- Second Omicron boosters for high-risk adults: The FDA and CDC are planning to authorize a second round of bivalent, Omicron-specific vaccines for high-risk adults, the Washington Post reported this week. This decision will apply to Americans over age 65 and those who have compromised immune systems, with these groups becoming eligible four months after their initial bivalent boosters. It’s unclear exactly when the decision will become official; the FDA and CDC will make authorizations sometime “in the next few weeks,” according to WaPo.
- HHS announces (underwhelming) Long COVID progress: This week marks one year since Biden issued a presidential memo kicking off a “whole-of-government response” to Long COVID. The Department of Health and Human Services (HHS) commemorated the occasion with a fact sheet sharing the federal government’s progress so far. Unfortunately, that progress has been fairly minor, mostly consisting of reports and guidance that largely summarize existing government programs or build on existing systems (such as Veterans Affairs hospitals). Many of the Long COVID programs that Biden previously proposed have not received funding from Congress; meanwhile, the National Institutes of Health’s RECOVER initiative, the one program that has been funded, has faced a lot of criticism.
- RECOVER PIs recommend action on treatment: Speaking of RECOVER: this week, a group of scientists leading research hubs within the national study called for federal funding that would support treatment. The principal investigators (PIs) of these hubs have developed expertise in Long COVID through recruiting and studying patients, leading them to identify gaps in available medical care for long-haulers. To respond, the PIs recommend that Congress allocate $37.5 million to support Long COVID medical care at the RECOVER research sites. Their proposed budget includes patient outreach, telehealth support, educating healthcare workers on Long COVID, and more.
- Ventilation improvements in K-12 schools: The CDC released a new study this week in its Morbidity and Mortality Weekly Report, sharing results of a survey (conducted last fall) including about 8,400 school districts representing 62% of public school students in the U.S. Research company MCH Strategic Data asked the districts about how they’d improved ventilation in their school buildings, along with other COVID-19 safety measures. About half of the districts reported “maintaining continuous airflow in classrooms,” one-third reported HVAC improvements, 28% reported using HEPA filters, and 8% reported using UV disinfectants. The results indicate that many districts have a long way to go in upgrading their indoor air quality.
- Flu vs. COVID-19 mortality risk: Ziyad Al-Aly and his colleagues at the VA healthcare system in St. Louis have published another paper analyzing COVID-19 through the VA’s electronic health records. This study, published in JAMA Network, describes the mortality risk of COVID-19 compared to seasonal flu for patients hospitalized during the 2022-2023 winter season. The researchers evaluated about 9,000 COVID-19 patients and 2,400 flu patients, finding that risk of death for COVID-19 patients in the 30 days following hospitalization was about 1.6 times as high as the risk of death for flu patients. Despite great advances in vaccines and treatments, COVID-19 remains more dangerous than other seasonal viruses, the study suggests.
- Biobot launches mpox dashboard: This week, leading wastewater surveillance company Biobot Analytics launched a new dashboard displaying its mpox (formerly monkeypox) monitoring. Biobot tests for mpox at hundreds of sewage sites across the U.S., largely through its partnership with the CDC, and will continue this monitoring through at least summer 2023. The new dashboard shows mpox detections nationally over time and monitoring sites by state; it also includes some information on how mpox surveillance differs from COVID-19 surveillance.
Tag: Long COVID
-
Sources and updates, April 9
-
Sources and updates, March 26
- Paxlovid may lower risk of Long COVID: Taking paxlovid in the acute phase of a COVID-19 case may lower a patient’s risk of long-term symptoms by about 25%, according to a paper published this week in JAMA Internal Medicine. The paper, which summarizes an analysis of health records in the Veterans Affairs database, was originally posted as a preprint in the fall; lead author Ziyad Al-Aly and his colleagues at the St. Louis VA did more number-crunching during the peer review process. Several clinical trials (including one just announced at Yale this week) will test paxlovid as a potential treatment for Long COVID, with a longer course than people typically take during the acute disease.
- Estimating true vaccination rates in the U.S.: A new report from the COVID States Project, a group of academic researchers focused on connections between social behaviors and COVID-19 spread, provides estimates of vaccination rates by state in the U.S. The researchers compared vaccination data from the CDC to polling sources, including the Kaiser Family Foundation and original polling conducted by the COVID States Project. They found that CDC data often diverged from survey data, suggesting that the public health agency’s information has errors due to the CDC’s inability to connect disparate immunization records from different states. (In other words, if someone got their primary series in one state and a booster in another, they might show up twice in the CDC’s data.)
- Comparing COVID-19 outcomes by state: Another report looking at state-by-state data: researchers at the University of Washington’s Institute for Health Metrics and Evaluation compared COVID-19 death rates to state actions on COVID-19. The researchers found that states with higher poverty, more income inequality, higher Black and Hispanic/Latino populations, and less access to healthcare faced higher COVID-19 rates. States where more people voted for Trump in 2020 also saw more COVID-19. These patterns “seem to reflect the release of public health mandates” in more Republican states, journalist Amy Maxmen wrote in a Twitter thread summarizing the study.
- COVID-19 origins docs, raccoon dog analysis: Federal intelligence documents about investigations into the coronavirus’ origins will be declassified in the coming months, as required by a new law that President Biden signed this week. The law specifically requires that the Director of National Intelligence release “all information relating to potential links between China’s Wuhan Institute of Virology and COVID-19.” This information will first go to Congress, and then may become public. Meanwhile, there’s been some controversy about a recent analysis of viral samples at the Huanan Seafood Wholesale Market in Wuhan: news about this analysis was shared in the media before a scientific report was completed, and some researchers who worked on the analysis had their access to sequence repository GISAID revoked. This article in Science Magazine has more details on the situation.
- Increased Candida auris spread during the pandemic: C. auris is a pathogenic fungus that has developed resistance to multiple common drugs, and that can pose a serious threat to human health. (Yes, a fungus similar to the one that causes a pandemic in “The Last of Us”—though C. auris doesn’t turn people into zombies.) The fungus has spread more widely during the pandemic according to a recent CDC report, with a 44% increase in cases from 2019 to 2021. Other types of anti-microbial resistance have been on the rise as well, as COVID-19 led to less rigorous monitoring and heightened antibiotic use in many hospitals. More recent CDC data on the fungus are available here.
-
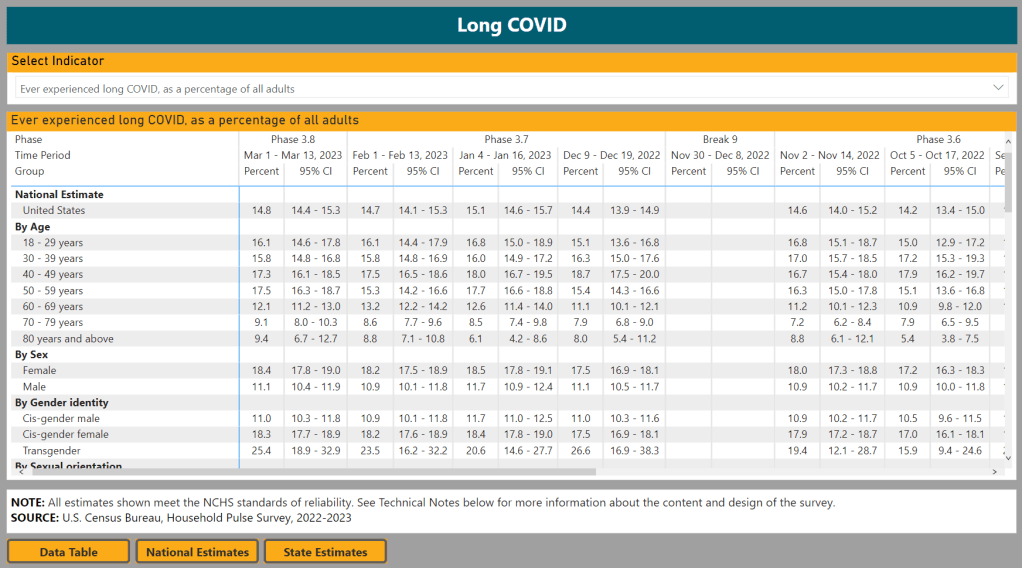
Pushing back against Long COVID misinformation

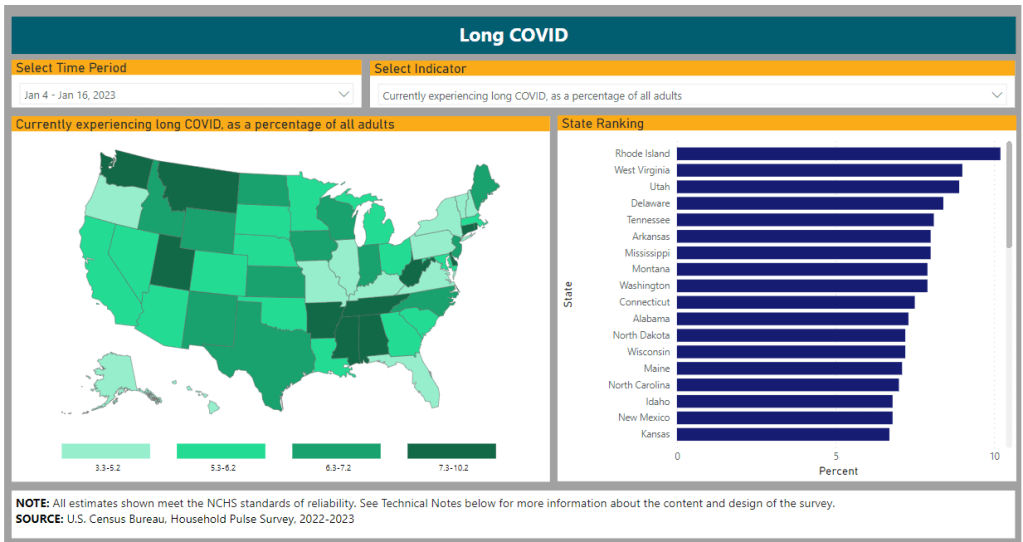
The CDC and Census’s Household Pulse Survey is one source showing the broad impacts of Long COVID. It’s an unfortunate reality in the Long COVID media landscape that a lot of journalists and commentators write about this condition without really doing their research. I frequently see articles that misunderstand key aspects of Long COVID or dismiss patients’ experiences.
Two recent stories (one in the Washington Post and one in Slate) make these mistakes, in fairly high-profile outlets. I’m not going to link to the full pieces here to avoid giving them more attention, but I wanted to share a bit about what these stories get wrong, to help readers recognize similar issues in other pieces.
The Washington Post piece discusses results from a data analysis project that the news outlet did in collaboration with Epic, an electronic health records company that has access to anonymized data from millions of people. Researchers evaluated whether patients had sought medical care for common Long COVID symptoms following a positive COVID-19 test. According to this analysis, Long COVID symptoms have become less common during the Omicron era compared to earlier COVID-19 waves—which may sound like a promising conclusion, until you recognize the analysis’ flaws.
Epic and the Washington Post didn’t share the full data behind this analysis, which makes it difficult to fully evaluate. But the public methodology provides enough information to be critical. First of all, relying on electronic health records for Long COVID leaves out a lot of people. Many of the people most vulnerable to this condition have limited access to PCR tests and to the doctors who might help them diagnose new symptoms, and PCR tests in particular have only gotten harder to access since early 2022.
Second, this analysis focused on people who had new symptoms after COVID-19—and excluded people who had existing symptoms that might overlap with Long COVID before they got hit by COVID-19. This focus leaves out people with preexisting conditions (i.e. other chronic diseases), who tend to be at higher risk for Long COVID. Epidemiologist Deepti Gurdasani has a helpful Twitter thread explaining this issue in detail:
Meanwhile, the Slate piece dismisses Long COVID, arguing that the condition is “neither as common nor as severe” as experts have warned it might become. Like the Washington Post piece, this article bases its conclusion on flawed research that focuses on biased health records, and other types of biased data. For example, the author argues that people aren’t getting social security disability benefits in large numbers; but Long COVID patients face many barriers to this program, as I’ve covered for KHN.
The Slate article fails to cite Long COVID patients or experts who have cared for those patients. It also fails to include extensive research showing that Long COVID can mean lasting damage to many organ systems. In fact, Slate issued a correction to the piece shortly after it was published, explaining that, yes, research has “identified biological changes” associated with Long COVID. (The author initially wrote that there were “no biomarkers” for Long COVID.)
I’ve signed onto a letter demanding that Slate retract this article, along with hundreds of other journalists, researchers, and clinicians with Long COVID expertise. You can read it and consider signing here.
These two articles fall into a similar trap: they cherry-pick evidence to suggest that Long COVID might not be as common as some experts and patient-advocates say it is. But they ignore substantial evidence showing how widespread and how damaging the condition actually is. And furthermore, even if Long COVID is getting “milder” or “rarer” with Omicron, so many people have been infected by it (and by prior variants) that there are still millions out there who need help. Arguing over prevalence distracts from the true story: people are suffering, and they need support.
It’s important to note that the majority of journalists covering Long COVID are doing so in good faith, simply trying to understand a complex and confusing condition. But it can be easy to make mistakes (like citing the wrong evidence, or failing to talk to a person with Long COVID). Plus, some bad actors have shown up in the media again and again; the author of the Slate article, for example, previously wrote a highly discredited story for New York Magazine.
For other journalists covering this topic, I’m always happy to help answer questions or point folks to resources. The tipsheet I compiled for NICAR might be a good place to start. And for editors assigning these stories: please make sure you’re giving assignments to a credible writer.
More Long COVID data
-
Sources and updates, March 12
- COVID-19 polling data from Axios/Ipsos: During the workshop I led at NICAR last weekend, one attendee (who works at the market research company Ipsos) recommended that journalists and researchers interested in Long COVID data should check out the Axios/Ipsos polling project to track American attitudes on COVID-19. Recent iterations of the poll have included questions about Long COVID, and the polling results are broken out by demographics (age, race, houeshold income). The surveys ask many other COVID-19 questions as well, such as attitudes about masking. To access the data, you can download PDFs from the Ipsos site or spreadsheets from Roper.
- CDC provides guidance for Long COVID deaths: The CDC National Center for Health Statistics has started to add information about Long COVID to its guidance for death certificates, following a report that the agency published in December about deaths from Long COVID. The guidance now explains that SARS-CoV-2 “can have lasting effects on nearly every organ and organ system of the body weeks, months, and potentially years after infection,” and can contribute to premature death months or years after a patient’s original infection. For context, see MuckRock’s report on Long COVID deaths from December.
- Long COVID gastrointestinal symptoms: Ziyad Al-Aly and his team at the Veterans Affairs St. Louis Health Care System have a new paper in Nature about long-term gastrointestinal symptoms following COVID-19. Using the VA electronic health records database, the researchers compared 150,000 people who’d had COVID-19 to millions of controls. They found people with COVID-19 had elevated risks of many gastrointestinal disorders (including acid-related illness, intestinal disorders, pancreatitis, and more) in the year following their acute cases, compared to the controls. GI symptoms have long been an under-publicized aspect of COVID-19 and Long COVID.
- Clinical trial for Long COVID shows promising results: And one more Long COVID study: researchers at the University of Minnesota examined the potential for three common medications to lower risk of Long COVID. This study was a blinded, randomized control trial—the gold standard of medical research. One of the drugs tested, metformin (which is a common medication for type 2 diabetes), led to a significantly lower risk of Long COVID compared to the placebo. The study hasn’t yet been peer-reviewed, but it shows promising results for metformin as a potential Long COVID treatment option.
- Examining trust in public health agencies: Another new paper, published this week in Health Affairs, shares results from a survey of about 4,200 U.S. adults (a nationally representative sample) about trust in public health agencies. The survey suggested that trust in federal agencies is connected to perceptions of scientific expertise, while trust in state and local agencies is more tied to “perceptions of hard work, compassionate policy, and direct services.” Survey respondents who reported the least trust in public health cied concerns about political influence, private sector influence, inconsistency, and excessive restrictions.
- Some parents lied about children’s COVID-19 status: One more notable survey study, published this week in JAMA Network Open: researchers at Middlesex Community College (in Connecticut) and University of Utah Health, among other collaborators, surveyed a group of 1,700 U.S. parents about COVID-19 protective measures for their children. The study found about 26% of respondents reported lying about or misrepresenting their child’s COVID-19 status in order to break quarantine rules. Common motivations for this behavior were wanting to “exercise personal freedom as a parent,” not being able to miss work or other responsibilities, and wanting kids to have normal experiences. The results suggest “a serious public health challenge” for continued COVID-19 outbreaks and other infectious diseases, the paper’s authors write.
- Maternal mortality during the pandemic: MuckRock (where I work part-time) has published new analysis showing a significant increase in maternal deaths during the COVID-19 pandemic, based on CDC mortality data. The death rate for women ages 15 to 44 went from about 29 deaths per 100,000 births in 2019 to 46 deaths per 100,000 births in 2021. Death rates were significantly higher for Black women and in states with more restrictive policies on maternal healthcare. You can find the full analysis (including a selection of state-level data) here.
-
Remission Biome could represent a new paradigm in patient-led research
Screenshot of the Remission Biome website. I have a new story out in National Geographic this week about a growing area of research connecting the gut microbiome—the diverse community of microorganisms that live in our digestive systems—with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), the chronic disease that often occurs after viral infection and has many commonalities with Long COVID. (Here’s a non-paywalled link to the story.)
Two recent papers, both funded by the National Institutes of Health, point to specific differences between the gut ecosystems of ME/CFS patients and those of healthy controls. The new studies built on previous research in this area, but utilized larger patient cohorts than typical ME/CFS studies. Their findings provide avenues for better diagnosing and treating ME/CFS patients, as well as people with Long COVID who meet the criteria for ME/CFS. (Some studies suggest about half of Long COVID patients fall into this category.)
Continued gut microbiome research could identify specific bacterial supplements that help alleviate ME/CFS symptoms, along with new drugs that target specific changes in these patients’ metabolisms and immune systems. But many people with ME/CFS and Long COVID aren’t waiting for the clinical trials; they’re experimenting with the supplement and diet changes that are already available.
One big project in this realm is Remission Biome, a study by two ME/CFS patients who were working scientists before their symptoms became disabling. Patient-researchers Tamara Romanuk and Tess Falor both have experienced “remission events,” in which their ME/CFS symptoms faded after taking bacterial supplements. When they met on Twitter, they started a project attempting to recreate those events—but it quickly grew into a much larger effort to understand how the microbiome interests with post-viral illness symptoms.
I talked to Romanuk and Falor for my National Geographic story. We discussed how to design a study in which the scientists are also the patients, how their project builds on big data in microbiome research, communicating with the patient community, future plans for Remission Biome, and more. Since most of the conversation didn’t make it into my story, I wanted to share it here.
This interview has been lightly edited and condensed for clarity.
Betsy Ladyzhets: I wanted to start by asking how you all came to do this project, specifically replicating remission events that you’d experienced in the past, and how that intersects with other research that’s been done in this area of ME/CFS and the microbiome.
Tamara Romanuk: I had always been planning on trying to replicate the event… It had been in my mind constantly to try to recreate the experience. I actually did, at one point, take another course of amoxicillin [an antibiotic] but I didn’t do anything else. I didn’t do the probiotics. I didn’t do the sort of the full suite that I was that we’re proposing here [in the Remission Biome protocol].
So, it’s something I would have come to on my own regardless. But when I met Tess and she told me that she had had a similar event, it seemed like, okay, this was something we were probably going to do in the future together. It was just a matter of when. I think we must have talked about it even within the first weeks of meeting each other.
Tess Falor: It was, 10 days [after we met]… I had an interesting experience, in that that I didn’t realize that it was the antibiotics that might have done this [alleviated symptoms]. So back when I had my event in 2009, I went gluten-free and started the antibiotics at the same time. And two days later, after I had my major remission, I accidentally ate gluten. And then I felt worse the next day. So for 13 years, I’ve been assuming that it was going gluten-free that made the difference. And I never consider that I could recreate it because I’ve been gluten for that whole time.
It wasn’t until I met Tamara last fall that I realized that, wow, this [remission event] actually could have been the antibiotics. So when that came up, then, Tamara had this idea to try to recreate it. If it was actually the antibiotics that did it, could we create this really extreme remission event?
BL: I see. In terms of identifying the antibiotics, the probiotics, and the other treatments that you’re using in this study, how did you arrive at this protocol that y’all are following?
TR: Yeah, great question. When we decided to recreate it, the plan started as, “let’s take the antibiotics, and let’s throw in some probiotics, and let’s see what happens.” But we’re scientists, so it morphed very, very quickly into something much, much bigger.
Where Tess and I went in our minds was directly to the theory and the models that would have given rise to a phenomenon like this. Instead of starting at a protocol, we went, “this is our pet theory [about why remission occurred], and if our pet theory is right, how do we work backwards and recreate the protocol?” One of the really interesting things about doing it from that angle was that most of the stuff that I had initially thought I would include I actually threw out very, very quickly. The probiotic that I thought we were almost for sure going to use has ended up being, “oh, that actually might have stopped my event from continuing rather than promoting it.”
And we’re working in an age where there’s some really new cutting-edge databases and information sources out there. I wouldn’t have actually been able to do this type of protocol development a few years ago, even. [For example], we knew that we wanted to manipulate tryptophan metabolites in the gut. And so we needed to find strains of bacteria that were involved in tryptophan metabolism. And then we also knew that we wanted really specific metabolites to be produced in the gut and get to the brain. We were able to go into a database and actually follow that chain, identify specific strains of bacteria that would do exactly what we wanted in terms of gut and brain metabolites, and then trace it back to probiotic manufacturers. That’s pretty phenomenal. And that wouldn’t have been possible two years ago.
BL: Yeah, that’s incredible that you could just follow it all the way through like that.
TF: Absolutely. I’ll also mention that we’ve gotten advice from experts, too. Three people who study the microbiome gave us specific advice, and it all kind of converged in the same ideas, the same strains. So that was cool, too.
BL: Actually, it’s interesting that you mentioned tryptophan, because that was one of the processes identified in the recent papers [the two studies that were the focus of my National Geographic story] as well. I think the main one they looked at was butyrate.
TF: Yeah, those are both things that we are thinking about as part of our hypotheses. When those papers came out, we were like, “wow, this is really cool timing.” We read the papers, and found [their findings] line up with what we’re thinking. And we’ve already been thinking about this for months.
TR: There’s a really neat tie-in here in terms of the tryptophan metabolism. Because initially, my theory had been surrounding Robert Phair’s idea of the “Metabolic Trap,” which is, of course dependent on tryptophan. But the [remission] event itself was also incredibly unique because it was a bit psychedelic. Colors were brighter, smells were smellier, the world was amazing, we felt overwhelming gratitude. I tell people that it was a little bit like a mix between doing MDMA and psilocybin mushrooms. But without the hallucination. It was just this overwhelming change in my mood.
So I was thinking about tryptophan, serotonin, the same receptors that might actually get activated during a psychedelic trip. It really seemed that this entire pathway—from tryptophan to serotonin, to some good and some bad molecules like kynurenine, which can be both pro- and anti-inflammatory, and then quinolinic acid, which is absolutely pro-inflammatory in the brain. When you start at tryptophan, you keep going along this pathway, and whatever path it ends up following, you get different neurotransmitter activity going on. [The remission] was a microbiome event, but it’s really a microbiome-mediated event that’s occurring in the brain.
BL: That makes sense, yeah. Because it’s the microbiome that impacts these metabolic processes that then impact what’s happening in the brain, right?
TR: Absolutely.
BL: In terms of tracking what happens when you do this protocol, what are you using to study the changes in your gut and the further progression that you were talking about?
TF: Tamara knows more details than I do, but I’ll just say we are measuring a ton of biomarkers. Everything from specific composition of the gut, to measures of the immune system, like cytokines, and measures of what’s going on in the brain.
TR: We probably have about a thousand metabolites that we’re gonna track. When you consider that we’re doing a lot of these pre[-trial], hopefully during as well as post, it really adds up. It’s actually one of the most exciting parts about the project, for Tess and I. We both have an explicitly systems thinking approach to science, and we love big data. This is something that actually really excites us, we’re going to be able to really dig in.
All of these tests really work in concert as well. The immunogenetics angles are really key for us. And Tess and I have some unique, similar genetic backgrounds, so that’s going to tie in. Then tracking neurotransmitters: actually tracking tryptophan, tracking serotonin, tracking kynurenic acid and quinolinic acid, as well as their ratios. And all of these metabolites.
BL: I see. Yeah, I feel like that will be really interesting to look at all the interactions between these different things. I know you mentioned that you’ve consulted with folks on the protocols, are there other things that you’re doing to maintain the safety of the experiment?
TR: Absolutely. So we’re working with one of my personal GPs [general practitioners], and she’s kind of acting as our GP safety liaison. She will be on hand if anything strange happens. But really what we’re doing in terms of safety is we’re testing ahead of time. We’re making sure we don’t have leaky gut, we’re making sure we don’t have a compromised blood-brain barrier, or making sure that we don’t have certain pathogenic bacteria in our system that could explode if they weren’t affected by the amoxicillin—and lead to a massive, very adverse reaction.
The main tests we’re doing there is from a company called Cyrex, they do these amazing immune tests… And then we’re doing tests like the GI effects from Genova, which will actually tell us if we have high levels of any pathogenic or potentially-pathogenic bacteria in our guts, before we actually start. If any of [certain concerning biomarkers] turn up as being really high for one of us, then we will take some time out, try to correct that specific defect and then proceed again.
BL: That makes sense.
TF: We do have a clinician who has a lot of experience with these specific tests, and specifically with the gut, who’s helping us. In addition to Tamara realizing it was a good idea to do all this pre-testing, she recommended it, too. So she can take a look at our results, and give us her perspective.
TR: One of the things we want to do there is, we want to actually figure out a very simplified testing protocol, which we can suggest to people to do for themselves before they do this [experimenting with supplements]. Because we want to actually bring this work to people who really need it, but we also want to make sure they’re safe. Hopefully, all of the testing that we do will help us arrive at a couple of biomarkers, which we can then tell people, “Look, if you test these one or two or three things, then you can do this without worrying so much about having side effects or adverse consequences.”
Right now, it would cost the regular person probably about $2,000 to test everything that we’re testing, in terms of making sure all these levels are safe. We want to figure out a way to decrease that cost, break that down into specific biomarkers. And then, hopefully, when we move into our Phase Two of Remission Biome—which is actually bringing this work to the patient population—we might even be able to give people these tests, or at least provide them with very significant discounts for these tests.
BL: Yeah, that’s something I wanted to ask you more about, too, is how you have been communicating with other people who want to try this sort of thing. I know from following y’all on Twitter and seeing some of the discussion around this project that folks are so interested. And generally, of course, there’s a big interest among people with Long COVID, ME, other similar conditions just trying to see what would work while there are no official FDA-approved treatments.
How have you found that experience? And, as you look towards Phase Two, what are some of the things you’re going to be thinking about, in bringing these results to other people?
TF: I’ve been talking to people on Twitter. And I would say, we’ve mostly been recommending, “wait until we do this first experiment, so that we can learn from it.” But for people who happen to be getting prescribed antibiotics [for an infection or something similar], then they have their doctor watching them. In that case, we can say, “you want to protect your gut, here are the probiotics that we’re doing, and you might possibly want to do a biome site test while working with your doctor.”
TR: We have had such an overwhelming response. I think hundreds of people must have contacted you [Tess] personally now with a story that they thought might be a revision event, like the one that we’re describing. And hundreds more have said that they’ve had some sort of a positive or negative reaction to antibiotics. And they’ve had ME/CFS, or Long COVID. Those stories are really the jumping-off point for us. We want to put together a very formal survey to actually figure out how people are responding to antibiotics in post-viral illness, in general. There are a lot of clues in people’s stories.
And the response of our community has been almost overwhelmingly positive, but there have been a few people who’ve had pretty severe baseline decreases after taking antibiotics. It’s always hard to know if the antibiotic itself was responsible for that decline or something else. But we really want to delve into that and figure out whether there’s a subset of people that seem to be having negative reactions.
BL: I also wanted to ask about communicating the results from this work. What are you thinking about in terms of both sharing with other people in the community, and also, are you looking towards like a preprint, or scientific publication?
TF: Yeah, we’ll be communicating in real-time with the community on Twitter, and getting input from all the scientists that we’ve talked to. That’s also something that we didn’t really mention yet is, we’ve talked to over 20 different researchers and gotten input from them. We have some that are interested in analyzing our results afterward. So, there’s community communication, but we are also planning to publish it, at least as a preprint.
TR: We’re going to be a great case study. And it’s going to be a great paper. It’s not going to end up in a formal journal, but we’ll definitely pop it into one of the preprint servers.
In addition to the case study, though, we really want to do a meta-analysis. A formal meta-analysis of all the studies that have ever looked at antibiotic use and post-viral illness. We think there are a lot of clues there. One of the things that’s really fascinating to us about this is that there are a number of similar situations that have happened in other conditions. One of the really key ones is PANS, or PANDAS, which often occurs in children when they get a staph infection—and then they get this crazy neurological event where their behavior changes and they develop OCD. Well, turns out, in an enormous number of those cases, if you give them antibiotics of the right type quickly enough—and a lot of the time, it’s amoxicillin plus minocycline, or doxycycline—you can actually completely put that child into remission.
And there’s other disease groupings that seem to have these remission events, in very similar ways. Even Alzheimer’s, many people who have a grandparent with Alzheimer’s will tell stories of moments of complete lucidity. This indicates that maybe brain damage isn’t the ultimate issue, maybe there’s something going on with the communication networks. And that’s really what we’re targeting here [in our research].
BL: That’s really interesting. I was actually just talking to another researcher for this story [Sonia Villapol at Houston Methodist Hospital], who mentioned that her lab, where she is studying Long COVID and the microbiome, has also done work on Alzheimer’s, and even traumatic brain injuries, where there’s some kind of microbiome interaction. I thought that was really interesting. It definitely seems like there’s so much more to be explored here.
TF: Yeah, one of the researchers that we talked to is also doing ME/CFS and Long COVID research, and then Parkinson’s—using probiotics for Parkinson’s. I think a lot of what we’re doing can apply to other conditions, too.
BL: Right. I also wanted to ask if y’all had any other comments about the two recent studies?
TR: Well, I was pretty excited to see butyrate as sort of the highlight molecule. Very early on, we decided that we were going to try to increase our butyrate levels… So we were really excited to see that both of those papers linked to butyrate-producing bacteria, which was really key for us. It’s not just that we want to increase butyrate during the experiment itself, but it’s also a great way to actually help heal leaky gut issues. So it’s a really great intervention.
BL: Yeah, that’s something that has come up a lot in the research I’ve done for this piece—the value of intervening early and trying to help people out before they’re going to have long-term symptoms, or at least in the earlier stages of illness. Which I know is one of the reasons why there’s so much interest in Long COVID, because you’re ideally diagnosing people earlier than what’s historically been the case for ME and some of these other related conditions.
TR: To me, the really exciting application of this is that antibiotics are a very safe intervention that have been used for dozens of years. If it turns out that there’s a chance that taking a quick course of amoxicillin and a tetracycline like minocycline or doxycycline, can take someone who might have developed much more severe Long COVID and then MECFS out of that track, well, that’s phenomenal. If there was actually something that you could go to your doctor and say, “hey, I’m having these Long COVID symptoms, what can we do right now?” And the answer is, “well, it’s pretty safe, why not just give you a week’s worth of antibiotics?” It’s a pretty exciting possibility that we could stop some of these more severe cases.
BL: Yeah, absolutely. I also wanted to ask, in terms of the institutional side of this, what do you think the NIH and other government agencies could be doing to better support this kind of work, and integrating ME/CFS and Long COVID research, as we try to understand the common mechanisms here?
TR: Well, they could actually be treating us. This is really the biggest roadblock: there are hundreds of thousands of people out there who are undiagnosed and untreated, and are trying to biohack their way out of serious post-viral illness. None of these people are seeing clinicians that know what they’re talking about. So, we need treatment centers—but not just the Long COVID treatment centers, where they just tell people to rest, but centers that actually do biochemical testing, figure out what’s actually going on in their bodies, and then doing targeted treatment.
Even if you can’t cure ME/CFS right now, it doesn’t mean that you can’t help people feel phenomenally better, and make sure that they don’t slide from moderate into severe. What you said before is so key, because most of us slide from moderate to severe when we get comorbidities. When we get MCAS on top of the Long COVID, for example. All of these comorbidities compound, and then they get people to a state where almost any intervention is aggravating to their systems, and they literally can’t tolerate light or sound or food. Treating someone at that stage is almost impossible, unfortunately, at this point. So early intervention is really key—but to get early intervention, you need clinicians that know what they’re doing interacting with patients.
BL: Which we don’t have nearly enough of.
TF: Yeah, that’s a major problem. Another angle that I’ll mention is more funding for research, specifically for ME/CFS. There are a lot of really great ME/CFS scientists who haven’t been able to get funding, but they’ve been trying to study this for decades. I keep hearing people saying that there’s these new researchers coming into Long COVID, who don’t really understand a lot about the history and what’s already been done. I think we need more funding for ME/CFS research, plus particularly funding for people who have been doing this for a long time.
TR: Absolutely. One of the things that Tess and I are really excited about is—I guess what we’re going to be calling Phase Three, but it’s starting now—is we’re putting together a hybrid DAO, plus a nonprofit, to actually provide funding for researchers in this area. It’s not just for researchers, it’s specifically for PhD patients.
We really want to tap into this community of sick scientists who’ve been sidelined by ME/CFS, by COVID, by other disabilities, and offer them the chance to actually get back into research in a way that they could do and would be supported. We’re really seeing a new model, a new way of being able to conduct research that is outside of academia, yet has checks and balances and support. Remission Biome has been, hands down, the best thing for my mental health that has happened in 10 years. If I could bring little bit of that to other people in my position—that’s what I would like.
TF: We’ve actually had a lot of people volunteer to help. And I’ve gotten the comment many times, people saying, “this feels so good to use my expertise again.” These are people that have been on disability for 10 years and haven’t been able to do any work or any research. And now they’re able to give their expertise towards our project, and help us gain momentum and move forward, and they’re just really happy about it. I think there’s so much untapped expertise out there.
BL: Yeah, that makes so much sense. And I hope I can keep following this project as y’all expand it.
More on Long COVID
-
Sources and updates, March 5
- FDA authorizes joint COVID/flu rapid test, but there’s a catch: Late last week, the FDA issued emergency use authorization to the U.S.’s first at-home, rapid test capable of detecting both COVID-19 and the flu. This could be a really useful tool for people experiencing respiratory symptoms, since COVID-19 and flu can appear so similar. But you might not be seeing this test on pharmacy shelves anytime soon: Lucira Health, the test’s manufacturer, just declared bankruptcy. And the company actually blamed FDA authorization delays for contributing to its financial situation, as it had produced supplies anticipating a fall/winter sale of tests. Brittany Trang at STAT News reported on the situation; read her story for more details.
- COVID-19 surveillance stressed out essential workers: For a new report, the nonprofit Data & Society interviewed 50 essential workers from meatpacking and food processing, warehousing, manufacturing, and grocery retail industries about their experiences with COVID-19 surveillance efforts, like temperature checks and proximity monitoring. Overall, workers found that these surveillance measures added time and stress to the job but did not actually provide information about COVID-19 spread in their workplaces. (Companies often cited privacy concerns as a reason not to share when someone got sick, according to the report.) The report shows how health data often doesn’t make it back to the people most impacted by its collection.
- Vaccinations vs. Long COVID meta-analysis: A new paper published this week in the BMJ examines how COVID-19 vaccination impacts Long COVID risk. The researchers (at Bond University in Australia) performed a meta-analysis, compiling results from 16 prior studies. While the studies overall showed that vaccination can decrease risk of getting Long COVID after an infection (and may reduce symptoms for patients already sick with Long COVID), the studies were too different in their methodologies to actually allow for “any meaningful meta-analysis,” the authors noted. To better study this question, more rigorous clinical trials are needed, the researchers wrote.
- Tracking Long COVID with insurance data: Another notable Long COVID paper, published this week in JAMA Health Forum: researchers at the insurance company Elevance Health compared health outcomes for about 13,000 people with post-COVID symptoms compared to 27,000 who did not have symptoms. The researchers found that, in the one year following acute COVID-19, Long COVID patients had higher risks for several health outcomes, including strokes, heart failure, asthma, and COPD; people in the post-COVID cohort were also more likely to die in that year-long period. I expect insurance databases like the one used in this paper may become more common Long COVID data sources. Also, see Eric Topol’s Substack for commentary.
- FDA committee recommends RSV vaccine applications: Finally, a bit of good news on the “other respiratory viruses” front: the FDA’s vaccine advisory committee has recommended the agency move forward with two applications for RSV vaccines. Major pharmaceutical companies Pfizer and GlaxoSmithKline (GSK) have been working on RSV vaccine options; while early data appear promising, clinical trials on both vaccines have found potentially concerning safety signals. The trial populations have been relatively small, making these signals difficult to interpret right now but worthy of additional study. As usual, Katelyn Jetelina at Your Local Epidemiologist has provided a great summary of the FDA advisory committee meeting.
-
My tips for covering Long COVID (using data, records, and patient interviews)

Cover slide from my workshop at NICAR this weekend. On Friday, I led a workshop at NICAR about covering Long COVID. NICAR is a data journalism conference—the acronym stands for National Institute for Computer-Assisted Reporting, which is an old-school term for data journalism—so my session focused on data sources, along with suggestions for public records requests and for interviewing long-haulers.
My main goal for the workshop was to introduce Long COVID as a worthwhile coverage topic for journalists who aren’t already on the science or health beat. Plenty of science/health reporters (like myself) have written great articles about biomedical research, patient experiences, and other similar topics. But there are many other facets of Long COVID, ranging from its impact on work to the public agencies that should be held accountable for failing to address this crisis.
To that end, I spent part of the session talking about excellent Long COVID articles that don’t focus on science/health topics. I also gave attendees a prompt to brainstorm story ideas for their beats or coverage areas. This led to some interesting conversations about potential local stories on Long COVID clinics, Household Pulse Survey data, tracking disability applications, and more.
If you’re curious to see more of what I shared from the session: here’s a link to the tipsheet I compiled, and here’s a link to my slides.
Also: as I’ve mentioned previously, I am currently leading a project at MuckRock (where I work part-time) to investigate U.S. government responses to Long COVID. For any journalists who may be interested in collaborating with MuckRock on Long COVID or other public health topics, you can reach out to us here.
More Long COVID coverage
-
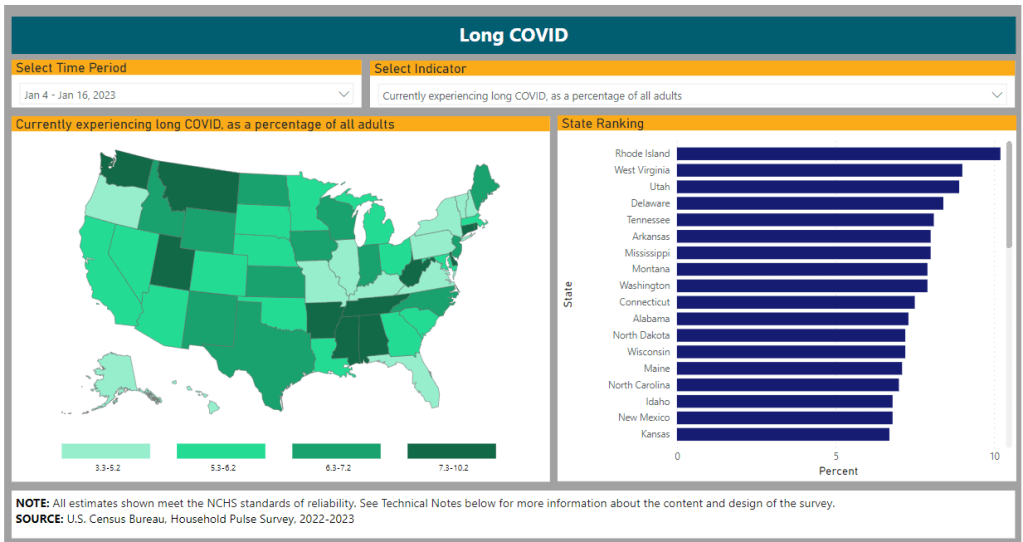
How researchers track Long COVID’s impacts
The Census and CDC’s Household Pulse Survey provides one major source of data on Long COVID prevalence. I got an interesting question from a reader last weekend, asking if excess deaths might be one way to identify the impact of Long COVID. It’s an interesting idea: could the numbers of deaths from medical causes above what researchers expect in a given timeframe indicate some premature deaths tied to Long COVID?
Based on my previous work with excess deaths (see MuckRock’s Uncounted project), I think this could be possible, though it’d likely be very hard to identify direct relationships between Long COVID and specific deaths. As far as I know, no researchers are working on this question; if you know of anyone who is, please reach out.
Still, the reader’s question got me thinking about how, exactly, we track the impacts of Long COVID. Doctors, researchers, and long-haulers themselves have learned a lot about the condition over the last three years. We still don’t have clear estimates of exactly how many people in the U.S. are dealing with this chronic disease, but we’ve come much closer to understanding its impacts than we were when patients first began advocating for themselves in 2020.
Tracking Long COVID is challenging because of uneven access to COVID-19 tests and to medical care, which means long-haulers with certain types of privilege are more likely to get an accurate diagnosis. A lack of knowledge about Long COVID, both among medical professionals and among the overall population of people who might get it, also contributes to this issue. (For more details, see this post from early December.)
Still, some strategies have emerged for identifying people with Long COVID and tracking how the condition is impacting them. Here are a few.
Following people who were hospitalized for COVID-19:
In this strategy, researchers identify people who had COVID-19 and track how the virus impacts them over time. It’s often easiest for researchers to track people who were hospitalized, since hospitals keep detailed medical records of their patients, though this tactic leaves out long-haulers who initially had mild cases.
Sometimes, researchers doing this type of follow-up study will directly survey COVID-19 patients, which can lead to more comprehensive data than using health records alone. One recent study in this category found that, among a group of 800 adults hospitalized for COVID-19, about half were still experiencing some financial issues and limitations in their ability to do day-to-day activities six months later. The study’s authors noted that financial issues were “reported more frequently” among patients who identified with demographic minorities.
Following COVID-positive patients through electronic health records:
In other studies, researchers use electronic health records to identify how people who had COVID-19 fare months later. Two recent studies associated with the National Institutes of Health’s RECOVER initiative fall into this category. One paper utilized records from New York City health centers, and found that Black and Hispanic adults were more likely to have potentially Long COVID-related health issues following a COVID-19 case. The other paper, which used records from 34 medical centers across the U.S., found that white, female, non-Hispanic patients living in areas with greater healthcare access were more likely to receive an actual Long COVID diagnosis.
Angela Vázquez, president of the Long COVID group Body Politic, summarized the two new studies succinctly on Twitter, writing: “Black and Hispanic Americans appear to experience more symptoms and health problems related to #LongCovid than white people, but are not as likely to be diagnosed with the condition.” Vázquez also pointed out that the studies may have missed neurological symptoms among Black and Hispanic patients, due to less access to care for these groups.
Broad surveys of potential patients:
Electronic health records are far from perfect sources of Long COVID data, as they often present only sets of information that doctors are already compiling—and they are often biased towards the people who are able to access medical care for COVID-19 (or Long COVID) in the first place. As a result, some researchers track Long COVID through broader surveys, seeking to identify everyone who might have some long-term symptoms following a COVID-19 case, even if those people might not be calling their condition “Long COVID.”
The Census and CDC’s Household Pulse Survey questions on Long COVID are one notable example of this strategy. Census researchers ask a random sample of Americans whether they’ve had “any symptoms lasting 3 months or longer” following a COVID-19 case, then follow up with questions about whether those symptoms are current and whether they impact the respondent’s ability to carry out day-to-day activities. The resulting data provide a broader view of Long COVID in the U.S., including people who may not have sought medical care for their symptoms.
Biological studies of specific organs impacted by COVID-19:
In order to better understand how a case of COVID-19 may lead to long-term, debilitating symptoms, some researchers focus on studying exactly what happens to different parts of the body after a coronavirus infection. This research sometimes focuses on testing for the continued presence of virus after a patient’s acute COVID-19 case is over or tracking changes to the immune system, as scientists test different theories into how Long COVID occurs.
One major area of research has been the brain. Freelance journalist Stephani Sutherland recently published a major feature in Scientific American exploring how Long COVID impacts the brain and nervous system, summarizing research into the biological causes of common symptoms like fatigue and brain fog. Physician E. Wesley Ely, who cares for Long COVID patients, wrote an essay on the same topic that appeared in STAT News this week; Ely discussed what he’s learned from autopsy studies examining the brains of people who had COVID-19.
Identifying trends in the labor market:
Finally, researchers often seek to track the impacts of Long COVID indirectly, by looking at statistics on people who have left the labor market during recent years. It’s no secret that a lot of people have left their jobs during the pandemic; Long COVID experts argue that the chronic disease may be one major driver of the labor shortage. One often-cited Brookings Institution analysis suggested two to four million people may be out of work due to Long COVID.
This strategy for studying Long COVID may be the most difficult, as it’s hard to actually tie job loss numbers to the condition without more specific data. Most research surveys or electronic health records databases don’t ask people about their work situations; the recent study cited above is a notable outlier. Similarly, most unemployment claims and short-term disability datasets don’t ask people if Long COVID is contributing to their need for assistance.
Still, I hope to see more studies in the future that examine Long COVID’s impact on work and other activities. Related: the U.S. Department of Labor recently published a report about the need for more assistance geared toward workers with Long COVID.
More Long COVID data
-
This winter’s COVID-19 surge wasn’t “mild”

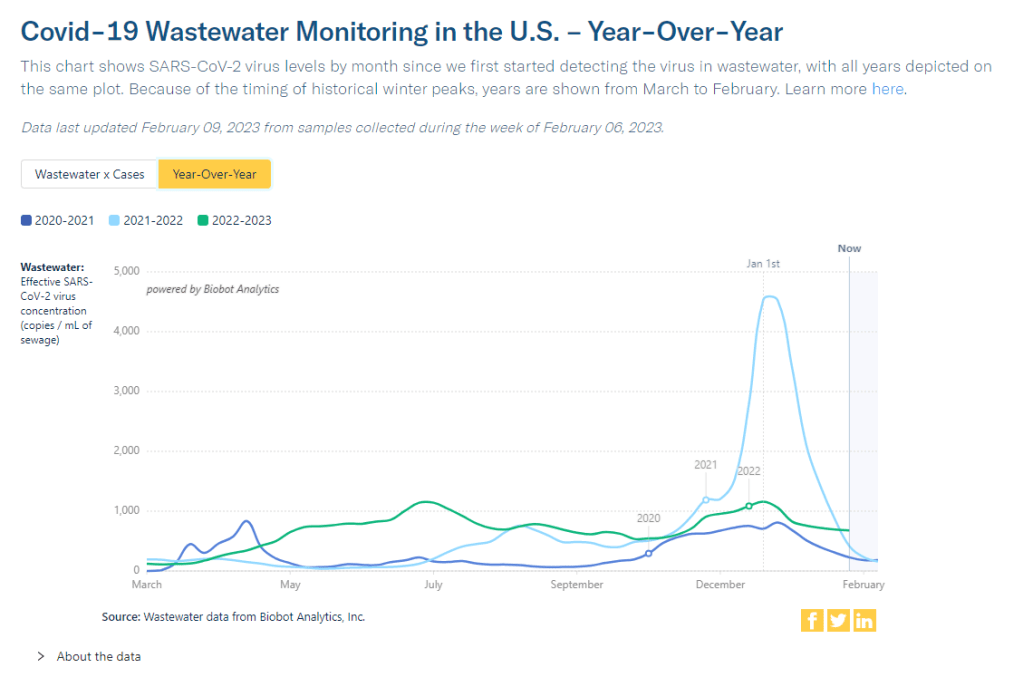
Wastewater surveillance data from Biobot suggests that COVID-19 spread this winter (2022-2023) was higher than all other surges prior to Omicron’s emergence. You might have seen some headlines like this in the last few weeks: COVID-19 was “mild” this winter. This winter was “better” than previous winters. COVID-19 is becoming “another seasonal virus” like flu and RSV. But is this true?
While it’s accurate that the U.S. reported fewer COVID-19 cases this past winter compared to last year (when the country experienced our first, massive Omicron surge) or the prior year (our biggest surge pre-vaccines), this winter still saw an extraordinary amount of severe illness, death, and potential future disability due to COVID-19. Surges of other respiratory viruses also put enormous strain on the healthcare system.
If we call this winter “mild,” we run the risk of believing this level of disease is acceptable. Such portrayals of COVID-19 seek to make us think future surges will be nothing to worry about, despite clear evidence to the contrary.
Let’s go through some numbers. Since the beginning of November, the U.S. has reported:
- More than 5 million new COVID-19 cases (reported). Note that cases are likely underreported by 10 to 20 times in our era of under-testing, so the true number may be closer to 100 million.
- More than 400,000 new COVID-19 hospitalizations, piling on top of hospitalizations for the flu, RSV, and other diseases, and coming as hospitals deal with staff shortages and worker burnout.
- More than 40,000 new COVID-19 deaths, amounting to more than 400 new deaths per day. This number is also likely an undercount, as death certificates can take a long time to be processed.
- The majority of COVID-19 deaths were among vaccinated people. A report from the Kaiser Family Foundation found that breakthrough deaths started to outnumber those among unvaccinated people in summer 2022, a trend that has continued with low booster uptake.
- Coronavirus levels in wastewater were higher than all surges prior to Omicron, including the winter surge in 2020-2021 and the Delta surge in summer 2021, according to data from Biobot.
- XBB.1.5, the latest and most contagious Omicron subvariant, evolved in the U.S. this winter, likely in New York State. Unchecked COVID-19 spread makes it easier for the virus to keep mutating.
- More than 5% of American adults are currently experiencing Long COVID. This number has ranged from 5.5% to 7% since September 2022, according to the CDC and Census’ Household Pulse Survey.
- Almost 80% of adults with Long COVID report activity limitations due to the condition, including about 25% who report “significant” activity limitations, per the Household Pulse Survey.
In an average week this winter, the U.S. reported more deaths from COVID-19 than the number of casualties on September 11, 2001. The latter event was a horrific tragedy that inspired lasting changes to national security, while the former has been written off as “mild.”
Past surveys from many sources—including the CDC itself—have suggested that, when people know COVID-19 is spreading widely in their communities, they’re willing to take basic safety precautions. But when government leaders and mainstream media outlets downplay the risks, people don’t have the information they need to make informed choices. We’ve seen this pattern at a large scale this winter, and I worry that the trend will only continue.
And here’s what concerns me even more: in previous winters, cases went up over the holidays, then declined through January and February. This year, however, the decline isn’t really happening. Transmission has gone down a bit from its peak, but it’s now plateaued at a level higher than the peaks of previous surges, per Biobot’s data.
So, not only did we have a bad surge this winter, we’re now stuck at a high-COVID baseline that seems very difficult to shake, in the era of many new variants and few public health precautions. The situation reminds me of a Twitter thread from the evolutionary biologist T. Ryan Gregory, which I shared when writing about XBB.1.5 in early January:
That “area under the curve” is what the U.S. is seeing now, as COVID-19 spread stays at high levels. Thousands of cases a day, thousands of hospitalizations a day, hundreds of deaths a day.
As a journalist and as an individual capable of taking precautions, I resist the narrative that any of this is acceptable. If you’re reading this, I hope you can, too.
More federal data
-
Sources and updates, January 29
- New York State expands wastewater surveillance program: This week, the New York State health department announced a major investment in the state’s wastewater surveillance program: the program has received a $6.6 million grant from the CDC and $15 million from the governor (over the next three years). With this investment, New York’s wastewater surveillance network will grow from 125 to 215 testing sites and will expand from COVID-19 to include flu, RSV, hepatitis, norovirus, and antimicrobial resistance. This is great news for New York—I hope to see other states make similar investments.
- Bivalent boosters vs. XBB lineages: The bivalent, Omicron-specific booster shots provide some protection against XBB.1.5 and related Omicron subvariants, according to a new study published this week in the CDC’s Morbidity and Mortality Weekly Report. CDC researchers used data from COVID-19 testing at pharmacies to compare results among people who had received the new booster and those who hadn’t. Booster recipients were significantly less likely to have a symptomatic XBB/XBB.1.5 infection compared to people who hadn’t received the shot, the researchers found (with a vaccine effectiveness value of 48%). While the boosters work less well against XBB.1.5 than they did against BA.4/BA.5, they’re still a valuable protective measure.
- CDC overhauling data communications: The CDC is creating new internal offices that will change how it processes, publishes, and communicates about data, according to POLITICO. The new offices include an Office of Health Equity and an Office of Public Health Data, Surveillance, and Technology—both of which have new acting directors as of this week. It’s currently unclear what the new offices will do, exactly, or how they will improve upon a fractured nationwide health data system (with decisions about how to store and share key data largely left up to state agencies and private companies). Still, it’s good to see movement on the CDC’s efforts.
- WHO deliberates ending the global health emergency: On Friday, a World Health Organization committee met to discuss whether the official global health emergency over COVID-19 should be ended. The committee’s decision will be made public tomorrow, as a recommendation to WHO Director-General Tedros Adhanom Ghebreyesus; Tedros will ultimately decide whether or not to end the emergency. Global health experts who spoke to STAT reporter Helen Branswell suggested that the WHO likely isn’t ready to end this emergency yet, but it may happen later in 2023.
- KFF compiles Long COVID data: A new report from the Kaiser Family Foundation compiles and provides context for Long COVID data reported by the Census and CDC’s Household Pulse Survey. The share of people who reported ever having Long COVID symptoms following a COVID-19 case has declined slightly over time, the KFF report finds; this number went from 35% in June 2022 to 28% in January 2023. However, the number is still high and Long COVID can be debilitating for many, as 79% of people with Long COVID report limitations to their day-to-day activities.
- Health of Congressional Districts: Finally: a new dashboard, published this week by researchers at NYU Langone Health, provides detailed health metrics for all 435 Congressional districts in the U.S. (plus Washington, D.C.). The dashboard is a helpful source for researchers and policymakers looking to understand health patterns in specific districts. One of its key metrics is a “COVID Local Risk Index” that reflects the risk residents face for severe health, social, and economic outcomes of COVID-19.