiative’s autopsy study, which aims to use extensive postmortem testing on people who might have died from acute COVID-19 or Long COVID to identify biological patterns. Like the rest of RECOVER, this study is moving slowly and facing logistical challenges: about 85 patients have been enrolled so far, an investigator at New York University said.
Overall, the NCHS study suggests an urgent need for more medical education about Long COVID, especially as the CDC works to implement a new death code specific to this chronic condition. We also need broader outreach about the consequences of Long COVID. To quote from the story:
“Institutions like the CDC should do more to educate people about the long-term problems that could follow a COVID-19 case, said Hannah Davis, the patient researcher. “We need public warnings about risks of heart attack, stroke and other clotting conditions, especially in the first few months after COVID-19 infection,” she said, along with warnings about potential links to conditions like diabetes, Alzheimer’s and cancer.
And we need other methods of studying Long COVID outcomes that don’t rely on a deeply flawed death investigation system. These could include studies of excess mortality following COVID-19 cases, Long COVID patient registries that monitor people long-term, and collaborations with patient groups to track suicides.
For any reporters and editors who may be interested, MuckRock’s story is free for other outlets to republish.
More Long COVID reporting
-
COVID-related nonprofits taking donations this holiday season
Last week, in response to my call for donations to the COVID-19 Data Dispatch, I received some very generous support from readers. Thank you to everyone who donated—you are truly helping me keep this a free, accessible publication for anyone following COVID-19 news.
Following up on last week’s post, I wanted to share some suggestions for other COVID-related organizations that are taking donations this holiday season. If you have the resources and are looking for places to donate, please consider these nonprofits!
- Body Politic, which runs one of the foremost Long COVID online support groups, is seeking donations to transition from a grassroots, all-volunteer organization to a format that’s more sustainable in the long-term. Their funding goal is $500,000.
- The COVID-19 Longhauler Advocacy Project seeks donations to support its work advancing Long COVID research and supporting patients. Like Body Politic, this organization was founded by volunteers themselves dealing with Long COVID.
- Marked by COVID is a nonprofit advocacy organization, also volunteer-run, seeking recognition of the Americans who lost their lives to COVID-19 and improved public health policies in the U.S.
- Peste Magazine is a new online magazine focused on health journalism, advocacy, and the arts. The publication’s work so far has focused on COVID-19 but also includes other health justice topics; donations help to support payments for writers.
- ME Action is a leading advocacy organization for people with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), a chronic condition that shares many symptoms with (and is often co-diagnosed with) Long COVID. Since the pandemic started, it’s also been involved with Long COVID advocacy.
- Solve ME/CFS is another advocacy organization for ME/CFS and now Long COVID, focused particularly on funding and supporting research on these conditions.
- Dysautonomia International is a leading advocacy group for dysautonomia, an umbrella term for conditions involving a malfunctioning autonomic nervous system. Similar to ME/CFS, dysautonomia is often a co-diagnosis for Long COVID.
- Your local mutual aid group: Early in the pandemic, hundreds of mutual aid groups started across the country to help share food and other supplies with people in need. Some of them are still doing this important work! Websites like Mutual Aid Hub and this NYC directory can help you find a group in your area.
Disclaimer: This is not sponsored content, these recommendations come from my own research and reporting on COVID-19. If you’d like to recommend another organization, let me know and I’ll include it in a future issue.
-
The future of tracking Long COVID
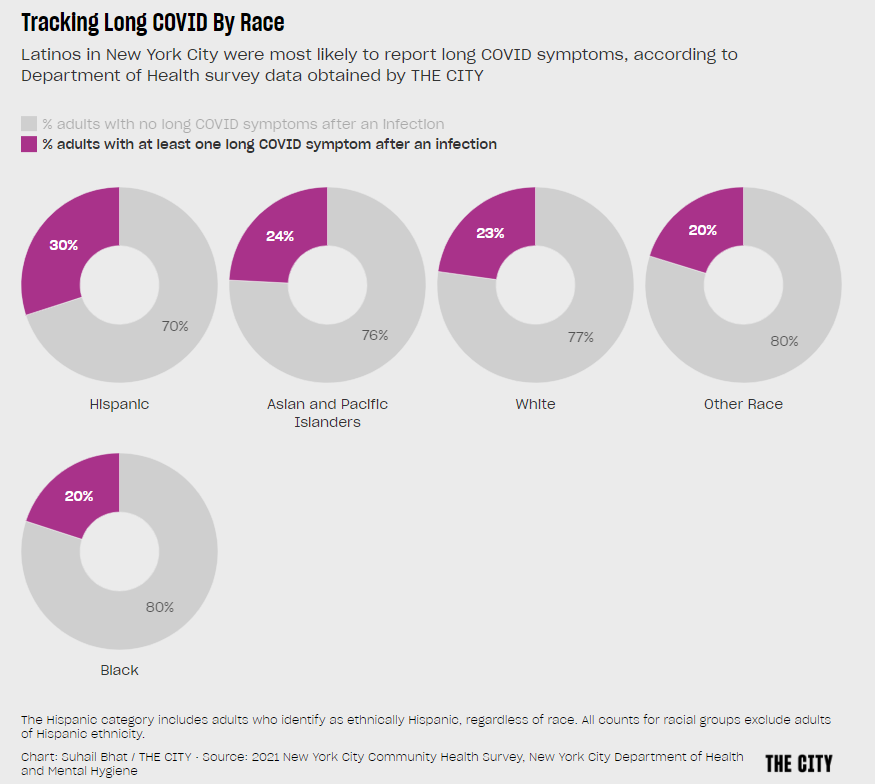
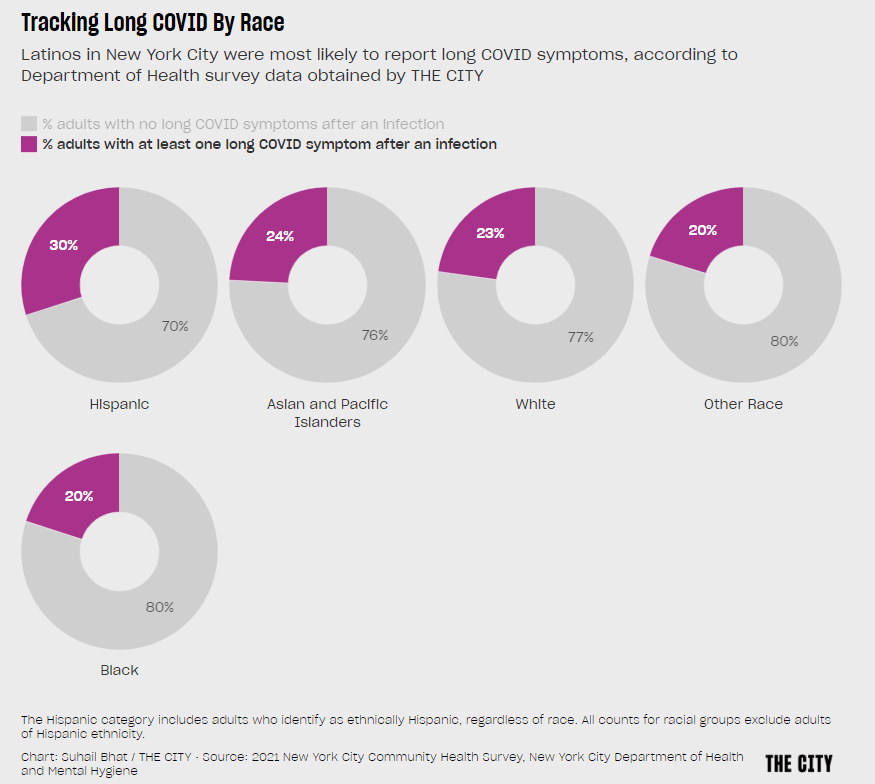
Hispanic or Latino New Yorkers were more likely to report Long COVID symptoms than other demographic groups, in a 2021 survey by the city health department. Chart via THE CITY. I had two new articles about Long COVID published this week:
- This story in Science News describes how researchers are working to fill gaps in Long COVID data, largely by collaborating with patients and across different areas of medicine.
- This story in Gothamist/WNYC describes three public Long COVID clinics run by New York City Health + Hospitals, which offer a range of care to New Yorkers with the condition but fall short of all the specialties needed for comprehensive treatment.
The reporting process for both stories gave me a lot to think about, in considering potential improvements in recording who has Long COVID and how this chronic disease impacts people.
And we have a lot of room for improvement. There are plenty of reasons why Long COVID research and data collection are currently difficult, ranging from a lack of consistency in how the condition is diagnosed to historical underfunding for similar chronic diseases like myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia. For more details, see this post I wrote in May.
The U.S. scientific and medical systems also made specific mistakes early in the pandemic that contributed to our current data gaps, including the dearth of PCR testing—leading many current long-haulers to not have positive test results from their initial infections—and early refusals by many doctors to believe patients’ prolonged symptoms had resulted from the coronavirus. Most medical schools do not spend much time training new doctors to recognize complex, chronic diseases, leaving them unprepared to tackle Long COVID.
But these problems can be addressed—especially if doctors and researchers are willing to step outside their specific fields to collaborate with each other and with patients. Here are a few specific recommendations that I learned about in reporting my stories for Science News and Gothamist/WNYC.
Listen to and collaborate with patients.
“Patients know the right questions to ask to properly document their experience,” Lisa McCorkell, one of the founders of the Patient-Led Research Collaborative (PLRC), told me in an email interview for my story.
In fact, a survey study by PLRC in which patient-researchers asked other long-haulers to describe their symptoms is considered one of the most comprehensive accounts of this condition. Other researchers have used this list of symptoms in designing their own patient surveys.
Surveys are one important mechanism of compiling patient experiences, as they can capture information that does not make it into medical records. (Common Long COVID symptoms like post-exertional malaise often are not well-captured in these records.) But patients can also weigh in on other aspects of study methodologies, such as how to collect data in a way that won’t overly tax participants or how to compare groups of patients for accurate results.
Plus, hypotheses from patients can be valuable starting points for clinical trials, as Julia Moore Vogel from the Scripps Research Translational Institute explained to me. Vogel, who is a long-hauler herself, is working on a new study at Scripps that’s informed by her and other patients’ experiences with Garmin wearable devices. The projects funded by PLRC’s grant program offer further examples of research studies informed by patient priorities.
Connect health records from different sources.
One major challenge with studying Long COVID is that this complex condition can impact every organ system in the body. You can’t just analyze heart disease records from a cardiology practice, or lung function records from a pulmonary practice. Every patient could be seeing ten or more different specialists, and all of those doctors might inform different pieces of the overall disease puzzle.
As a result, devising systems that better compile and connect records from different sources is a priority for researchers studying Long COVID. Arjun Venkatesh, a patient-reported outcomes researcher, described this as “the clunkiest part” of his work: there are a lot of “hidden barriers” to connecting records, he said, ranging from privacy protections to technical mismatches. (For example, a patient requesting their records from a particular doctor might be asked to provide a fax number, something most people do not have in 2022.)
Still, new projects are in the works to make this type of data sharing easier. One example is Kindred, an app designed by Yale researchers that empowers patients to request their electronic health records and share them with scientists studying Long COVID. Patients also have more legal protections in making data requests now, thanks to a new federal rule that took effect this fall.
Use wearables and other new tracking technologies.
Smart watches, Fitbits, and other similar trackers are usually advertised for consumers interested in better tracking their individual health and fitness. But they can also provide valuable, long-term data to researchers studying health conditions like Long COVID.
The Scripps Research Translational Institute is one institution focused on wearable devices, through studies like Vogel’s and another program called the DETECT study, led by epidemiologist Jennifer Radin. In DETECT, researchers compile data from people across the country who have volunteered to share their wearable device data with Scripps. After one of the participants gets COVID-19, the scientists can compare their post-COVID health indicators to the patient’s pre-COVID baseline.
“We compare each person to themselves over time,” Radin told me when I talked to her for my Science News story. This method is different from traditional medical research, in which two similar groups of people are compared to each other on a population-wide basis.
Wearables research faces a lot of its own challenges, such as expanding access to more people (by making devices more affordable or even giving them to study participants for free) and creating analysis systems that can make sense of thousands of data points from each patient. But I personally find it fascinating and hope to continue covering this area. I was even inspired by my reporting to buy a smart watch, as a holiday present to myself.
Local surveys and outreach in partnership with community groups.
Anyone can get Long COVID—young or old, vaccinated or unvaccinated, with or without prior health conditions. But a lot of people still don’t know about this chronic condition, even when they might be experiencing long-term symptoms themselves.
As a result, a major priority for Long COVID researchers and patient-advocates is improving education and outreach about this condition. New York City has a program that could serve as an example here: NYC Health + Hospitals runs a hotline called AfterCare, which residents can call to learn about Long COVID and city resources, including the public clinics I wrote about.
While AfterCare has proactively called New Yorkers who previously tested positive for COVID-19, the program’s administrators are concerned that it’s likely not reaching everyone who could be served by the hotline. Local long-haulers who I talked to for my Gothamist/WNYC story want to see broader outreach—like subway ads, billboards, and commercials—telling people about Long COVID.
These same outreach programs could also help researchers collect more comprehensive data about Long COVID. Last week, THE CITY, another local NYC outlet, reported on some early results of a survey conducted by the city health department to find out which groups of New Yorkers are most vulnerable to the condition. Unsurprisingly, the survey found that Hispanic/Latino residents and those living in the Bronx were disproportionately impacted.
I hope to see more local health agencies follow in NYC’s lead to conduct surveys like this one, paired with outreach and education about Long COVID. This type of data could go a long way in showing political leaders where more resources are needed.
More Long COVID reporting
-
Sources and updates, November 27
- More data on the new, bivalent boosters: A new study, published this week in the CDC’s Morbidity and Mortality Weekly Report, has further evidence that the new, Omicron-specific booster shots provide additional protection against COVID-19 for people who previously received the original vaccines. Researchers used test results from pharmacies to compare symptomatic COVID-19 cases among people who had received the new boosters to those who had only received older vaccines. New booster recipients were less likely to get sick, they found, indicating protection against Omicron BA.4, BA.5, and their sublineages. In short: if you haven’t gotten one of the new boosters yet, now is a good time!
- Patient-Led Research Collaborative announces grant winners: The Patient-Led Research Collaborative, an organization of Long COVID patient-researchers that has produced groundbreaking work about this condition, just announced the winners of its $5 million fund to support new biomedical research on Long COVID. The winning projects will pursue avenues of top priority to patients, such as understanding post-exertional malaise, testing for microclots, and a clinical trial for the drug naltrexone. Projects were themselves evaluated by a panel of patient experts and patients will be heavily involved in the resulting research. Congrats to the PLRC team on this announcement, and I look forward to following the results of these studies!
- HHS publishes Health+ Long COVID report: Another piece of Long COVID news this week: the Department of Health and Human Services published a report summarizing interviews with people who have Long COVID. The report was one of several responses to the Biden administration’s call last spring for Long COVID research and support programs. It describes patients’ desires for meaningful research, better healthcare, financial support, and more. While this new report may not be adding much to the body of knowledge about Long COVID, it’s helpful to see this information coming from a major government source.
- Football games associated with COVID-19 spread: And one more study that caught my attention this week: a new paper in JAMA Network Open describes a correlation between National Football League (NFL) games and COVID-19 spikes in the surrounding counties during the league’s 2020-2021 season. Counties hosting more popular games (with at least 20,000 fans present) were more likely to see increased COVID-19 spread afterwards. The paper shows how large events can contribute to widespread disease transmission, even among people who didn’t themselves attend the events.
-
Long COVID book recommendations

The Long Haul and The Long COVID Survival Guide, pictured on Betsy’s desk. (Photo by Betsy Ladyzhets.) Two new books about Long COVID were published this month, and I’d like to recommend both of them to any readers interested in learning more about the condition—especially to other journalists covering COVID-19.
First, The Long COVID Survival Guide (from the Experiment Publishing, released November 8) is a compilation of essays from people with Long COVID, for people with Long COVID, edited by journalist and Body Politic founder Fiona Lowenstein. The book covers everything from getting a medical diagnosis to finding community with advocates for other chronic illnesses.
The Survival Guide is structured like a manual, every chapter ending with specific “survival tips” for long-haulers to use in their own Long COVID journeys. But it’s also a very relevant read for people who don’t have Long COVID, as it provides context about the different challenges long-haulers might go through: medical gaslighting, cognitive challenges, women’s health issues, learning to ask for help, and more.
Personally, I got a lot of ideas for future journalism projects from this book. As someone covering scientific research and data, I found the chapters about getting a diagnosis (by Dona Kim Murphey, Rachel Robles, and David Putrino) and about navigating Long COVID research (by Lisa McCorkell) particularly valuable.
Second, The Long Haul (from Simon & Schuster, released November 15) is a nonfiction narrative about how people with Long COVID came together to better understand the condition and advocate for themselves. Author Ryan Prior is a journalist with experience at CNN and other national outlets, and has lived with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) since he was a teenager.
Prior brings his lived experience and his journalistic experience—which includes covering other chronic illnesses and patient advocacy movements—to covering Long COVID. The book provides valuable backstories on major Long COVID groups, like Body Politic, the Patient-Led Research Collaborative, and the COVID-19 Longhauler Advocacy Project. It also describes early research efforts seeking to better understand Long COVID, including the first stages of the National Institutes of Health’s RECOVER study.
I’m still reading The Long Haul (as of this writing, I’m a couple of chapters in), but am already finding it incredibly helpful to learn about how Long COVID advocates started pushing for research and recognition, with context from ME/CFS and other post-viral illness work.
The Long COVID Survival Guide and The Long Haul might not be the most upbeat reading choices for the holiday season, but they’re really vital for anyone engaging with Long COVID—whether you’re a journalist covering this topic or a friend to a long-hauler. To quote from Dr. Akiko Iwasaki’s afterword, in the Survival Guide:
Long COVID has changed the narrative. The world no longer has any excuse to make the same mistake over and over again, as we have done for previous pandemic and endemic infections. It’s finally time for us to listen.
Transparency note: I received advanced copies of both of these books to aid in my work as a journalist covering Long COVID, but am not getting any compensation to write this post—i.e., this isn’t sponsored content or anything. I genuinely want more people to learn about and read these books!
More Long COVID reporting
-
Sources and updates, November 13
- Updated booster doses by state: This week, the CDC started reporting how many people have received the bivalent, Omicron-specific boosters by state, including state-level data for several demographic groups (over age 5, over 12, over 18, and over 65). The numbers are low: Vermont and Washington, D.C. have the highest booster rates as of November 9, with 21% and 20% of their populations receiving the bivalent shots, respectively. In about half of states, less than 10% of the population has received an updated booster. (H/t Jason Salemi.)
- Additional data suggests new boosters work against BQs: Speaking of the updated booster shots, a recent preprint from researchers at Emory University, Stanford University, and the NIH found that the new boosters produced several times more neutralizing antibodies against subvariants BQ.1.1 and BA.2.75.2 compared to the older vaccines. This was a small lab study and hasn’t yet been peer-reviewed, but it follows similar evidence from other research suggesting that the new boosters do provide additional protection against the most concerning variants currently circulating in the U.S. (See last week’s post.) If you haven’t gotten a bivalent booster yet, now is a good time!
- More evidence that masks in schools prevent COVID-19 spread: Another notable new study this week, published in the New England Journal of Medicine: a group of researchers from Boston institutions examined the differences in COVID-19 case numbers between public school districts that kept mask requirements in place during spring 2022, and those that lifted their requirements upon a statewide policy change in February. Overall, ending required masking led to “an additional 44.9 COVID-19 cases per 1,000 students and staff” during the remainder of the semester, the researchers found. The study demonstrates that masks are still a useful public health strategy to reduce illness—and risk of Long COVID—in schools.
- Paxlovid may reduce Long COVID risk: When Paxlovid first became available earlier in the year, some Long COVID patients reported that the drug helped alleviate their symptoms. A new study from Ziyad Al-Aly and his team at the Veterans Affairs St. Louis healthcare system provides evidence behind the anecdotal reports, finding that veterans treated with Paxlovid had a 25% lower risk of long-term symptoms, based on their electronic health records. The study has received some criticism (and has not yet been peer-reviewed); to me, it provides motivation for actual clinical trials examining Paxlovid’s use for treating Long COVID. RECOVER is running one such trial, but it won’t start until early 2023.
- Estimating COVID-19 infections from wastewater: And one more study that caught my attention this week: researchers at the University of Florida used a modeling technique called a “mass balance equation” to estimate how many people in Gainseville, Florida were sick with COVID-19 based on the virus’ concentration in wastewater. Using about one year of wastewater data (May 2020 to May 2021), the researchers were able to accurately predict actual infections with an error of just 1%. Translating wastewater data into useful information for public health action has been a major challenge for the growing field, so I was glad to see this study providing a potentially-useful method.
-
How data gaps contribute to financial challenges for people with Long COVID

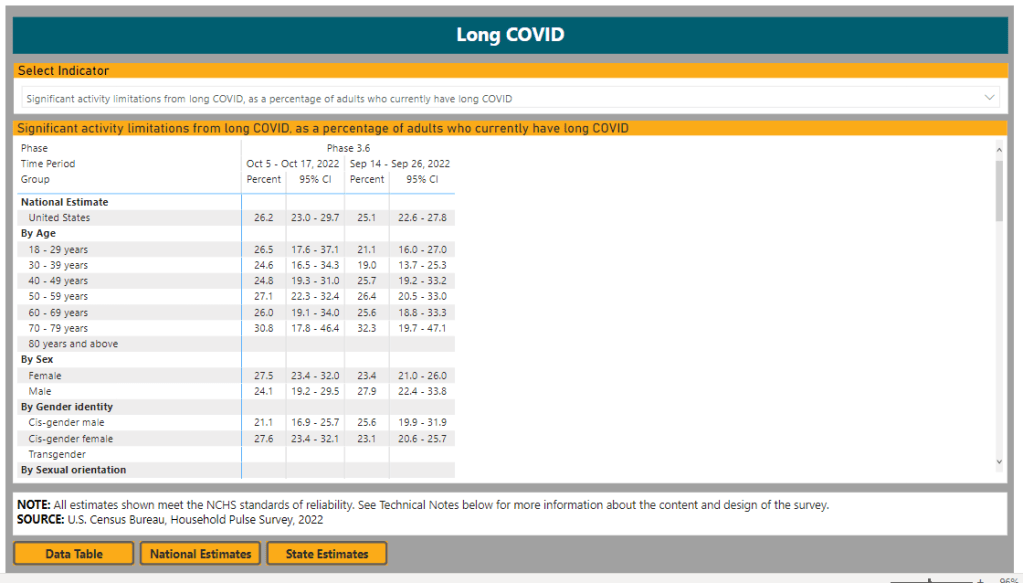
Long COVID symptoms place “significant activity limitations” on about one-quarter of patients, according to data from the Census and CDC’s Household Pulse Survey. This week, I had a story published at Kaiser Health News (KHN) about barriers that people with Long COVID are facing as they apply for disability benefits, focusing on programs offered by the federal Social Security Administration. For me, working on this story highlighted the consequences of the U.S.’s poor data collection on Long COVID.
The article shares stories from a couple of individual patients who are unable to work due to their Long COVID symptoms, but can’t access the support they need. Here’s how the story starts, focusing on Brooklyn mom Josephine Cabrera Taveras:
When Josephine Cabrera Taveras was infected with covid-19 in spring 2020, she didn’t anticipate that the virus would knock her out of work for two years and put her family at risk for eviction.
Taveras, a mother of two in Brooklyn, New York, said her bout with long covid has meant dealing with debilitating symptoms, ranging from breathing difficulties to arthritis, that have prevented her from returning to her job as a nanny. Unable to work — and without access to Social Security Disability Insurance or other government help — Taveras and her family face a looming pile of bills.
“We are in the midst of possibly losing our apartment because we’re behind on rent,” said Taveras, 32. Her application for Social Security disability assistance, submitted last fall, was rejected, but she is appealing.
Like many others with long covid, Taveras has fallen through the cracks of a system that was time-consuming and difficult to navigate even before the covid pandemic. People are facing years-long wait times, insufficient legal support, and a lack of clear guidance on how to prove they are disabled — compounded by the challenges of a medical system that does not have a uniform process for diagnosing long covid, according to health experts and disability attorneys.
Estimates of how many people might be in situations similar to Taveras vary widely. I cite a couple of differing estimates in the story: one report from the Brookings Institution suggests between two and four million people may be out of work due to Long COVID, while another from the National Bureau of Economic Research suggests the number is closer to 500,000.
The CDC and Census’ Household Pulse Survey reports about 14% of all U.S. adults have experienced Long COVID symptoms, and about one in four adults who currently have Long COVID are experiencing “significant activity limitations” due to their symptoms. But the Social Security Administration itself said that it’s only identified 40,000 disability claims that “include indication of a COVID infection at some point,” in a comment for my story.
Why do these estimates vary so much? It goes back to the beginning of the pandemic, when PCR tests were not available to many people who likely had COVID-19 and early long-haulers were dismissed by their doctors. As we approach three years with COVID-19, there’s still no clear process for diagnosing Long COVID—much less a comprehensive system for identifying and tracking patients. (Many patients also might not yet identify as disabled, but will start looking for government support in the coming years, advocates pointed out to me.)
Right now, individual long-haulers lack standards or guidance for the medical paperwork they need to access programs like social security disability. And at a broader level, we lack clear estimates of how many people with Long COVID need these programs. The Household Pulse Survey has been a useful step towards such estimates in recent months, but more detailed data are needed to actually tackle the employment crisis that Long COVID presents.
Even so, we know enough to say that this is a crisis. For the story, I talked to Katie Bach, a senior fellow at the Brookings Institution and author of the report cited above. She told me that, while researchers disagree on the scale of Long COVID’s impact on employment, even the lowest estimates are reason for concern.
“Even if the bottom end of my range is overstated by 100%, we’re still losing $50 billion a year in wages,” she said. “I don’t think anyone who looks seriously at Long COVID would say this is not a significant problem for the U.S.”
I hope to do more reporting on this problem; see last week’s post about my new project at MuckRock for more details. Also, the KHN story is freely available to republish, for any other news outlets that might be interested in sharing it!
More Long COVID reporting
-
Sources and updates, November 6
- New data on Omicron boosters: This week, we got two major updates on the safety and effectiveness of the bivalent, Omicron-specific booster shots from Pfizer and Moderna. First, a study in the CDC’s Morbidity and Mortality Weekly Report examined safety, finding that side effects of the new boosters similar to the side effects of previous vaccines, according to the agency’s vaccine surveillance systems. For example, about 60% of vaccine recipients experienced pain, swelling, or itching in the arms where they received the shot. And second, Pfizer and BioNTech shared new data about the companies’ bivalent booster, suggesting that the new booster produces four times more neutralizing antibodies against BA.4 and BA.5 compared to the original booster shot. The study focused on older adults (over age 55) but is still helpful evidence that the new boosters are more effective against currently-circulating variants.
- NIH RECOVER is preparing its first clinical trial: RECOVER, the National Institutes of Health’s flagship study to understand and eventually treat Long COVID, announced this week that it’s preparing clinical trials to test potential treatments. The first of these trials was recently posted to ClinicalTrials.gov (a site for tracking studies that have received federal funding). This trial will focus on testing Paxlovid for Long COVID patients, and RECOVER anticipates it will begin enrolling patients in early 2023. Patients have previously expressed concerns that RECOVER is moving pretty slowly with trials, considering how many Americans are impacted by Long COVID.
- Patients Rising Now Congressional Scorecard: Speaking of government action on medical issues: Patients Rising Now, an advocacy organization focused on patients with chronic illnesses, recently published its first scorecard for Congressional representatives. The resource grades every Senator and House member in the 117th Congress based on how their voting record aligns with the organization’s priorities. While COVID-19 is not specifically mentioned in the grades, this scorecard could have implications for future pandemic-related votes.
- COVID-19 vaccination and race/ethnicity inequities: A new paper from researchers at the University of Minnesota and Boston University examined how vaccination impacted COVID-19 mortality patterns in Minnesota. During the Delta and Omicron surges, the researchers found, mortality among middle-aged people of color was higher than mortality among white people in an age group ten years older. The paper shows that COVID-19 remains “a pandemic of the disadvantaged,” author Elizabeth Wrigley-Field wrote on Twitter. (Disclaimer: through my work at MuckRock, I am collaborating with BU researcher Andrew Stokes, one of the paper’s coauthors.)
- RSV vaccine(s) could be coming soon: Finally, a bit of good news about another respiratory virus: two potential vaccines for RSV are likely to be under FDA review in the coming months. Pfizer recently reported promising results from a clinical trial of a vaccine for pregnant people, who pass antibodies to their children (thus reducing infant RSV risk). And U.S. pharmaceutical company GSK reported results from a trial testing its RSV vaccine for older adults.