- CDC awards $3 billion to improve public health infrastructure: The CDC announced this week that it has awarded state and local public health agencies a total of $3.2 billion to support hiring and training new workers, along with other infrastructure needs. The agency published a breakdown of all the agencies that received awards, although it has not included specific details on what funds will be used for in each place. Local reporters, if your health department received funding, this might be worth looking into!
- CDC expands wastewater testing for polio: Another notable CDC announcement this week: the agency is expanding its wastewater surveillance for polio to two new areas, Oakland County, Michigan and Philadelphia. Testing wastewater for polio is more complicated than testing it for the coronavirus, as STAT News’ Helen Branswell explains in this article; as a result, the CDC is expanding this surveillance in a more limited capacity than what it’s doing for other viruses, like monkeypox and the flu.
- Majority of COVID-19 deaths are now among vaccinated people: A new report from the Kaiser Family Foundation explains why more than 50% of COVID-19 deaths in the U.S. in recent months were among people who had received at least two vaccine doses. According to KFF, factors driving this trend include the rising share of Americans who are vaccinated, waning protection from initial doses, and low uptake of booster shots—particularly of the Omicron-specific boosters that provide better protection against newer variants. More reason to get the new booster if you haven’t yet!
- Paid sick leave correlates with higher vaccination rates: Speaking of vaccination: a new study from researchers at Drexel University and Boston University found that large U.S. cities with city-wide paid sick leave policies had higher vaccination rates than those without such policies. The correlation was particularly evident in neighborhoods with higher social vulnerability, the researchers found. Expanding paid sick leave could help reduce inequities in vaccination coverage, the paper’s authors recommend.
- No monoclonal antibody drugs are currently authorized in the U.S.: This week, the FDA announced that bebtelovimab, a monoclonal antibody made by Eli Lilly, is no longer authorized for COVID-19 treatments in the U.S. The drug was designed based on older versions of the Omicron variant and doesn’t perform well against BQ.1 and BQ.1.1, the sublineages that are currently causing the majority of new cases in the U.S. As a result, no monoclonal antibodies are currently authorized, though Paxlovid and other treatments are still available.
Tag: booster shots
-
Sources and updates, December 4
-
Sources and updates, November 27
- More data on the new, bivalent boosters: A new study, published this week in the CDC’s Morbidity and Mortality Weekly Report, has further evidence that the new, Omicron-specific booster shots provide additional protection against COVID-19 for people who previously received the original vaccines. Researchers used test results from pharmacies to compare symptomatic COVID-19 cases among people who had received the new boosters to those who had only received older vaccines. New booster recipients were less likely to get sick, they found, indicating protection against Omicron BA.4, BA.5, and their sublineages. In short: if you haven’t gotten one of the new boosters yet, now is a good time!
- Patient-Led Research Collaborative announces grant winners: The Patient-Led Research Collaborative, an organization of Long COVID patient-researchers that has produced groundbreaking work about this condition, just announced the winners of its $5 million fund to support new biomedical research on Long COVID. The winning projects will pursue avenues of top priority to patients, such as understanding post-exertional malaise, testing for microclots, and a clinical trial for the drug naltrexone. Projects were themselves evaluated by a panel of patient experts and patients will be heavily involved in the resulting research. Congrats to the PLRC team on this announcement, and I look forward to following the results of these studies!
- HHS publishes Health+ Long COVID report: Another piece of Long COVID news this week: the Department of Health and Human Services published a report summarizing interviews with people who have Long COVID. The report was one of several responses to the Biden administration’s call last spring for Long COVID research and support programs. It describes patients’ desires for meaningful research, better healthcare, financial support, and more. While this new report may not be adding much to the body of knowledge about Long COVID, it’s helpful to see this information coming from a major government source.
- Football games associated with COVID-19 spread: And one more study that caught my attention this week: a new paper in JAMA Network Open describes a correlation between National Football League (NFL) games and COVID-19 spikes in the surrounding counties during the league’s 2020-2021 season. Counties hosting more popular games (with at least 20,000 fans present) were more likely to see increased COVID-19 spread afterwards. The paper shows how large events can contribute to widespread disease transmission, even among people who didn’t themselves attend the events.
-
Sources and updates, November 20
- CDC update on COVID-19 mortality trends: This week, the CDC published a detailed report about how deaths from COVID-19 have changed in 2022. Overall, between 2,000 and 4,500 COVID-19 deaths were reported each week between April and September 2022, the CDC researchers found; this is lower than at earlier points in the pandemic, but still represents a loss of more than 100,000 Americans over the course of a year. Older adults and those who were un- or under-vaccinated had a higher risk of death from COVID-19, the researchers found; racial and ethnic disparities have “decreased, but persisted.”
- Moderna reports new data on its bivalent booster: Several studies in the last couple of weeks have indicated that the new, Omicron-specific boosters from Pfizer and Moderna are more effective against new variants than the older vaccines. Moderna provided additional data this week, reporting that its new booster led to five times more antibodies that neutralize Omicron BA.4 and BA.5 compared to earlier booster shots. While Moderna’s study hasn’t yet been peer-reviewed, the results are promising in following a trend from past studies, STAT’s Matthew Herper reports.
- Booster shots could keep kids from missing school: Speaking of the new boosters: a new report from the Commonwealth Fund provides analysis of the boosters’ potential impact on school-aged children, as all kids older than five are eligible for the shots. If 80% of eligible Americans receive their bivalent boosters by the end of 2022, the report suggests, this could save over 46 million days of isolation and over 50,000 hospitalizations for school-aged children, along with other benefits. Even getting kids boosted at the level of flu vaccination in 2020-2021 would prevent millions of days of school from being lost.
- Test to treat is inaccessible to rural Americans: A new study, published this week in JAMA Network Open, examined equity issues with the Biden administration’s Test to Treat initiative. The initiative was designed to provide locations where Americans could get a COVID-19 test and then, if they received a positive result, quickly receive a free antiviral drug. But many people don’t live near available locations, the researchers found: “approximately 15% of the overall US population, 30% of American Indian or Alaskan Native people, and 59% of the rural population lived more than 60 minutes from the nearest site,” they write.
- Perception of local COVID-19 levels: A lot of people are acting with incorrect knowledge of their local COVID-19 risk, a new study in the CDC’s Morbidity and Mortality Weekly Report suggests. Researchers from several medical and public health institutions surveyed people who had recently tested positive for COVID-19 in Detroit, Michigan and DuPage County, Illinois, during June and July, 2022. About half of the 5,000 people surveyed said that they thought local COVID-19 transmission was “low or moderate,” even though it was actually at high levels in both places.
-
Sources and updates, November 13
- Updated booster doses by state: This week, the CDC started reporting how many people have received the bivalent, Omicron-specific boosters by state, including state-level data for several demographic groups (over age 5, over 12, over 18, and over 65). The numbers are low: Vermont and Washington, D.C. have the highest booster rates as of November 9, with 21% and 20% of their populations receiving the bivalent shots, respectively. In about half of states, less than 10% of the population has received an updated booster. (H/t Jason Salemi.)
- Additional data suggests new boosters work against BQs: Speaking of the updated booster shots, a recent preprint from researchers at Emory University, Stanford University, and the NIH found that the new boosters produced several times more neutralizing antibodies against subvariants BQ.1.1 and BA.2.75.2 compared to the older vaccines. This was a small lab study and hasn’t yet been peer-reviewed, but it follows similar evidence from other research suggesting that the new boosters do provide additional protection against the most concerning variants currently circulating in the U.S. (See last week’s post.) If you haven’t gotten a bivalent booster yet, now is a good time!
- More evidence that masks in schools prevent COVID-19 spread: Another notable new study this week, published in the New England Journal of Medicine: a group of researchers from Boston institutions examined the differences in COVID-19 case numbers between public school districts that kept mask requirements in place during spring 2022, and those that lifted their requirements upon a statewide policy change in February. Overall, ending required masking led to “an additional 44.9 COVID-19 cases per 1,000 students and staff” during the remainder of the semester, the researchers found. The study demonstrates that masks are still a useful public health strategy to reduce illness—and risk of Long COVID—in schools.
- Paxlovid may reduce Long COVID risk: When Paxlovid first became available earlier in the year, some Long COVID patients reported that the drug helped alleviate their symptoms. A new study from Ziyad Al-Aly and his team at the Veterans Affairs St. Louis healthcare system provides evidence behind the anecdotal reports, finding that veterans treated with Paxlovid had a 25% lower risk of long-term symptoms, based on their electronic health records. The study has received some criticism (and has not yet been peer-reviewed); to me, it provides motivation for actual clinical trials examining Paxlovid’s use for treating Long COVID. RECOVER is running one such trial, but it won’t start until early 2023.
- Estimating COVID-19 infections from wastewater: And one more study that caught my attention this week: researchers at the University of Florida used a modeling technique called a “mass balance equation” to estimate how many people in Gainseville, Florida were sick with COVID-19 based on the virus’ concentration in wastewater. Using about one year of wastewater data (May 2020 to May 2021), the researchers were able to accurately predict actual infections with an error of just 1%. Translating wastewater data into useful information for public health action has been a major challenge for the growing field, so I was glad to see this study providing a potentially-useful method.
-
National numbers, November 13

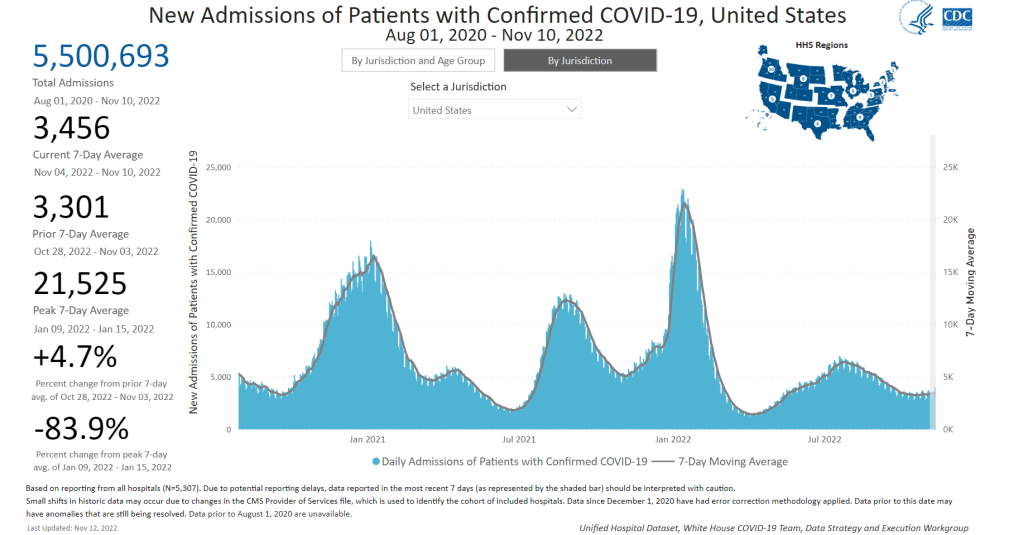
COVID-19 hospitalizations have risen slightly in recent weeks, indicating the start of a fall/winter surge, according to CDC data. In the past week (November 3 through 9), the U.S. reported about 290,000 new COVID-19 cases, according to the CDC. This amounts to:
- An average of 41,000 new cases each day
- 88 total new cases for every 100,000 Americans
- 6% more new cases than last week (October 27-November 2)
In the past week, the U.S. also reported about 24,000 new COVID-19 patients admitted to hospitals. This amounts to:
- An average of 3,500 new admissions each day
- 7.4 total admissions for every 100,000 Americans
- 5% more new admissions than last week
Additionally, the U.S. reported:
- 2,300 new COVID-19 deaths (340 per day)
- 44% of new cases are caused by Omicron BQ.1 and BQ.1.1; 8% by BF.7; 2% by BA.2.75 and BA.2.75.2 (as of November 12)
- An average of 400,000 vaccinations per day
We are beginning to see the impacts of colder weather and new variants this week, as both official COVID-19 cases and new hospital admissions went up slightly: increasing by 6% and 5% from the prior week, respectively.
Wastewater monitoring similarly shows an uptick in coronavirus transmission at the national level, according to Biobot’s dashboard. The Northeast still has the highest virus concentration, but other regions of the country are catching up—particularly the West coast, which reported a significant increase in the last two weeks.
About half of the wastewater surveillance sites included on the CDC’s national dashboard reported increases in coronavirus transmission over the two-week period ending November 7, with 30% of sites reporting increases of at least 100%.
Omicron BQ.1 and BQ.1.1 are likely a major source of increased virus spread. These two strains—subvariants of BA.5 that are even more contagious—now account for 44% of new cases in the week ending November 12, according to CDC estimates. New variants tend to have an impact on transmission when they reach about 50% prevalence, so we will likely see more BQ-driven spread in the weeks to come.
The New York/New Jersey region continues to report the highest amounts of BQ.1 and BQ.1.1: these variants represented about 60% of new cases in the last week. These two states also reported some of the highest (official) case rates in the country last week, along with Puerto Rico, New Mexico, and North Dakota, per the latest Community Profile Report. Cases and hospitalizations in New York City, often a bellwether for the rest of the country, are rising again.
At the same time, the U.S. is seeing an early and intense flu season. Most of the country’s Southeast region (from Virginia to Mississippi) reported the highest possible levels of influenza-like activity in the week ending November 5, according to the CDC. Flu, COVID-19, and RSV are all straining hospitals as we head into the holiday season.
The new, Omicron-specific booster shots provide enhanced protection against the latest variants, but uptake remains very low—as shown by new CDC data providing vaccinations by state. Only 10% of the eligible population has received one of the new shots, as of November 9.
-
Sources and updates, November 6
- New data on Omicron boosters: This week, we got two major updates on the safety and effectiveness of the bivalent, Omicron-specific booster shots from Pfizer and Moderna. First, a study in the CDC’s Morbidity and Mortality Weekly Report examined safety, finding that side effects of the new boosters similar to the side effects of previous vaccines, according to the agency’s vaccine surveillance systems. For example, about 60% of vaccine recipients experienced pain, swelling, or itching in the arms where they received the shot. And second, Pfizer and BioNTech shared new data about the companies’ bivalent booster, suggesting that the new booster produces four times more neutralizing antibodies against BA.4 and BA.5 compared to the original booster shot. The study focused on older adults (over age 55) but is still helpful evidence that the new boosters are more effective against currently-circulating variants.
- NIH RECOVER is preparing its first clinical trial: RECOVER, the National Institutes of Health’s flagship study to understand and eventually treat Long COVID, announced this week that it’s preparing clinical trials to test potential treatments. The first of these trials was recently posted to ClinicalTrials.gov (a site for tracking studies that have received federal funding). This trial will focus on testing Paxlovid for Long COVID patients, and RECOVER anticipates it will begin enrolling patients in early 2023. Patients have previously expressed concerns that RECOVER is moving pretty slowly with trials, considering how many Americans are impacted by Long COVID.
- Patients Rising Now Congressional Scorecard: Speaking of government action on medical issues: Patients Rising Now, an advocacy organization focused on patients with chronic illnesses, recently published its first scorecard for Congressional representatives. The resource grades every Senator and House member in the 117th Congress based on how their voting record aligns with the organization’s priorities. While COVID-19 is not specifically mentioned in the grades, this scorecard could have implications for future pandemic-related votes.
- COVID-19 vaccination and race/ethnicity inequities: A new paper from researchers at the University of Minnesota and Boston University examined how vaccination impacted COVID-19 mortality patterns in Minnesota. During the Delta and Omicron surges, the researchers found, mortality among middle-aged people of color was higher than mortality among white people in an age group ten years older. The paper shows that COVID-19 remains “a pandemic of the disadvantaged,” author Elizabeth Wrigley-Field wrote on Twitter. (Disclaimer: through my work at MuckRock, I am collaborating with BU researcher Andrew Stokes, one of the paper’s coauthors.)
- RSV vaccine(s) could be coming soon: Finally, a bit of good news about another respiratory virus: two potential vaccines for RSV are likely to be under FDA review in the coming months. Pfizer recently reported promising results from a clinical trial of a vaccine for pregnant people, who pass antibodies to their children (thus reducing infant RSV risk). And U.S. pharmaceutical company GSK reported results from a trial testing its RSV vaccine for older adults.
-
Sources and updates, October 30
- More detailed bivalent booster data: As of this week, the CDC is reporting some demographic data for the bivalent, Omicron-specific booster shots. The new data suggest that these boosters have had higher uptake among seniors, with about 11 million people over age 65 receiving a shot (compared to just 60,000 in the 5 to 11 age group). White and Asian Americans have higher booster rates than Black, Hispanic, and Native Americans, suggesting that the new doses are following a similar equity pattern to what we’ve seen with prior vaccines.
- COVID-19 mortality by occupation: A new report by the CDC’s National Vital Statistics System provides a rare area of data we don’t usually get in the U.S.: occupational data. CDC researchers used mortality data from 46 states and New York City to examine risk of death by occupation. People working in protective services, accommodation and food services, and other essential jobs that couldn’t be done remotely had the highest death rates—confirming what many public health experts have suspected throughout the pandemic.
- Life expectancy changes during the pandemic: A new study published in Nature, by researchers at the University of Oxford and other European institutions, estimated how life expectancy changed in 29 countries since the start of the pandemic. After a universal life expectancy decline in 2020, the researchers found, some western European countries “bounced back” in 2021 while the U.S. and eastern European countries did not. The results show the impacts of lower vaccination uptake in the U.S., particularly among younger adults.
- Disparities in Paxlovid prescriptions: Another CDC study that caught my attention this week was this analysis in Morbidity and Mortality Weekly Report (MMWR), describing racial and ethnic disparities in prescriptions of Paxlovid—the antiviral COVID-19 treatment which reduces risk of severe symptoms. Between April and July 2022, the researchers found, the share of COVID-19 patients over age 20 who received a Paxlovid prescription was 36% lower among Black patients than among White patients, and 30% lower among Hispanic patients. More work is needed to make Paxlovid availability more equitable.
- New estimates of Long COVID prevalence: One more notable paper published this week: researchers at Massachusetts General Hospital, Harvard, and collaborators conducted an online survey of about 16,000 U.S. adults who tested positive for COVID-19 in the last two months. Of those survey respondents, 15% reported current symptoms of Long COVID. The survey found that older adults and women were more likely to report Long COVID, while those who were fully vaccinated prior to infection had a somewhat lower risk of long-term symptoms. All of these findings are in line with results from other studies, but it’s helpful to see continued validation of these known trends.
-
The U.S. needs to step up its booster shot campaign

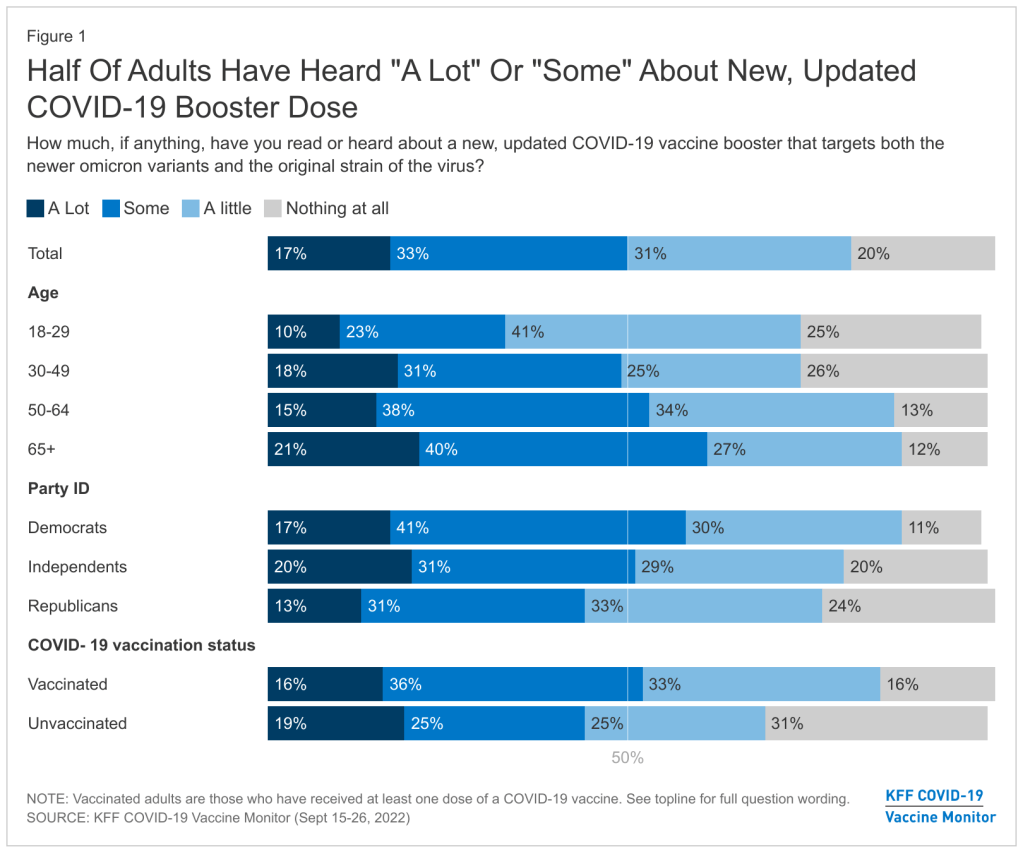
About half of U.S. adults haven’t heard much about the updated COVID-19 booster shots, according to a recent survey done by the Kaiser Family Foundation. New, Omicron-specific booster shots are publicly available for all American adults who’ve been previously vaccinated. This is the first time our shots actually match the dominant coronavirus variant (BA.5), and possibly the last time that the shots will be covered for free by the federal government.
So… why does it feel like almost nobody knows about them? Since the CDC and FDA authorized these shots, I’ve had multiple conversations with friends and acquaintances who had no idea they were eligible for a new booster. My own booster happened in a small, cramped room of a public hospital—a far cry from the mass vaccination sites that New York City has offered in past campaigns.
This week, the Kaiser Family Foundation (KFF) provided some data to back up such anecdotal evidence. According to the September iteration of KFF’s Vaccine Monitor survey, about half of U.S. adults have heard only “a little” or “nothing at all” about the new boosters. That includes more than half of adults who have been previously vaccinated.
Moreover, the KFF survey found that 40% of previously vaccinated adults (who received the full primary series) are “not sure” if the updated booster is recommended for them. Another 11% said the new booster is not recommended for them—which is not true! The CDC has recommended these boosters for everyone who previously got vaccinated.
Booster eligibility knowledge is even lower in certain demographics, KFF found. That includes: 55% of previously vaccinated Black adults and 57% of Hispanic adults don’t know that they’re eligible for boosters. Same thing for 57% of vaccinated adults with less than a college education and 58% of those living in rural areas.

As of September 28, only 7.6 million Americans have received an updated booster shot, the CDC reports. Overall, the CDC reports that about 7.6 million Americans have received an updated booster shot as of September 28, including 4.9 million who received a Pfizer shot and 2.7 million who received a Moderna shot. This represents less than 4% of all fully vaccinated adults who are eligible for the new boosters. And we don’t have demographic data yet, but I expect the patterns will fall among similar lines to what KFF’s survey found.
“Clear and consistent messaging accompanied by strategies to deliver boosters is needed to narrow these gaps,” said public health expert Anne Sosin, sharing the KFF findings on Twitter. We need big, public campaigns for the new boosters in line with what we got for the original vaccines in 2021—or else the new shots won’t be very helpful in an inevitable fall/winter surge.
More vaccine data
-
Sources and updates, September 25
- CDC adds data on new booster shots: The latest addition to the CDC’s COVID Data Tracker is the Omicron-specific, bivalent booster shots, authorized a couple of weeks ago. So far, the CDC has only provided a total count of Omicron booster recipients (4.4 million, as of September 21) and incorporated these boosters into total counts of Americans who’ve received “first” and “second boosters. A note at the top of the dashboard explains the CDC is working to provide more granular data about the new boosters as separated out from past boosters.
- Evidence Commons (ASU): Researchers at Arizona State University’s College of Health Solutions have compiled this detailed dashboard of scientific publications related to COVID-19 tests, supported with funding from the Rockefeller Foundation. The dashboard incorporates information from over 3,000 papers, sorted by the type of test under study, methodology, analysis location, and more. It’s a helpful tool to sort through diagnostic details that are often buried in technical documents.
- Helix announces new CDC partnership: Speaking of testing, the viral sequencing and population genomics company Helix announced this week that it has an “extended agreement” with the CDC to sequence coronavirus samples for the agency’s analysis. While Helix has been working with the CDC on variant tracking for some time, the new partnership extends this important effort: Helix (and research partners) will sequence over 3,000 coronavirus samples per week for the next year, “with the option to double the number of samples during surge moments,” according to the company’s press release.
- Pathogen Genomics Centers of Excellence: The CDC has also directed new surveillance funding to five state health departments that will test out new genomics technologies and respond to infectious disease outbreaks. These five departments—Georgia, Massachusetts, Minnesota, Virginia, and Washington—are receiving $90 million over the next five years; the funding came out of $1.7 billion allocated for genomic surveillance in the American Rescue Plan. I’m glad to see this sustained funding going beyond COVID-19, though I wish more than five states were getting the money!
- Long-term nervous system damage from COVID-19: Ziyad Al-Aly and his team at the Veterans Affairs St. Louis Healthcare System have published a new paper on long-term impacts from a COVID-19 infection. The study used a large dataset of electronic health records from a national VA database, including 154,000 people with COVID-19 and over five million controls. COVID-19 patients had an elevated risk of strokes, cognition and memory problems, seizures, mental health disorders, encephalitis, and more. While the VA population isn’t the best representation for the U.S. population as a whole (it skews older and male), the study still provides evidence for long-term neurological complications from COVID-19.
- Long COVID estimates in Europe: And one more piece of Long COVID news for this week: the World Health Organization’s European division has produced new estimates on Long COVID for the continent. Between 10% and 20% of COVID-19 cases in Europe have led to mid- or long-term symptoms, the WHO found, impacting up to 17 million people. The study also found women are more likely to develop Long COVID.
-
National numbers, September 25
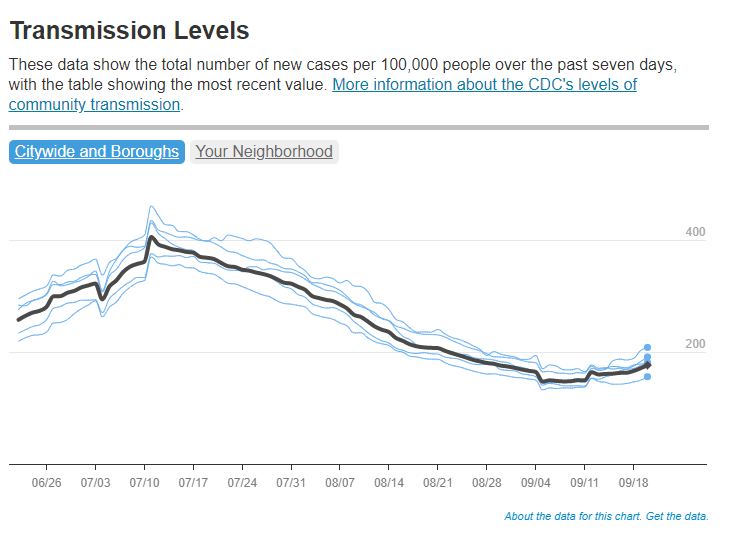
Reported COVID-19 cases in New York City have started going up slightly in the last few days, according to the city health department. In the past week (September 17 through 23), the U.S. reported about 380,000 new COVID-19 cases, according to the CDC. This amounts to:
- An average of 54,000 new cases each day
- 116 total new cases for every 100,000 Americans
- 11% fewer new cases than last week (September 10-16)
In the past week, the U.S. also reported about 28,000 new COVID-19 patients admitted to hospitals. This amounts to:
- An average of 4,000 new admissions each day
- 8.5 total admissions for every 100,000 Americans
- 10% fewer new admissions than last week
Additionally, the U.S. reported:
- 2,400 new COVID-19 deaths (350 per day)
- 83% of new cases are caused by Omicron BA.5; 12% by BA.4.6; 2% by BF.7; 1% by BA.2.75 (as of September 24)
- An average of 300,000 vaccinations per day
Nationally, official COVID-19 case counts continue to decline: reported cases are down about 11% last week compared to the prior week, while new COVID-19 patients in hospitals are down 10%. But signals from wastewater and variants suggest a fall surge may be starting soon.
“Currently, most of the country is reporting moderate to high SARS-CoV-2 levels in wastewater,” CDC officials noted in this Friday’s COVID Data Tracker Weekly Review. For almost 20% of sites, these coronavirus levels are the highest seen since December 2021, the CDC reports. About half the wastewater sites in the CDC’s network are reporting an increase in coronavirus levels and half are reporting a decrease.
Notably, many of the wastewater sites reporting increased coronavirus spread are in the Northeast, a region that’s also a hotspot for Omicron subvariants BA.2.75 and BF.7. BF.7, a new sublineage that evolved from BA.5, is particularly worth watching (more on that below). Overall, the U.S.’s variant composition is slowly shifting from BA.5 to these two subvariants, along with BA.4.6—which caused 12% of new cases nationwide in the week ending September 24.
According to the latest Community Profile Report, states reporting significant increases in cases from week to week include Nevada, California, New Hampshire, Kentucky, Massachusetts, New Jersey, New York, and Oregon. In New York City—often a bellwether for new surges—cases have started to tick up slightly, according to the city’s health department, after a long (and slow) decline from July’s summer peak.
Meanwhile, other common respiratory viruses might make a comeback this fall, report Dr. Katelyn Jetelina and Dr. Caitlin Rivers in a joint issue of their newsletters. Data so far on the flu, RSV, rhinovirus, and other viruses we consider part of a normal fall season suggest that children in the U.S. might have a particularly virus-heavy fall and winter—putting more pressure on the healthcare system.
One of the best ways to protect yourself from COVID-19 this fall is by receiving one of the new, Omicron-specific booster shots. According to the CDC, about 4.4 million Americans have received one so far, as of September 21. The new shots have brought our vaccine administration counts to over 300,000 new doses given a day, but that still pales in comparison to the millions administered daily during the spring 2021 campaign.
I received my own booster on Friday at a NYC Health + Hospitals site. Unlike my primary series doses, for which my girlfriend and I had to wait in long lines with hundreds of other New Yorkers, we got our new shots in a small, hard-to-find room tucked away in a small corner of a south Brooklyn hospital campus. This vaccination campaign seems to be almost an afterthought when it deserves primetime attention.