- Grants to help with global pandemic preparedness: This week, the World Bank’s Pandemic Fund announced the recipients of its first round of grants. The fund is a finance initiative to “strengthen pandemic prevention, preparedness, and response capacities,” particularly for low- and middle-income countries. Its first round of grants will go to 37 countries across 6 global regions, distributing $338 million in funding. The full list of awards is available on the World Bank’s website.
- Genetic marker of asymptomatic COVID-19: A new paper published in Nature this week reports on a common genetic marker that may lead people to have symptom-free COVID-19 cases. The researchers (a team from the University of California San Francisco and other institutions) searched for genetic patterns among 30,000 people who shared their COVID-19 symptom information through a smartphone app. They found a correlation between asymptomatic infection and a specific version of a gene related to T cells. As Eric Topol notes in his newsletter, this study follows two others that examined genetic markers of Long COVID.
- Quantifying cognitive symptoms of Long COVID: Speaking of Long COVID: researchers at Kings College London studied the condition’s cognitive symptoms (also called brain fog) by measuring patients’ performance in different mental tasks. The study included over 3,000 participants, more than half of whom completed two rounds of testing over two years. Overall, the researchers found that cognitive symptoms persisted for nearly two years after patients’ initial infections, and most severe for patients with the longest-lasting Long COVID impacts. For these patients, “the effect of COVID-19 on test accuracy was comparable in size to the effect of a 10-year increase in age,” per a press release by Kings College London.
- Long COVID is common in children: Another Long COVID study published this week: researchers at a hospital in Toronto compiled a review paper examining the condition’s prevalence among children. Their review included 30 studies including about 15,000 total pediatric patients. Across all the studies, researchers reported that about 16% of children experienced at least one Long COVID symptom three or more months after their COVID-19 infections. However, compiling these data was a challenging task because different studies used different definitions of Long COVID, different methods of following up with patients over time, and other inconsistencies, the authors wrote.
- Dogs detecting COVID-19 through scent: One more paper that stuck out to me this week: a pair of researchers (one at the University of California, Santa Barbara and one at a biotech company focused on sniffing for COVID-19) examined how well dogs can detect the coronavirus. This was also a review paper, including 29 studies and 31,000 COVID-19 test samples. Overall, the dogs performed with similar accuracy to PCR tests, researchers found. “We believe that scent dogs deserve their place as a serious diagnostic methodology that could be particularly useful during pandemics,” one of the authors said in a statement.
- Monoclonal antibody to protect babies from RSV: Finally, a bit of good news for combatting another common respiratory virus: the FDA has approved a new monoclonal antibody treatment to protect infants and young children against RSV. The therapy is likely to be recommended by the CDC and manufactured in time for respiratory virus season this fall. In clinical trials, it lowered the risk of an RSV infection requiring medical care by about 76%—which is a big deal for a disease that leads to more babies in hospitals than any other in the U.S., reports Helen Branswell at STAT.
Tag: global health
-
Sources and updates, July 23
-
Sources and updates, May 28
- New Long COVID papers from the Patient-Led Research Collaborative: Speaking of new Long COVID research: the Patient-Led Research Collaborative, a group of long-haulers who do and support research on their condition, has recently published two new papers. The first, published in Nature and based on a patient survey, discusses Long COVID’s intersection with common psychiatric conditions such as depression and anxiety. The second, published in Fronteirs in Rehabilitation Science, is a review paper going over the reproductive health impacts of Long COVID. Long COVID frequently causes disruptions to the menstrual cycle, gonad function, fertility, and other areas of reproductive health, yet these symptoms are understudied.
- FDA fully approves Paxlovid: The FDA has provided full approval to Pfizer for its antiviral COVID-19 pill, Paxlovid. Millions of Americans have received Paxlovid since it earned Emergency Use Authorization in late 2021, and many studies have shown that it’s effective in reducing the risk of severe COVID-19 symptoms. With the federal public health emergency’s end, the FDA has encouraged pharmaceutical companies to apply for full approval for their COVID-19 products so that they can permanently remain on the market; Paxlovid is a high-profile example of that trend.
- Bivalent COVID-19 vaccines protect, but wane: The CDC published another study this week evaluating the bivalent (or Omicron-specific) COVID-19 booster shots. These vaccines clearly provide additional protection against severe COVID-19 symptoms, the study finds, but this immune system boost goes away after several months. In the study, vaccine effectiveness against hospitalization declined from 62% in early weeks post-vaccination, to 24% at three to six months post-vaccination. The study shows that additional boosters and/or newer vaccines are needed for vulnerable adults.
- Value of regular testing for controlling outbreaks: Another notable new study: researchers at the University of Wyoming compared how well different mitigation strategies work for preventing the spread of COVID-19 and other diseases, using a model informed by both epidemiological and economic factors. They found that frequent testing—paired with isolation for people who tested positive—was more effective at reducing disease spread than physical distancing measures, like closing businesses or having employees work from home. The paper suggests that testing can help reduce illness while keeping businesses open.
- Funding for a WHO disease surveillance initiative: The Rockefeller Foundation and World Health Organization recently announced a new partnership, with the foundation providing $5 million to support the WHO’s Hub for Pandemic and Epidemic Intelligence. This Hub was established in 2021, with goals including fostering global collaboration on disease surveillance, providing better (and more complete) data, and improving tools for public health decisions. Rockefeller’s support will help with scaling up genomic surveillance, real-time data collection, and more.
-
WHO ends the global health emergency for COVID-19
As the U.S. gears up to end its federal public health emergency for COVID-19, the World Health Organization just declared an end to the global health emergency. WHO Director-General Tedros Adhanom Ghebreyesus announced the declaration on Friday, following a meeting of the organization’s COVID-19 emergency committee the day before.
Here’s what this declaration means, pulling from Helen Branswell’s article in STAT News and Katelyn Jetelina’s Your Local Epidemiologist post:
- The world is at a point of transition from considering COVID-19 an unexpected emergency to considering it a part of our daily lives, a disease that we’ll be dealing with in the long term.
- The WHO will have fewer resources for an international response to COVID-19, such as coordinating between countries and sharing data at a global scale.
- The WHO will also have less authority when it comes to issuing international guidance to control COVID-19 spread.
- There will be fewer incentives for countries to accelerate vaccines, treatments, and tests for COVID-19.
The declaration does not mean that COVID-19 is “over.” We have plenty of long-term issues to deal with here: millions suffering from Long COVID, continued COVID-19 waves around the world, potential new variants, healthcare worker shortages, and declines in childhood vaccination rates, to name a few. Tedros may set up a new committee to make recommendations on long-term COVID-19 management, according to Branswell’s article.
In fact, the WHO recently publicized the impacts of Long COVID: Tedros delivered a PSA explaining that one in ten coronavirus infections leads to some form of Long COVID, and suggesting that “hundreds of millions of people will need longer-term care.” Shifting out of the emergency phase of our global COVID-19 response should be a call to action for scientists and health experts to now focus on Long COVID needs.
Still, a lot of people might interpret the WHO’s declaration as an announcement that they no longer need to worry about COVID-19. Some mainstream publications that have covered the change haven’t done a great job of conveying the nuances here, and I’ve already seen some misinterpretation on social media.
COVID-19 may not be an emergency at this point. But we’re probably going to be living with it for the rest of our lives, and there’s a lot of work left to do.
More on international data
-
Sources and updates, April 23
- External review of the CDC: The People’s CDC, a group of public health experts, scientists, and educators dedicated to advocating for increased COVID-19 precautions, released a new report reviewing the federal CDC’s actins during the pandemic. The report incorporates feedback from a survey of almost 500 experts and from over 200 reports. Overall, the People’s CDC “found that the CDC has prioritized individual choice and short-term business interests over sharing accurate scientific evidence with the public and protecting population health.” (Disclaimer: I was one of the experts surveyed for this report!)
- Use of COVIDTests.gov: This new paper, published in the CDC’s Morbidity and Mortality Weekly Report (MMWR), reports on how Americans used COVIDTests.gov, the USPS/HHS effort to distribute free at-home tests. Since the site’s launch in January 2022, about one in three U.S. households received a test kit from this program, the research team found. They also found that this program may have helped improve equity in COVID-19 test access, as Black and white Americans utilized the free tests at similar rates. Of course, the program has been discontinued as of this spring.
- Impact of racial discrimination on vaccination: Speaking of health equity: another report published in MMWR this week shares a correlation between discrimination and vaccination status. Researchers at the CDC and their collaborators analyzed data from the CDC’s National Immunization Survey, including about 1.2 million survey results from April 2021 through November 2022. Among the respondents, people who reported experiencing racial or ethnic discrimination in a healthcare setting were less likely to be vaccinated for COVID-19. The findings confirm many health experts’ equity concerns from early in the vaccine rollout.
- Declining childhood vaccinations worldwide: Vaccine equity is a concern on the global scale, too. A new report from UNICEF shows that 67 million children worldwide missed at least one vaccination between 2019 and 2021, as healthcare systems were strained. The report also presents new data on global confidence in childhood vaccines: in some countries, this confidence has dropped by up to 44 percentage points. Vaccine confidence only improved in three countries (China, India, and Mexico). “The threat of vaccine hesitancy may be growing,” UNICEF warns.
- Healthcare workers present while sick: One more paper that caught my attention this week: researchers at the Veterans Affairs healthcare system in Boston tracked a cohort of about 4,000 healthcare workers between December 2020 and September 2021. In addition to PCR testing, the workers conducted daily COVID-19 symptom reviews, and received guidance to stay home or leave work if they didn’t feel well. But the researchers found that many workers didn’t actually stay home: among 255 workers who had symptomatic COVID-19 during the study period, almost half reported that they were present, at work, at the time they received a positive test result. The paper indicates why it’s important to keep masks in healthcare settings, even when community cases are lower.
-
Sources and updates, February 5
- CDC warns of risk to immunocompromised people: As of January 2023, there are no longer any monoclonal antibody treatments available for COVID-19, as these treatments do not provide protection against recent versions of Omicron. The no-longer-effective treatments include Evusheld, a drug used as a protective measure (to reduce risk of symptomatic COVID-19 for immunocompromised people. With Evusheld now unavailable, the CDC issued recommendations last week for people who have severely compromised immune systems. Of course, the CDC’s recommendations are largely targeted to individual action; to actually protet this vulnerable group, all Americans would need to follow collective public health measures.
- Modeling COVID-19 as a persistent “endemic“: A recent preprint, from researchers at the drug company Fractal Therapeutics and collaborators, estimates just how challenging it is for people to avoid COVID-19 when the disease is not managed at a societal level. The researchers estimated Americans’ long-term COVID-19 risk based on an epidemiological model incorporating frequent reinfections, and limited individual-level protections. People who are vaccinated but don’t take other measures to reduce their risk of getting COVID-19 “can expect to spend an average of 6 days a year acutely sick with COVID-19 and also incur a 12% risk of long COVID (symptoms lasting more than 3 months),” the researchers write.
- Global COVID-19 vaccination rate: Another new study, published in the CDC’s Morbidity and Mortality Weekly Report, provides an update on global vaccination rates, calculated by researchers at the World Health Organization. According to the WHO team, about 76% of older adults (ages 60 and older) have received a primary series of COVID-19 vaccines. (The study doesn’t report on booster rates, which are likely much lower worldwide.) As the vast majority of COVID-19 deaths worldwide have occurred among this age group, it should be a priority for vaccination, including the primary series and booster doses.
- COVID-19 litigation database: I recently learned about this database of COVID-related legal documents, run by researchers at the University of Trento in Italy. The database aims to publish case documents from around the world reflecting challenges to COVID-19 policies. As of February 4, it includes documents from 1,978 cases, which can be searched by country, year, type of human rights issue, vulnerable group involved, and more.
- Flu vaccine works well this year: A bit of non-COVID good news: this season’s flu vaccine is well-matched to the flu strain currently circulating in North America, according to a recent study from Canadian researchers and public health officials. Receiving a flu shot halved an individual’s risk of a severe flu case that needed medical care, the study found. Flu shots often have an effectiveness below 40%, explained STAT’s Helen Branswell on Twitter, as the vaccines do not always perfectly match up to circulating viral strains. But this year, the shot appears to be working well.
- NYC declares end of mpox epidemic: And one more bit of good news: New York City officials have declared that the city’s epidemic of mpox (formerly called monkeypox) is now over. The city was a hub for mpox transmission last summer and became a center of the U.S. outbreak; but NYC has reported low case numbers since early fall. The federal public health emergency for mpox also recently ended.
-

Russia’s invasion of Ukraine has COVID-19 impacts

While Ukraine’s COVID-19 cases appear to have gone down in recent days, the country is (obviously) not prioritizing COVID-19 reporting during an invasion. Chart via Our World in Data. When Russian troops began attacking Ukraine, the country was just recovering from its worst COVID-19 surge of the pandemic. To state the terrifying obvious: war makes it much harder to control a pandemic.
Here are a few reports on this situation from the past week:
- The New York Times describes Ukraine’s ability to control COVID-19 as “another casualty of Russia’s invasion.” Reporter Adeel Hassan discusses the challenges of controlling disease spread when people are crowding together in shelters, fleeing to refugee camps, and often unable to access masks or other supplies. The crisis in Ukraine will also impact COVID-19 in nearby countries tasked with caring for refugees, Hassan writes.
- In addition to COVID-19, Ukraine “has been trying to control a polio outbreak since October,” reports Dana Varinsky at NBC News. About 13% of Ukrainian children under age six had not received their polio shots as of 2020, and are vulnerable to a re-emergence of this disease. Global health experts are highly concerned about the potential impacts of both COVID-19 and polio on Ukraine and neighboring countries.
- While data on Ukraine’s cases show a decrease in recent weeks, these numbers are pretty unreliable. Our World in Data reports a steep decline from 860 new cases per million on February 12 to zero new cases in the last couple of days. This is unsurprising for a country with pressing issues to deal with than data reporting. “These numbers are going to have to be taken with some sort of salt, understanding it may be underreported, or in many ways not reported at all,” public health expert Sonny Patel told NBC.
- Meanwhile in the U.S., hospitals are considering a potential increase in Russian cyber threats, POLITICO reports. Earlier in March, the U.S. Cybersecurity and Infrastructure Security Agency issued a warning to hospitals and other healthcare organizations saying they should prepare for Russian cyberattacks. “No “specific or credible” threats have been made yet, but health care organizations are concerned, given Russia’s cyber warfare history,” according to reporter Ben Leonard. (The full story is paywalled, but a summary is available in POLITICO’s newsletter.)
Over the past year, we’ve seen more and more examples of COVID-19 surges intersecting with other disasters. This includes violence in Palestine last summer, as well as hurricanes, wildfires, and the Texas winter storm here in the U.S. To me, these horrible convergences make it clear that healthcare systems in the U.S. and around the world need a lot more investment to be resilient in these times of crisis.
-

We failed to vaccinate the world in 2021; will 2022 be more successful?
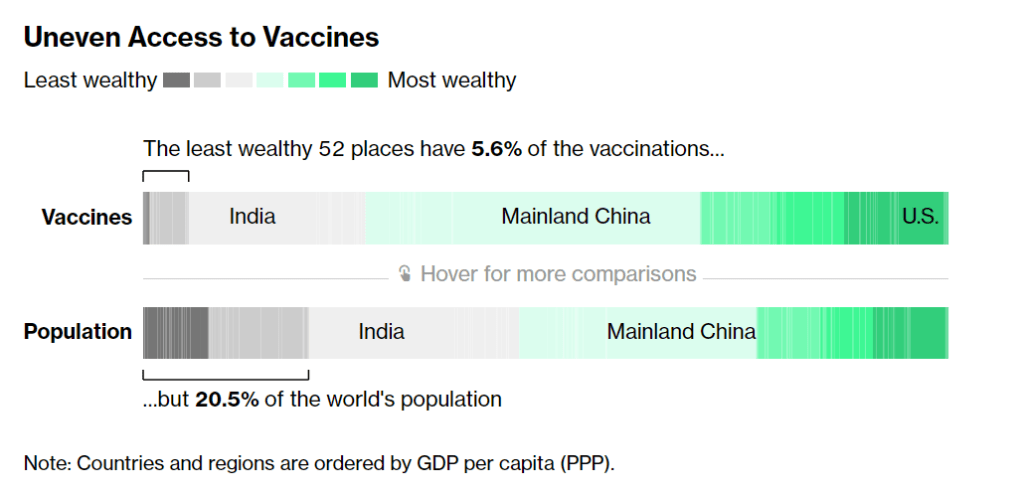
According to Bloomberg, the 52 least wealthy places in the world have 5.6% of the vaccinations. Chart from Bloomberg’s vaccine tracker, screenshot taken on December 19. In January, COVAX set a goal that many global health advocates considered modest: delivering 2.3 billion vaccine doses to low- and middle-income countries by the end of 2021. COVAX (or COVID-19 Vaccines Global Access) is an initiative to provide equitable access to vaccines; its leadership includes the United Nations, the World Health Organization (WHO), and other organizations.
Despite COVAX’s broad support, the initiative has revised its vaccine delivery projections down again and again this year. Now, the initiative is saying it’ll deliver just 800 million vaccine doses by the end of 2021, according to the Washington Post, and only about 600 million had been delivered by early December.
Considering that most COVID-19 vaccines are two-dose series—and boosters will likely be necessary to combat Omicron—those doses are just a drop in the bucket. According to Bloomberg’s vaccine tracker: “The least wealthy 52 places have 5.6% of the vaccinations, but 20.5% of the world’s population.”
Why this access gap? Many scientists and advocates in low- and middle-income nations blame vaccine manufacturers and rich countries like the U.S., I found when I reported a story on this topic for Popular Science.
“We basically have artificial scarcity of vaccine doses,” says Robbie Silverman, a vaccine advocate at Oxfam America. The pharmaceutical companies control “where doses are produced, where they’re sold, and at what price.” The world’s vaccine supply is thus limited by contracts signed by a small number of big companies; and many of those contracts, [Fatima Hassan, health advocate from South Africa] says, are kept secret behind non-disclosure agreements.
While rich countries claimed to support COVAX, the Washington Post reports, “they also placed advance orders with vaccine manufacturers before COVAX could raise enough money to do so.” This practice pushed COVAX to the back of the vaccine line—and then, when rich countries decided they needed booster shots, that pushed COVAX to the back of the line again. India’s spring 2021 surge didn’t help either, as the country blocked vaccine supplies produced at the Serum Institute of India from being exported to other nations.
According to Our World in Data, low-income nations have administered about 60 million doses total, while high-income nations have administered more than 300 million booster shots. At times this winter, there were more booster shots administered daily than first and second doses in low-income countries.
Even taking booster shots into consideration, there should be enough vaccine supplies produced by the end of this year to vaccinate 40% of the world’s population by the end of this year, meeting WHO targets, according to STAT News’ Olivia Goldhill. The world is on track to manufacture about 11 billion vaccines in total this year, Goldhill reports, while about 850 million doses are needed to get all countries to a 40% vaccination benchmark.
But again, rich countries pose a problem: the countries currently focused on administering booster shots have stockpiled hundreds of millions of doses, and are unwilling to send their stockpiles abroad. From STAT News:
“That number can be redistributed from what high-income countries expect to have by the end of this year. So it’s not an overall supply challenge,” said [Krishna Udayakumar, founding director of Duke’s Global Health Innovation Center]. “It’s very much an allocation challenge, as well as getting high income countries more and more comfortable that they don’t need to hold on to hundreds of millions of doses, for contingencies.”
The vaccine shortage for low-income countries is less than the surplus vaccines within the G7 countries and the European Union, according to separate analyses from both Duke and Airfinity, a life sciences analytics firm that is tracking vaccine distribution.
While leaders in the U.S., the U.K., and other nations with large stockpiles maintain that they can both administer booster shots at home and send doses for primary series shots abroad, their true priorities are clear. The U.S., for example, has pledged to donate 1.2 billion doses to other countries, but about 320 million—under one-third—of those doses have been shipped out so far.
Another challenge is the type of vaccines being used in wealthy nations, as opposed to low- and middle-income nations. Wealthy nations have been particularly eager to horde Pfizer and Moderna’s vaccines, which are more effective against Omicron and other variants of concern. On the other hand, many low-income nations have relied on Sputnik, CoronaVac, and other vaccines which are less effective.
“We’re now entering an era of second-class vaccines for second-class people,” Peter Maybarduk, director at the DC-based nonprofit Public Citizen, told me in October, discussing these differences in vaccine effectiveness. As Omicron spreads around the world, this concern is only growing.
The more the coronavirus spreads across the world, particularly in regions with less immunity from vaccines, the more it can mutate and create new variants. Delta and Omicron provide clear examples, demonstrating the need to vaccinate the world in 2022.
And there are some reasons to hope that this goal may be feasible. COVAX’s global supply forecast shows major jumps in vaccine supplies in the first three months of 2022. At the same time, vaccine companies are increasing their production capacity, and donations from the U.S. and other countries are expected to kick in. In South Africa, an mRNA vaccine hub is working to train African companies to manufacture COVID-19 vaccines similar to Pfizer and Moderna’s, without violating patents.
Still, additional variants—and the need for additional booster shots—could be a major hurdle, as vaccine companies continue to prioritize wealthy nations. These companies continue to refuse to share their intellectual property with other manufacturers, even as they make patents for COVID-19 antiviral drugs widely available. And, once vaccines are delivered, getting them from shipments into arms will be a challenge.
More international data
-
Sources and updates, December 12
- CDC adds booster shot trends to its dashboard: One significant update to the CDC’s COVID-19 dashboard this week: the agency has added daily booster shot administration trends to its Vaccination Trends page. Now, you can see how many booster shots are being given each day in your state; in New York, for example, I see clear jumps when eligibility opened to all adults, and when Omicron was identified after Thanksgiving.
- Global Health Security Index: Back in fall 2019, a group of public health and national security researchers put out an index that ranked 195 countries around the world on their capacity to respond to future health threats. The U.S. was ranked number one—a ranking that soon became laughable as the country proved to be incredibly unprepared for the COVID-19 pandemic. This week, the organization released their 2021 update to that index… and the U.S. is, somehow, still number one. Yet despite this, the researchers say, “no country is fully prepared for future pandemic or epidemic threats.”
- COVID Collaborative: Hidden Pain report: The COVID Collaborative is a team of health, education, and economic experts aiming to develop recommendations for U.S. leaders. Their recent Hidden Pain report focuses on children who lost parents or caretakers to COVID-19—a group that, the report estimates, includes over 167,000 children across the country.
- State Alcohol-Related Laws During COVID-19: The Alcohol Policy Information System has compiled a database of alcohol-related state laws during the pandemic, including rules about drinking both inside and outside of bars and restaurants. The database allows you to see when a specific state allowed restaurants to open or close, restrictions for take-out only, shortened hours, and more. (H/t Data Is Plural.)
-
Omicron variant: What we know, what we don’t, and why not to panic (yet)
On Thanksgiving, my Twitter feed was dominated not by food photos, but by news of a novel coronavirus variant identified in South Africa earlier this week. While the variant—now called Omicron, or B.1.1.529—likely didn’t originate in South Africa, data from the country’s comprehensive surveillance system provided enough evidence to suggest that this variant could be more contagious than Delta, as well as potentially more able to evade human immune systems.
Note that the words suggest and could be are doing a lot of work here. There’s plenty we don’t know yet about this variant, and scientists are already working hard to understand it.
But the early evidence is substantial enough that the World Health Organization (WHO) designated Omicron as a Variant of Concern on Friday. And, that same day, the Biden administration announced new travel restrictions on South Africa and several neighboring countries. (More on that later.)
In today’s issue, I’ll explain what we know about the Omicron variant so far, as well as the many questions that scientists around the world are already investigating. Along the way, I’ll link to plenty of articles and Twitter threads where you can learn more. As always, if you have more questions: comment below, email me, (betsy@coviddatadispatch.com), or hit me up on Twitter.
Where did the Omicron variant come from?
This is one major unknown at the moment. South Africa was the first country to detect Omicron this past Monday, according to STAT News. But the variant likely didn’t originate in South Africa; rather, this country was more likely to pick up its worrying signal because it has a comprehensive variant surveillance system.
Per The Conversation, this system includes: “a central repository of public sector laboratory results at the National Health Laboratory Service, good linkages to private laboratories, the Provincial Health Data Centre of the Western Cape Province, and state-of-the-art modeling expertise.”
Researchers from South Africa and the other countries that have detected Omicron this week are already sharing genetic sequences on public platforms, driving much of the scientific discussion about this variant. So far, one interesting aspect of this variant is that, even though Delta has dominated the coronavirus landscape globally for months, Omicron did not evolve out of Delta.
Instead, it may have evolved over the course of a long infection in a single, immunocompromised individual. It also may have flown under the radar in a country or region with poor genomic surveillance—which, as computational biologist Trevor Bedford pointed out on Twitter, is “certainly not South Africa”—and then was detected once it landed in that country.
Why are scientists worried about Omicron?
Omicron seems to be spreading very quickly in South Africa—potentially faster than the Delta variant. Based on publicly available sequence data, Bedford estimated that it’s doubling exponentially every 4.8 days.
An important caveat here, however, is that South Africa had incredibly low case numbers before Omicron was detected—its lowest case numbers since spring 2020, in fact. So, we cannot currently say that Omicron is “outcompeting” Delta, since there wasn’t much Delta present for Omicron to compete with. The current rise in cases may be caused by Omicron, or it may be the product of a few superspreading events that happen to include Omicron; we need more data to say for sure.
Still, as Financial Times data reporter John Burn-Murdoch pointed out: “There’s a clear upward trend. This may be a blip, but this is how waves start.”
Another major cause for concern is that Omicron has over 30 mutations on its spike protein, an important piece of the coronavirus that our immune systems learn to recognize through vaccination. Some of these mutations may correlate to increased transmission—meaning, they help the virus spread more quickly—while other mutations may correlate to evading the immune system.
Notably, a lot of the mutations on Omicron are mutations that we simply haven’t seen yet in other variants. On this diagram from genomics expert Jeffrey Barrett, the purple, yellow, and blue mutations are all those we haven’t seen on previous variants of concern, while the red mutations (there are nine) have been seen in previous variants of concern and are known to be bad.
Some of these new mutations could be terrible news, or they could be harmless. We need more study to figure that out. This recent article in Science provides more information on why scientists are worried about Omicron’s mutations, as well as what they’re doing to investigate.
How many Omicron cases have been detected so far?
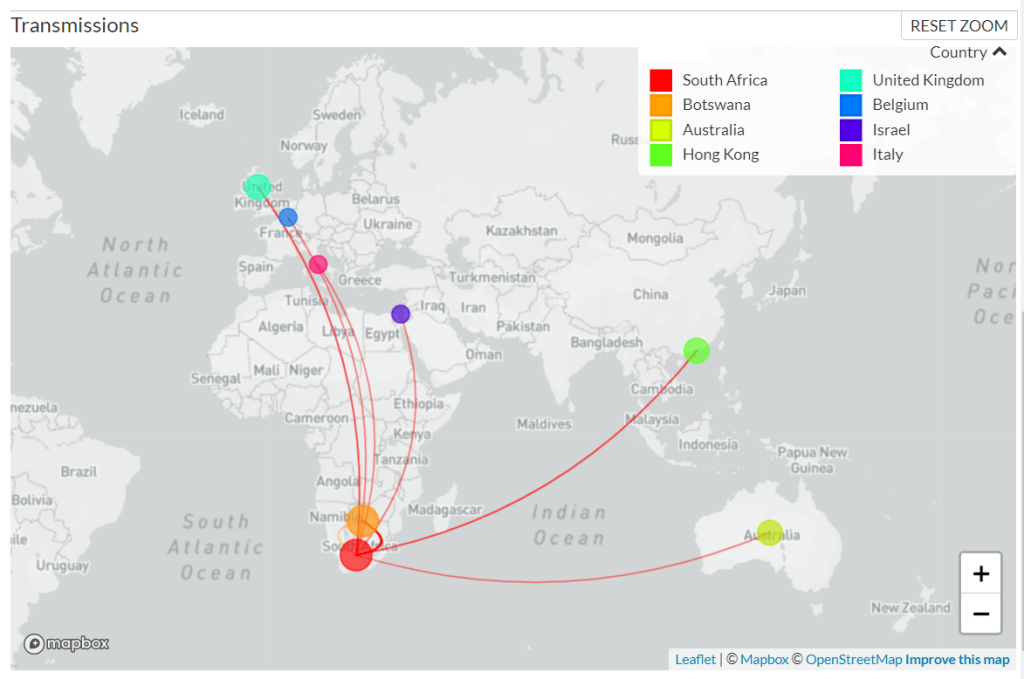
As of Sunday morning, genetic sequences from 127 confirmed Omicron cases have been shared to GISAID, the international genome sharing platform. The majority of these cases (99) were identified in South Africa, while 19 were identified in nearby Botswana, two in Hong Kong, two in Australia, two in the U.K., one in Israel, one in Belgium, and one in Italy.
According to BNO News, over 1,000 probable cases of the variant have already been identified in these countries. Cases have also been identified in the Netherlands, Germany, Denmark, the Czech Republic, and Austria. Many of the cases in the Netherlands are connected to a single flight from South Africa; the travelers on this flight were all tested upon their arrival, and 61 tested positive—though authorities are still working to determine how many of those cases are Omicron.
The U.K. Health Security Agency announced on Saturday that it had confirmed two Omicron cases in the country. Both of these cases, like those in Israel and Belgium, have been linked to travel—though the Belgium case had no travel history in South Africa. “This means that the virus is already circulating in communities,” Dr. Katelyn Jetelina writes in a Your Local Epidemiologist post about Omicron.

After South African scientists sounded the alarm about Omicron, cases were detected in Botswana, Australia, Hong Kong, Israel, the U.K., and other countries. Chart via GISAID, screenshot taken about 11:30 AM NYC time on November 28. Omicron hasn’t been detected in the U.S. yet. But the CDC is closely monitoring this variant, the agency announced in a rather sparse Friday press release.
Luckily, Omicron is easy to identify because one of its spike protein mutations enables detection on a PCR test—no genomic sequencing necessary. Alpha, the variant that originated in the U.K. last winter, has a similar quality.
How does Omicron compare to Delta?
This is another major unknown right now. As I mentioned earlier, Omicron is spreading quickly in South Africa, at a rate faster than Delta spread when it arrived in the country a few months ago. But South Africa was seeing a very low COVID-19 case rate before Omicron arrived, making it difficult to evaluate whether this new variant is directly outcompeting Delta—or whether something else is going on.
(Note that a couple of the tweets below refer to this variant as “Nu,” as they were posted prior to the WHO designating it Omicron.)
We also don’t know if Omicron could potentially evade the human immune system, whether that means bypassing immunity from a past coronavirus infection or from vaccination. However, vaccine experts say that a variant that would entirely evade vaccines is pretty improbable.
Every single coronavirus variant of concern that we’ve encountered so far has responded to the vaccines in some capacity. And the variants that have posed more of a danger to vaccine-induced immunity (Beta, Gamma) have not become dominant on a global scale, since they’ve been less transmissible than Delta. Our vaccines are very good—not only do they drive production of anti-COVID antibodies, they also push the immune system to remember the coronavirus for a long time.
It’s also worth noting here that, so far, Omicron does not appear to be more likely to cause severe COVID-19 symptoms. Angelique Coetzee, chairwoman of the South African Medical Association, announced on Saturday that cases of the variant have been mild overall. Hospitals in South Africa are not (yet) facing a major burden from Omicron patients.
What can scientists do to better understand Omicron?
One thing I cannot overstate here is that scientists are learning about Omicron in real time, just as the rest of us are. Look at all the “We don’t know yet.”s in this thread from NYU epidemiologist Céline Gounder:
Gounder wrote that we may have answers to some pressing questions within two weeks, while others may take months of investigation. To examine the vaccines’ ability to protect against Omicron, scientists are doing antibody studies: essentially testing antibodies that were produced from past vaccination or infection to see how well they can fight off the variant.
At the same time, scientists are closely watching to see how fast the variant spreads in South Africa and in other countries. The variant’s performance in the U.K., where it was first identified on Saturday, may be a particularly useful source of information. This country is currently facing a Delta-induced COVID-19 wave (so we can see how well Omicron competes); and the U.K. has the world’s best genomic surveillance system, enabling epidemiologists to track the variant in detail.
How does Omicron impact vaccine effectiveness?
We don’t know this yet, as scientists are just starting to evaluate how well human antibodies from vaccination and past infection size up against the new variant. The scientists doing these antibody studies include those working at Pfizer, Moderna, and other major vaccine manufacturers. Pfizer’s partner BioNTech has said it expects to share lab data within two weeks, according to CNBC reporter Meg Tirrell:
If BioNTech finds that Omicron is able to escape immunity from a Pfizer vaccination, the company will be able to update that vaccine within weeks. Moderna is similarly able to adjust its vaccine quickly, if lab studies show that an Omicron-specific vaccine is necessary.
Even if we need an updated vaccine for this variant, though, people who are already vaccinated are not going back to zero protection. As microbiologist Florian Krammer put it in a Twitter thread: “And even if a variant vaccine becomes necessary, we would not start from scratch… since it is likely that one ‘variant-booster’ would do the job. Our B-cells can be retrained to recognize both, the old version and the variant, and it doesn’t take much to do that.”
What can the U.S. do about Omicron?
On Friday, the Biden administration announced travel restrictions from South Africa and neighboring countries. The restrictions take effect on Monday, but virus and public health experts alike are already criticizing the move—suggesting that banning travel from Africa is unlikely to significantly slow Omicron’s spread, as the variant is very likely already spreading in the U.S. and plenty of other countries.
At the same time, travel restrictions stigmatize South Africa instead of thanking the country’s scientists for alerting the world to this variant. Such stigma may make other countries less likely to share similar variant news in the future, ultimately hurting the world’s ability to fight the pandemic.
So what should the U.S. actually be doing? First of all, we need to step up our testing and genomic surveillance. As I mentioned above, Omicron can be identified from a PCR test; an uptick in PCR testing, especially as people return home from Thanksgiving travel, could help identify potential cases that are already here.
We also need to increase genomic surveillance, which could help identify Omicron as well as other variants that may emerge from Delta. In a post about the Delta AY.4.2 variant last month, I wrote that the U.S. is really not prepared to face surges driven by coronavirus mutation:
We’re doing more genomic sequencing than we were at the start of 2021, which helps with identifying potentially concerning variants, but sequencing still tends to be clustered in particular areas with high research budgets (NYC, Seattle, etc.). And even when our sequencing system picks up signals of a new variant, we do not have a clear playbook—or easily utilized resources—to act on the warning.
We also need to get more people vaccinated, in the U.S. and—more importantly—in the low-income nations where the majority of people remain unprotected. In South Africa, under one-quarter of the population is fully vaccinated, according to Our World in Data.
What can I do to protect myself, my family, and my community?
In general, do all of the same things that you’ve already been doing. Most importantly, get vaccinated (including a booster shot, if you’re eligible).
Also: Wear a mask in indoor spaces, ideally a good quality mask (N95, KN95, or double up on surgical and cloth masks). Avoid crowds if you’re able to do so. Monitor yourself for COVID-19 symptoms, including those that are less common. Utilize tests, including PCR and rapid tests—especially if you’re traveling, or if you work in a crowded in-person setting.
I’ve seen some questions on social media about whether people should consider canceling holiday plans, or other travel plans, because of Omicron. This is a very personal choice, I think, and I’m no medical expert, but I will offer a few thoughts.
As I said in the title of this post, we don’t yet know enough about this variant for it to be worth seriously panicking over. All of the evidence—based on every single other variant of concern that has emerged—suggests that the vaccines will continue to work well against this variant, at least protecting against severe disease. And all of the other precautions that work well against other variants will work against this one, too.
So, if you are vaccinated and capable of taking all the other standard COVID-19 precautions, Omicron is most likely not a huge risk to your personal safety right now. But keep an eye on the case numbers in your community, and on what we learn about this variant in the weeks to come.
What does Omicron mean for the pandemic’s trajectory?
This variant could potentially lead to an adjustment in our vaccines, as well as to new surges in the U.S. and other parts of the world. It’s too early to say how likely either scenario may be; we’ll learn a lot more in the next couple of weeks.
But one thing we can say right now, for sure, is that this variant provides a tangible argument for global vaccine equity. If the country where Omicron originated had a vaccination rate as high as that of the U.S. and other high-income nations, it may not have gained enough purchase to spread—into South Africa, and on the global path that it’s now taking.
As physician, virologist, and global health expert Boghuma Kabisen Titanji put it in a recent interview with The Atlantic:
If we had ensured that everyone had equal access to vaccination and really pushed the agenda on getting global vaccination to a high level, then maybe we could have possibly delayed the emergence of new variants, such as the ones that we’re witnessing.
I will end the post with this tweet from Amy Maxmen, global health reporter at Nature. The Omicron variant was a choice.
More variant reporting