In the past week (June 19 through 25), the U.S. reported about 79,000 new cases, according to the CDC. This amounts to:
- An average of 11,000 new cases each day
- 24 total new cases for every 100,000 Americans
- 4% fewer new cases than last week (June 12-18)
Last week, America also saw:
- 12,900 new COVID-19 patients admitted to hospitals (3.9 for every 100,000 people)
- 2,000 new COVID-19 deaths (0.6 for every 100,000 people)
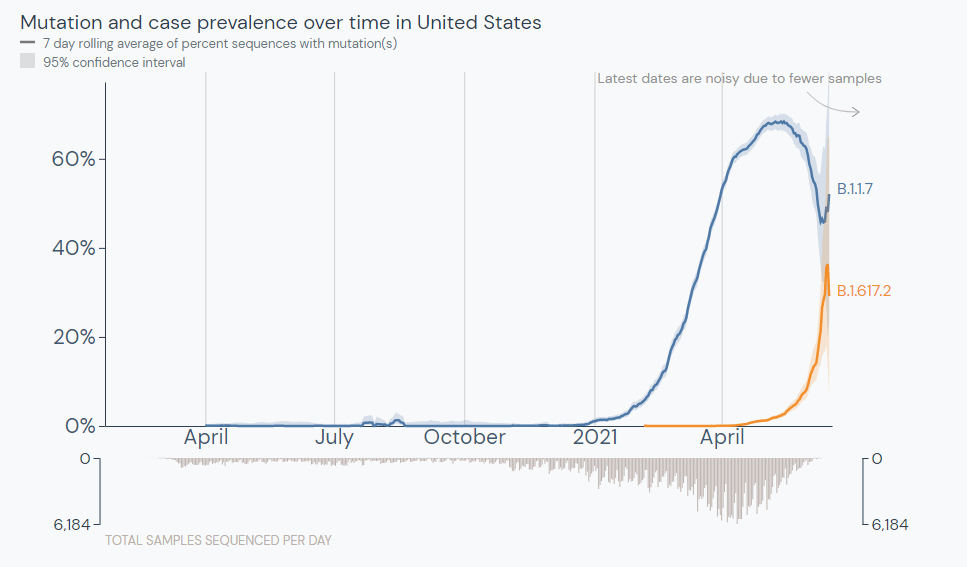
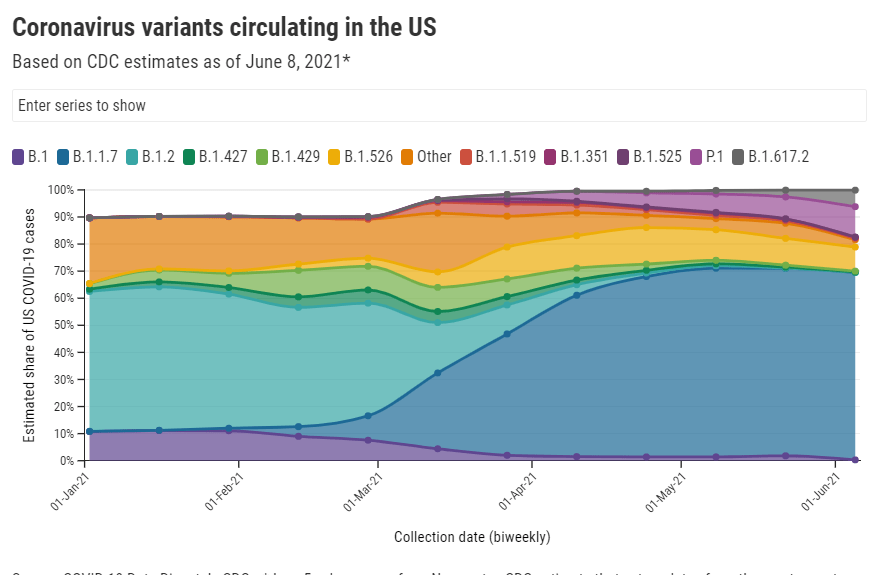
- 52% of new cases in the country now Alpha-caused (as of June 19)
- 21% of new cases now Delta-caused (as of June 19)
- An average of 0.75 million vaccinations per day (per Bloomberg)

Cases have continued to plateau this week, with less than a 5% drop in the daily average. As I’ve said in previous weeks, this is partially due to slowing vaccinations—the White House admitted last week that the U.S. won’t meet Biden’s July 4 goal—and partially due to the Delta variant, which now causes at least 20% of new cases in the country. (More on Delta later.)
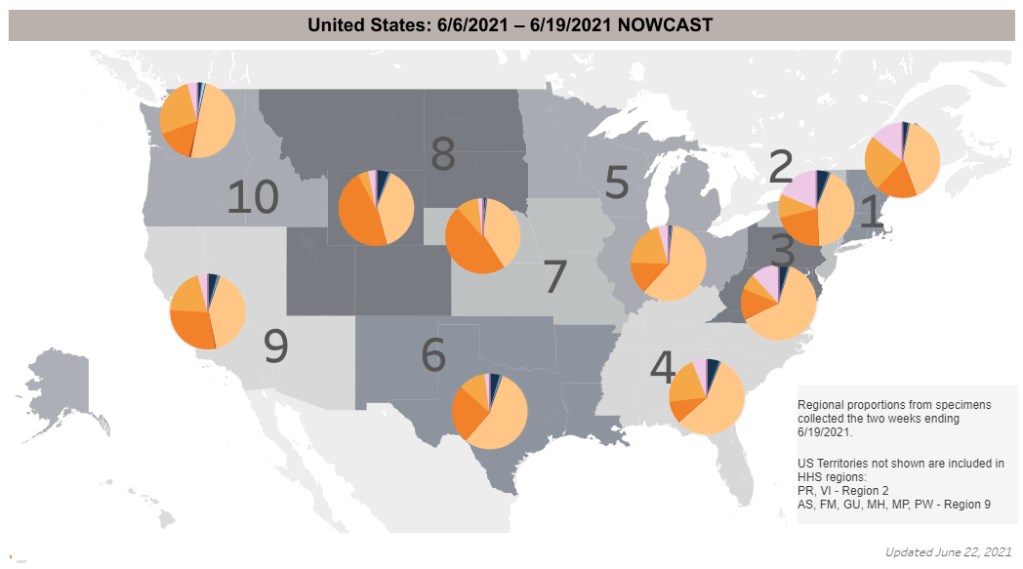
While those parts of the country that are widely vaccinated are still seeing low case numbers, others may need to prepare for another surge. A few Midwest states, in particular, have seen case jumps in recent weeks; the Delta variant is more prevalent in this region than others, per CDC data. (See the orange pie chart slices on the map above.)
Missouri now has the highest rate of new COVID-19 cases per capita: 87 cases for every 100,000 people during the week ending June 23, more than three times higher than the national average. The state has seen a sharp increase in COVID-19 patients requiring hospital care, including younger adults who may be less likely to get vaccinated. Experts in the state worry that this may be “a preview of what is to come in other parts of the country that don’t have higher vaccination rates.”
Just under 300 Americans are now dying from COVID-19 every day. A new analysis from the Associated Press confirms what many public health experts have expected: the vast majority of those deaths have occured in unvaccinated people. In May, only 150 out of over 18,000 COVID-19 deaths were in fully vaccinated Americans, the AP analysis found.
This is why CDC Director Dr. Rochelle Walensky recently said that “nearly every death, especially among adults, due to COVID-19, is, at this point, entirely preventable.”